Esophageal cancer is a malignant condition arising from the lining of the esophagus, the muscular tube that connects the throat to the stomach. This cancer is particularly aggressive, often diagnosed in advanced stages due to the subtlety of early symptoms. Its global significance stems from its high mortality rate and its ranking among the leading causes of cancer-related deaths worldwide.
Despite its relatively low incidence compared to other cancers, it remains a major health concern due to its typically late diagnosis and aggressive progression. According to the American Cancer Society, in 2024, approximately 22,370 new cases of esophageal cancer were diagnosed in the United States, with about 16,130 deaths resulting from the disease.
This article will explore the symptoms, causes, stages, and treatment options for esophageal cancer. We will also present the latest data on incidence and mortality rates, underscoring the urgent need for early diagnosis and innovative therapies.
What Are the Symptoms of Esophageal Cancer?
Esophageal cancer often presents with symptoms that may initially appear mild or mimic common gastrointestinal conditions, contributing to delays in diagnosis. By the time significant symptoms emerge, the disease has often progressed to advanced stages, reducing treatment options and survival rates.
Common Symptoms and Their Association with Late Diagnosis
- Difficulty Swallowing (Dysphagia): According to an article by the American Cancer Society , dysphagia is the most prevalent symptom of esophageal cancer, reported in over 90% of patients. This symptom typically begins with difficulty swallowing solid foods and progresses to liquids as the tumor enlarges, leading to significant esophageal obstruction. This progression often indicates advanced disease at the time of diagnosis.
- Unintended Weight Loss: According to an article by the Mayo Clinic , approximately 50% of individuals with esophageal cancer experience significant weight loss. This is primarily due to reduced food intake resulting from dysphagia and the cancer’s metabolic effects. Such weight loss is frequently observed in the later stages of the disease.
- Chest Pain or Discomfort: Patients may experience chest pain, pressure, or burning sensations, which are often mistaken for heartburn or gastroesophageal reflux disease (GERD).
What Are the Early Signs of Esophageal Cancer?
Esophageal cancer often presents with subtle, non-specific symptoms in its early stages, complicating timely diagnosis. Common initial symptoms include:
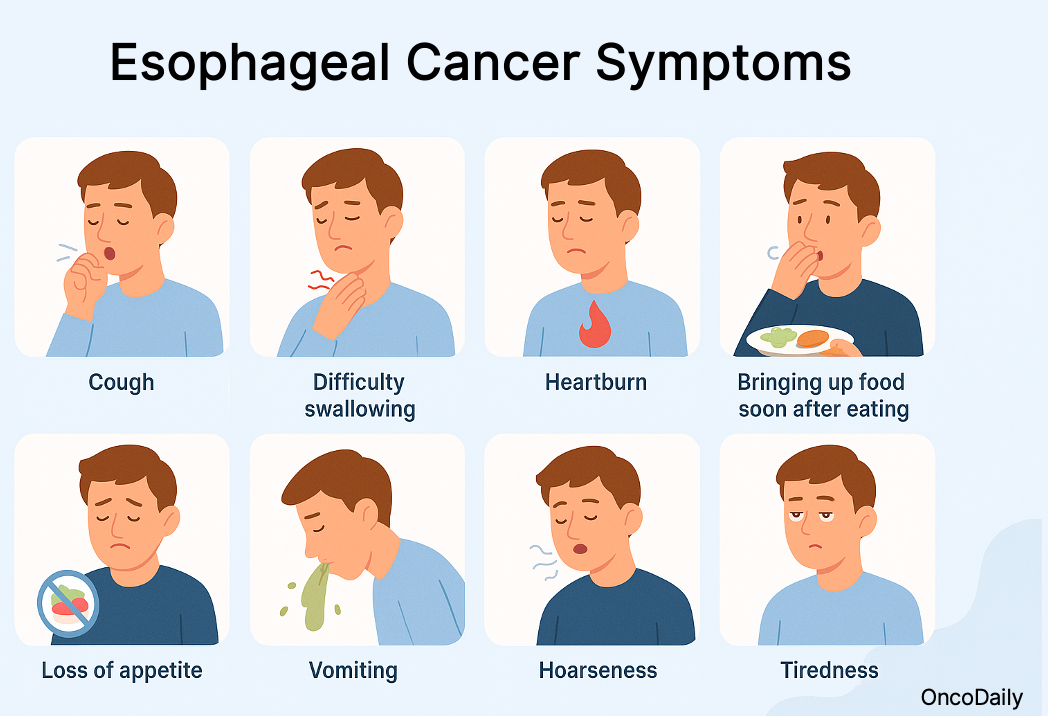
- Heartburn (Acid Reflux):According to an article published by Cancer Research UK, persistent heartburn or acid reflux is frequently reported by patients in the early stages of esophageal cancer. This symptom is often mistaken for gastroesophageal reflux disease (GERD), leading to delays in seeking appropriate medical evaluation.
- Chronic Cough: According to an article by the National Cancer Institute, a persistent cough that does not resolve over time can be an early indicator of esophageal cancer. This symptom is commonly attributed to respiratory conditions, which may result in misdiagnosis.
- Hoarseness: According to an article by Moffitt Cancer Center, changes in voice, such as hoarseness, occur when a tumor affects the recurrent laryngeal nerve. This symptom is often overlooked or attributed to benign causes, contributing to diagnostic delays.
Challenges in Early Detection
- Asymptomatic Early Stages: The disease often progresses without noticeable symptoms until it reaches an advanced stage, making early diagnosis difficult.
- Non-Specific Symptoms: When symptoms do occur, they are often non-specific and can be attributed to less severe conditions, leading to misdiagnosis or delayed diagnosis.
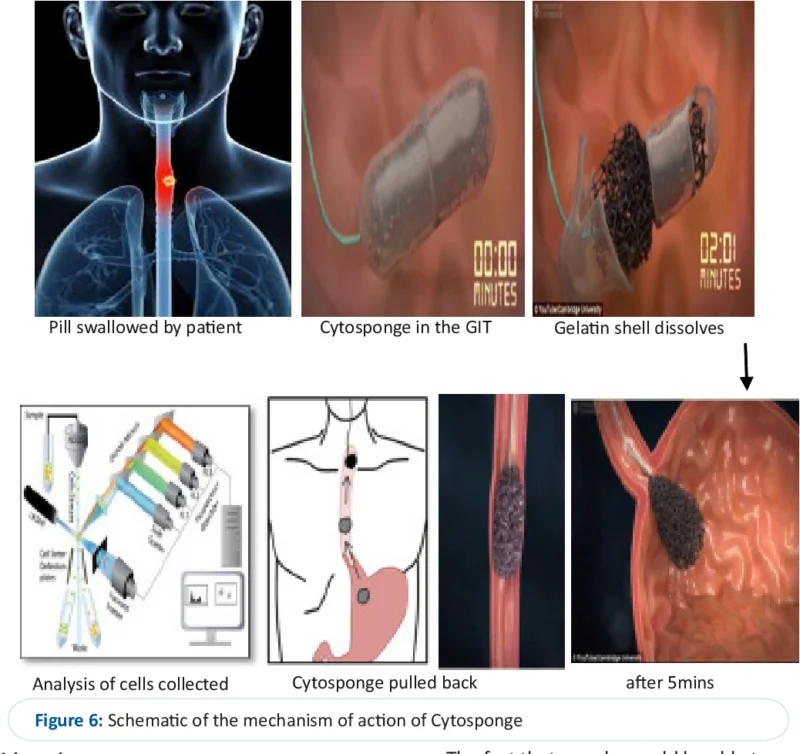
- Lack of Routine Screening: There are currently no widespread, non-invasive, and cost-effective screening tools for esophageal cancer, hindering early detection efforts.
What are the Causes and Risk Factors for Esophageal Cancer?
Esophageal cancer arises from a combination of medical conditions, lifestyle choices, genetic factors, and other contributing elements. Understanding these risk factors is crucial for prevention and early detection.
Medical Conditions
- Gastroesophageal Reflux Disease (GERD): Chronic acid reflux, known as GERD, can damage the esophageal lining, leading to changes that increase cancer risk. Persistent reflux is a significant risk factor for esophageal adenocarcinoma.
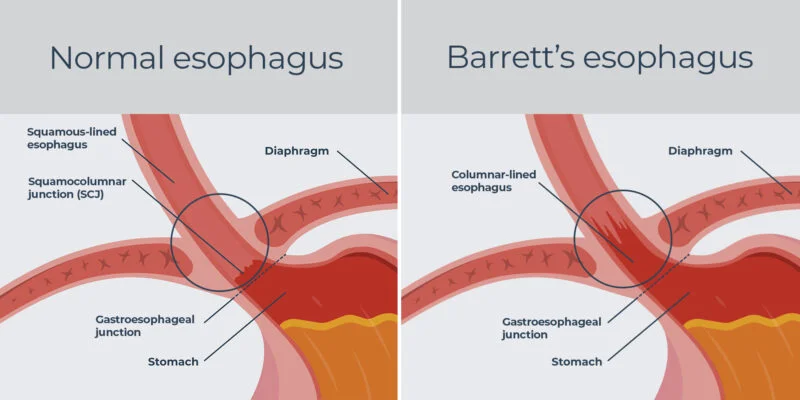
- Barrett’s Esophagus: This condition involves the replacement of normal esophageal lining with tissue similar to the intestinal lining, often due to prolonged GERD. Individuals with Barrett’s esophagus have a higher risk of developing esophageal adenocarcinoma.
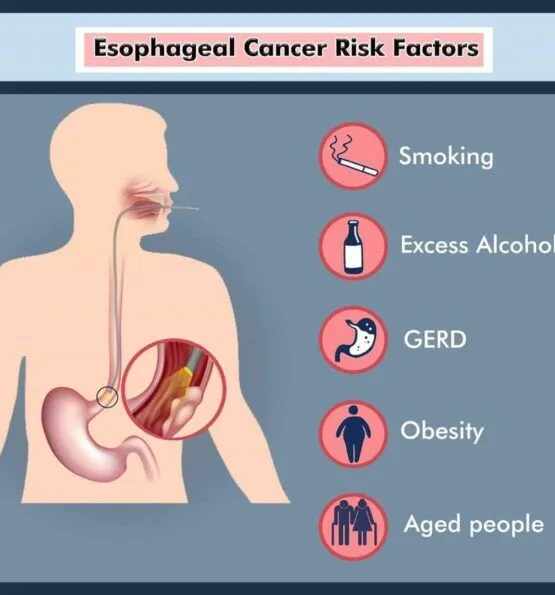
Risk Factors
- Smoking: Tobacco use damages the esophageal lining, significantly increasing the risk of esophageal squamous cell carcinoma.
- Alcohol Consumption: Chronic alcohol intake, especially when combined with smoking, elevates the risk of esophageal cancer.
- Genetic Predispositions : According to a study by Minyi Lee et al., published in Gastroenterology in 2023, pathogenic germline mutations in cancer-predisposing genes were identified in 9% of individuals with Barrett’s esophagus who progressed to adenocarcinoma, compared to 2.7% in non-progressors.
- Obesity: Visceral obesity is linked to an increased risk of esophageal adenocarcinoma, potentially due to factors like insulin resistance and changes in the esophageal microenvironment.
- Diet: Diets low in fruits and vegetables may elevate esophageal cancer risk, while certain dietary patterns can act as protective measures.
What Are the Types of Esophageal Cancer?
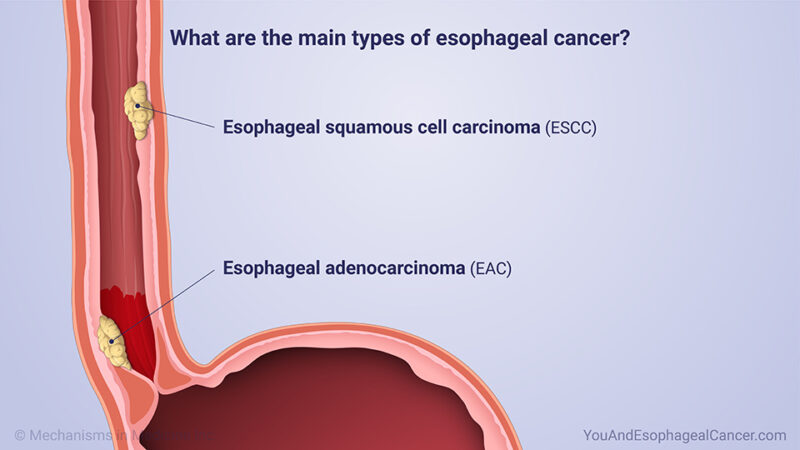
Esophageal cancer primarily manifests as two distinct histological types: adenocarcinoma and squamous cell carcinoma. Each type has unique characteristics, risk factors, and geographical prevalence, contributing to differences in disease management and outcomes. Adenocarcinoma accounts for about 60%–70% of cases in Western countries, typically occurring in the lower esophagus, while squamous cell carcinoma represents the majority of cases worldwide, especially in Asia and Africa, affecting the mid-to-upper esophagus. The occurrence of both histological types within a single tumor, such as adenosquamous carcinoma, is extremely rare, with a reported incidence of less than 1% of all esophageal cancers.
Esophageal Adenocarcinoma
- Chronic GERD is the primary driver of Barrett’s esophagus and a leading contributor to adenocarcinoma
- Obesity, especially central obesity, worsens GERD by increasing intra-abdominal pressure, leading to acid reflux and esophageal irritation.
- Smoking accelerates cellular damage, further increasing the risk of malignancy.
- Dietary habits that include high consumption of processed foods and low intake of fruits and vegetables contribute to oxidative stress and inflammation, promoting carcinogenesis.
- Demographics play a significant role, with adenocarcinoma being far more prevalent in white males, particularly in Western populations.
Squamous Cell Carcinoma
- Smoking: Tobacco use is one of the leading causes of squamous cell carcinoma. The carcinogens in tobacco cause cellular damage to the esophageal lining, significantly increasing cancer risk.
- Alcohol Consumption: Alcohol has a synergistic effect with smoking, meaning that the combined use of tobacco and alcohol multiplies the risk far beyond that of either factor alone. Chronic alcohol use irritates the esophagus and interferes with its ability to repair damaged tissues.
- Dietary Habits: Deficiencies in selenium, zinc, and other essential nutrients have been associated with an increased risk of ESCC. Diets low in fruits and vegetables fail to provide antioxidants and other protective factors that prevent cellular damage.
- Consumption of Extremely Hot Beverages: Drinking very hot liquids (above 65°C/149°F) repeatedly damages the esophageal lining over time, increasing the risk of cancer. This practice is particularly common in regions where tea or other beverages are consumed at scalding temperatures.
- Environmental Exposures: Exposure to certain toxins or chemical irritants in food, water, or occupational settings further contributes to the risk of developing ESCC.
- Achalasia: This motility disorder, which impairs the esophagus’s ability to move food into the stomach, leads to prolonged stasis and irritation, increasing the likelihood of squamous cell carcinoma.
How Is Esophageal Cancer Diagnosed?
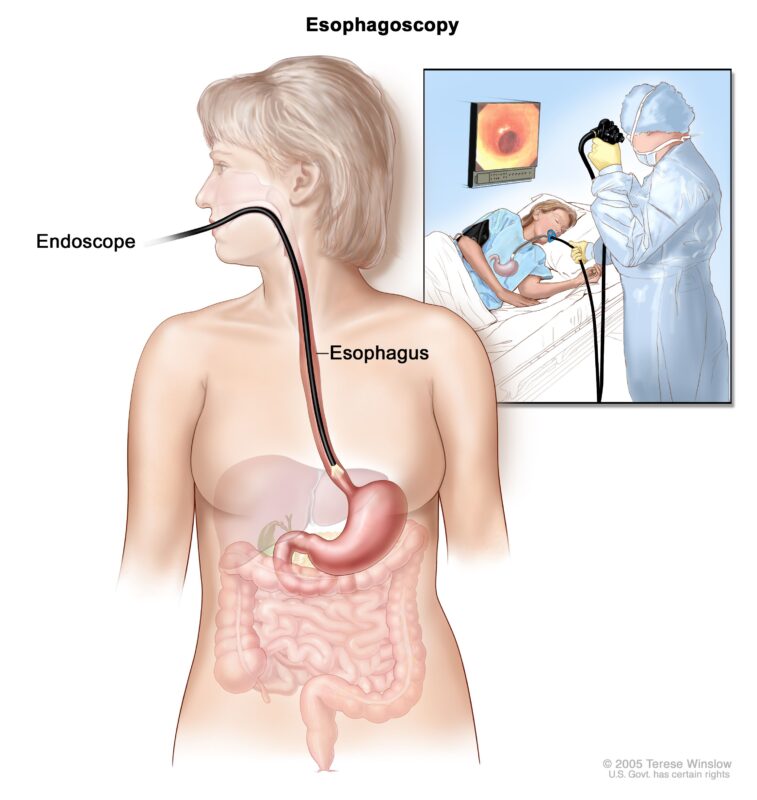
Once cancer is confirmed, imaging studies such as computed tomography (CT) and magnetic resonance imaging (MRI) are essential for determining the tumor’s extent, assessing lymph node involvement, and identifying distant metastases.
- CT Scans provide detailed cross-sectional images of the chest, abdomen, and pelvis, helping to stage the cancer and evaluate its spread to surrounding tissues or organs.
- MRI is particularly useful for soft tissue evaluation, providing high-resolution images of the esophagus and nearby structures.
What Are the Treatment Options for Esophageal Cancer?
The treatment of esophageal cancer requires a multidisciplinary approach, integrating a combination of surgery, chemotherapy, radiation therapy, and emerging treatments such as targeted therapy and immunotherapy. This aggressive malignancy demands tailored strategies based on the cancer’s stage, location, and the patient’s overall health, as each factor plays a critical role in determining the most effective treatment plan.For patients diagnosed at early stages, localized disease offers the best opportunity for successful intervention, often with curative intent. Procedures such as esophagectomy, combined with neoadjuvant or adjuvant chemotherapy, form the backbone of early-stage treatment. However, for those with locally advanced or metastatic disease, systemic therapies like chemotherapy and radiation therapy are essential to control tumor growth, alleviate symptoms, and extend survival.
Advancements in targeted therapies and immunotherapy have revolutionized the treatment landscape for esophageal cancer, offering new hope for patients with advanced disease. Therapies like trastuzumab, which targets HER2-positive tumors, and immune checkpoint inhibitors, such as nivolumab, have demonstrated significant improvements in patient outcomes when used in combination with standard treatments.
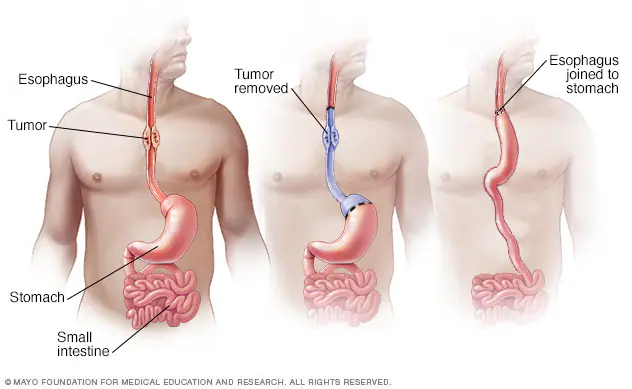
Surgical Options for Esophageal Cancer
Esophagectomy, the surgical removal of all or part of the esophagus, is a primary treatment for early-stage esophageal cancer. This procedure aims to excise cancerous tissues and reconstruct the digestive tract to restore swallowing function. This could be achieved by several techniques including.
- Transthoracic Esophagectomy (Ivor Lewis Procedure): Involves abdominal and thoracic incisions to remove the esophagus and part of the stomach, followed by reconstruction.
- Transhiatal Esophagectomy: Utilizes abdominal and neck incisions, avoiding the chest cavity, to remove the esophagus and connect the stomach to the remaining esophagus.
- Minimally Invasive Esophagectomy (MIE): Employs laparoscopic instruments through small incisions, potentially reducing recovery time and complications.
According to a study by Peng Zhang et al., published in the Journal of Cardiothoracic Surgery, involving 1,023 patients undergoing minimally invasive McKeown esophagectomy, favorable long-term survival rates were reported, with overall survival at 1, 3, and 5 years being 83.2%, 61.9%, and 55.9%, respectively. Recovery from esophagectomy is extensive, often requiring a hospital stay of one to two weeks and several months of rehabilitation. Patients may initially receive nutrition via a feeding tube and gradually reintroduce oral intake.
Potential risks include
- Respiratory Complications: Pneumonia is common post-surgery.
- Anastomotic Leak: Leakage at the surgical connection between the esophagus and stomach.
- Infection and Bleeding: Risks inherent to major surgeries.
- Digestive Issues: Challenges such as acid reflux, difficulty swallowing, and changes in bowel habits.
Chemotherapy and Combined Chemoradiotherapy for Esophageal Cancer
Chemotherapy remains a cornerstone in the treatment of esophageal cancer, particularly for locally advanced or metastatic disease, where surgical interventions are limited. It can be used alone or in combination with other treatments such as radiation, surgery, and, increasingly, immunotherapy. Significant advancements in drug combinations and treatment regimens have improved outcomes in both esophageal adenocarcinoma (EAC) and esophageal squamous cell carcinoma (ESCC) (Sheikh et al., Cancers, 2024).
For patients with advanced esophageal adenocarcinoma, studies have demonstrated the superior efficacy of the FLOT regimen (fluorouracil, leucovorin, oxaliplatin, and docetaxel). Compared to the widely used CROSS protocol (carboplatin and paclitaxel combined with radiation), FLOT has emerged as the preferred preoperative treatment option. In a 2024 trial, the FLOT regimen significantly improved median overall survival to 66 months compared to 37 months with CROSS, with a 5-year survival rate of 50.6% versus 38.7%, respectively (Hoeppner et al., 2024).
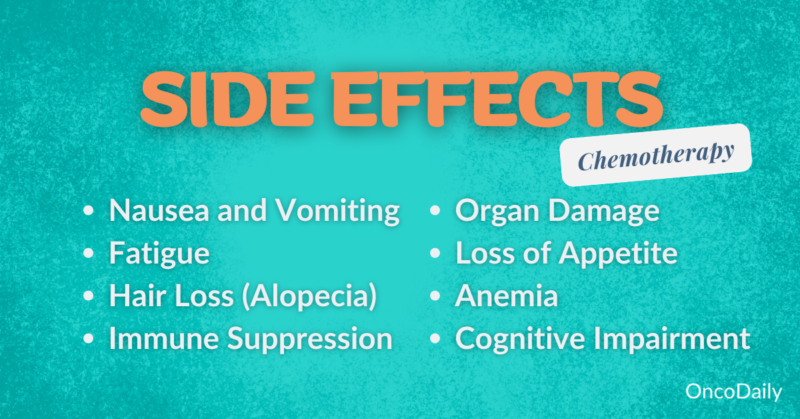
Learn More About Side Effects of Chemotherapy vs Immunotherapy: Special Article by OncoDaily
In addition to chemotherapy, combined chemotherapy and radiation therapy (chemoradiotherapy) plays a pivotal role, particularly in locally advanced esophageal cancer. Neoadjuvant chemoradiotherapy, delivered before surgery, has become the standard of care for resectable tumors. The widely cited CROSS trial demonstrated that chemoradiotherapy using carboplatin and paclitaxel with concurrent radiation (41.4 Gy) significantly improves overall survival compared to surgery alone, with a median survival of 49 months versus 24 months, respectively (Sheikh et al., Cancers, 2024).
For patients with unresectable ESCC, definitive chemoradiotherapy, which combines platinum-based chemotherapy (e.g., cisplatin and 5-fluorouracil) with radiation, remains the primary curative treatment option. This approach provides tumor control and symptom relief, achieving median survival rates of 12–18 months in advanced cases. ESCC, being more sensitive to radiation therapy compared to EAC, shows better response rates to this combined modality (Sheikh et al., Cancers, 2024).
Learn More About Side Effects of Radiotherapy: Special Article by OncoDaily
In recent years, emerging evidence has supported the integration of immunotherapy with chemotherapy for both subtypes, improving survival rates and tolerability. Immunotherapy agents, such as PD-1 inhibitors like nivolumab, have shown substantial benefits when added to chemoradiotherapy, particularly for patients with residual disease after neoadjuvant treatment (Sheikh et al., Cancers, 2024). This combined approach represents a major advancement, moving toward personalized, multimodal treatment strategies tailored to the specific molecular and clinical characteristics of the tumor.
What Are the Stages of Esophageal Cancer?
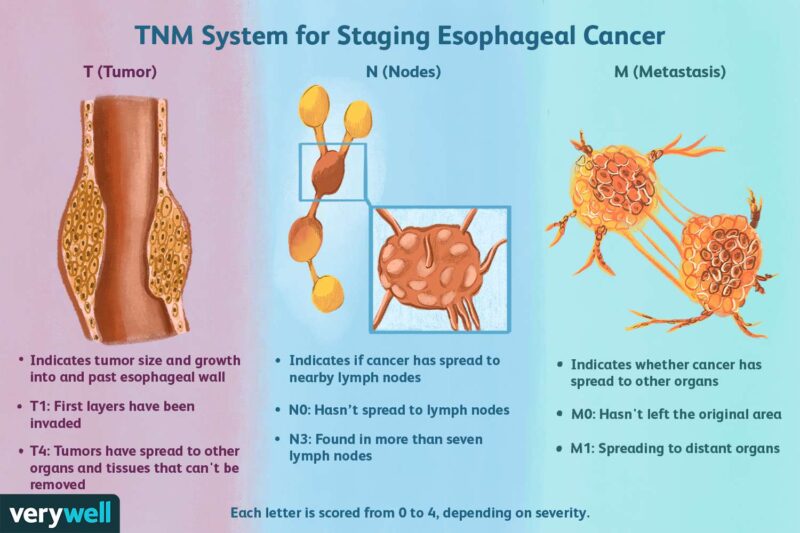
Stage I
Stage II
Stage III
Stage IV
- Palliative Chemotherapy is the mainstay treatment, helping to slow disease progression and relieve symptoms.
- Targeted Therapy and Immunotherapy are utilized for tumors with specific biomarkers. For example, trastuzumab is used for HER2-positive tumors, while immune checkpoint inhibitors like nivolumab target PD-L1-expressing cancers.
- Supportive Care plays a critical role in managing pain, swallowing difficulties, and other symptoms associated with advanced disease.
After Treatment: What to Expect
Recovering from esophageal cancer treatment involves navigating physical side effects, adopting dietary modifications, and addressing psychological challenges. Understanding these aspects and implementing expert-recommended lifestyle adjustments can significantly enhance the quality of life during and after recovery.
Post-treatment, patients may experience various physical side effects, including:
- Fatigue: A common aftermath of surgery, chemotherapy, or radiation therapy, leading to decreased energy levels.
- Swallowing Difficulties (Dysphagia): Treatment can cause scarring or narrowing of the esophagus, making swallowing challenging.
- Digestive Issues: Symptoms such as acid reflux, nausea, and changes in bowel habits are prevalent.
- Neuropathy: Some chemotherapy agents may result in nerve damage, causing numbness or tingling in extremities.
Nutrition plays a pivotal role in recovery. Patients often need to adjust their diets to accommodate changes in digestion and swallowing:
- Small, Frequent Meals: Consuming smaller portions multiple times a day can aid digestion and prevent discomfort.
- Soft or Liquid Diets: Easier-to-swallow foods can help manage dysphagia.
- High-Protein, High-Calorie Foods: To maintain weight and promote healing, incorporating nutrient-dense foods is beneficial.
- Avoiding Irritants: Steering clear of spicy, acidic, or hard-to-digest foods can reduce gastrointestinal discomfort.
The emotional toll of cancer treatment is significant:
- Anxiety and Depression: Concerns about recurrence and coping with physical changes can lead to mental health challenges.
- Body Image Issues: Surgical scars and changes in physical appearance may affect self-esteem.
- Cognitive Changes: Some patients report difficulties with memory and concentration, often referred to as “chemo brain.”
How Is Esophageal Cancer Prognosis Determined?
The prognosis for esophageal cancer is influenced by several factors, including tumor stage at diagnosis, patient age, and overall health. Understanding these elements is crucial for tailoring treatment strategies and providing accurate survival estimates.
Tumor Stage at Diagnosis
- Localized Stage: Cancer is confined to the esophagus, with a 5-year relative survival rate of approximately 49%.
- Regional Stage: Cancer has spread to nearby lymph nodes or tissues, reducing the 5-year relative survival rate to about 28%.
- Distant Stage: Cancer has metastasized to distant organs, with a 5-year relative survival rate of around 6%.
Patient Age and Overall Health
- Age: Younger patients often have better survival rates, potentially due to fewer comorbidities and a greater ability to tolerate aggressive treatments.
- Overall Health: Patients with good performance status and without significant comorbid conditions are more likely to undergo and recover from intensive treatments, leading to improved outcomes.
Latest Advancements in Esophageal, Gastroesophageal Junction (GEJ), and Gastric Cancers
Recent breakthroughs in gastroesophageal and GEJ cancers highlight significant progress in novel treatments and clinical trials. The TOPGEAR Phase III trial tested perioperative chemoradiotherapy (CRT) alongside standard chemotherapy (FLOT) for gastric and esophageal cancer, with findings suggesting no overall survival (OS) benefit for CRT.

TOPGEAR trial presented at ESMO 2024 by T. Leong
In HER2-positive disease, KEYNOTE-811 emphasized pembrolizumab’s efficacy when combined with trastuzumab and chemotherapy, especially in PD-L1 CPS ≥1 patients. Meanwhile, the Phase 1b/2 DESTINY-Gastric03 trial showcased promising results for trastuzumab-deruxtecan (T-DXd) combined with fluoropyrimidines and pembrolizumab, positioning T-DXd as a robust first-line option. These studies underscore a shift toward biomarker-driven therapies and tailored multimodality treatment approaches, advancing survival outcomes and patient-centric care strategies in upper GI cancers.
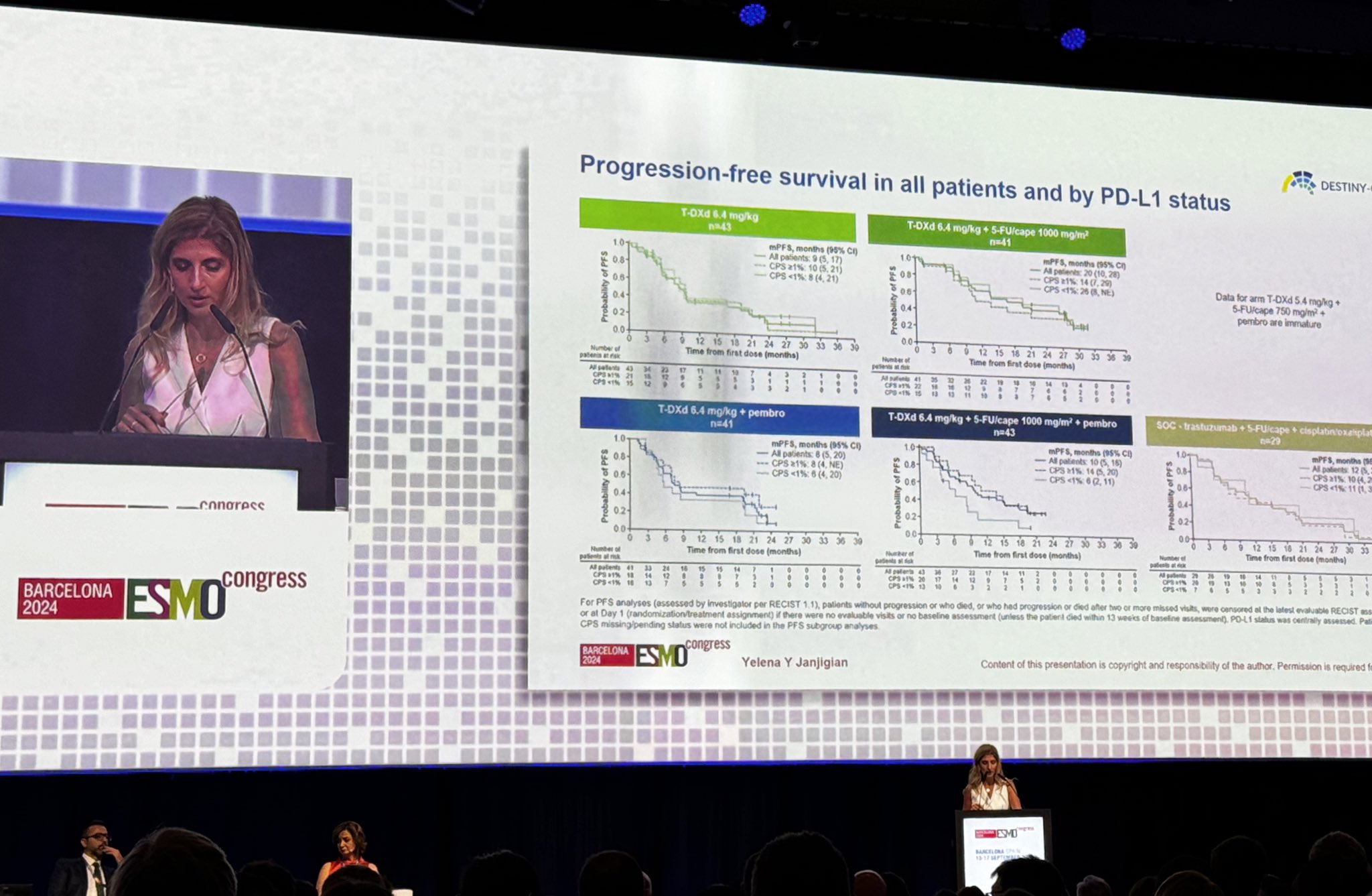
DestinyGastric03 trial presented at ESMO2024 by Y.Janjigian
Minimally invasive esophagectomy (MIE), particularly the McKeown procedure, has demonstrated favorable long-term survival rates. A study by Zhang et al. (2023) reported 5-year overall survival rates of 49.5% for patients undergoing the McKeown approach.
According to the article “Efficacy of Immune Checkpoint Inhibitors Combined with Chemotherapy in Advanced Esophageal Squamous Cell Carcinoma: A Meta-Analysis” by Wang et al. (2022), the addition of immune checkpoint inhibitors (ICIs) to chemotherapy has shown significant benefits in the treatment of advanced esophageal squamous cell carcinoma (ESCC). The analysis, which included data from 3,163 patients across multiple clinical trials, revealed that combining ICIs with chemotherapy reduced the risk of death by 32% compared to chemotherapy alone.
Targeted Therapy
Recent advances in molecular-targeted therapy have identified Claudin18.2 (CLDN18.2) as a promising target in gastric, gastroesophageal junction (GEJ), and esophageal cancers. CLDN18.2, typically restricted to gastric mucosal cells, becomes exposed across the tumor cell surface in malignancies, enabling it as a target for monoclonal antibody therapies. Zolbetuximab, a first-in-class monoclonal antibody, binds to CLDN18.2 and induces tumor cell destruction via antibody-dependent and complement-dependent cytotoxicity.
The SPOTLIGHT and GLOW Phase III trials demonstrated that zolbetuximab combined with platinum-fluoropyrimidine regimens significantly improved progression-free survival (PFS) and overall survival (OS) in CLDN18.2-positive, HER2-negative gastric or GEJ cancers. This success paves the way for its use in esophageal adenocarcinomas, particularly in patients with low PD-L1 CPS (<5).
Additionally, ongoing studies are exploring CLDN18.2-targeted therapies like antibody-drug conjugates (ADCs), bispecific T-cell engagers (BiTEs), and CAR-T therapies, offering new hope for refractory esophageal cancers. In HER2-positive esophageal adenocarcinoma, the ToGA trial established trastuzumab plus chemotherapy as the standard first-line treatment, improving OS to 13.8 months (HR: 0.74) compared to chemotherapy alone. Emerging strategies combining HER2-targeted agents with checkpoint inhibitors like pembrolizumab are also under investigation, aiming to further enhance survival outcomes.
How to Live with Esophageal Cancer?
Living with esophageal cancer is challenging, but with the right strategies, patients can navigate diagnosis, treatment, and recovery more effectively. Early on, building a strong care team and learning about the condition helps patients feel in control. Seeking a second opinion and understanding treatment options can provide confidence in the journey ahead.
During treatment, swallowing difficulties often require dietary changes. Soft, moist, or pureed foods and small, frequent meals are key, while avoiding acidic and spicy foods helps minimize discomfort. For those struggling with nutrition, feeding tubes may provide temporary support. Coping emotionally is just as important. Therapy, support groups, and mindfulness practices like yoga or meditation can ease anxiety. Managing physical side effects, such as fatigue or reflux, often involves medication or lifestyle adjustments, such as sleeping with an elevated head.
Recovery is gradual. Many patients benefit from light exercises to rebuild strength, speech therapy to address swallowing issues, and ongoing dietary modifications. Regular follow-ups with the care team are essential to monitor for recurrence.
Can Esophageal Cancer Be Prevented?
Preventing esophageal cancer starts with understanding risk factors and making proactive changes. Regular screenings, like endoscopies, are vital for people with chronic acid reflux (GERD), Barrett’s esophagus, or a family history of the disease. These screenings can catch early changes in the esophageal lining before cancer develops.
Quitting smoking is one of the most impactful steps, as smoking damages the esophagus and significantly increases cancer risk. Managing GERD is equally crucial—avoiding large meals, elevating the head during sleep, and using prescribed medications can help control acid reflux and prevent long-term complications.
A healthy lifestyle also plays a big role. Eating a diet rich in fruits, vegetables, and whole grains, maintaining a healthy weight, and limiting alcohol consumption all contribute to lowering the risk. Experts recommend a Mediterranean-style diet for its anti-inflammatory benefits.
By combining regular medical care with healthy habits, individuals can significantly reduce their risk of esophageal cancer and support long-term well-being.
You Can Also Read About Gastric Cancer: Special Article by OncoDaily

FAQ
What is esophageal cancer?
Esophageal cancer is a malignancy that develops in the lining of the esophagus, the muscular tube connecting the throat to the stomach. It is one of the more aggressive forms of cancer.
How common is esophageal cancer?
Esophageal cancer accounts for approximately 1% of all cancer diagnoses in the United States, with an estimated 20,640 new cases in 2024. Globally, it is more prevalent in certain regions like East Asia and sub-Saharan Africa.
What are the early symptoms of esophageal cancer?
Early symptoms include difficulty swallowing (dysphagia), persistent heartburn, unexplained weight loss, and chest discomfort. These symptoms often appear in later stages, making early detection challenging.
What causes esophageal cancer?
Risk factors include chronic gastroesophageal reflux disease (GERD), smoking, excessive alcohol consumption, obesity, and conditions like Barrett’s esophagus. Genetic predispositions can also play a role.
How is esophageal cancer staged?
Esophageal cancer is staged from Stage I (localized cancer) to Stage IV (cancer that has metastasized to distant organs). Staging determines the extent of the disease and guides treatment options.
What treatment options are available for esophageal cancer?
Treatment includes surgery, chemotherapy, radiation therapy, immunotherapy, and targeted therapy. The choice depends on the cancer stage, type, and patient health.
What are the survival rates for esophageal cancer?
Survival rates vary by stage. The 5-year survival rate is approximately 48% for localized cancer, 25%-35% for regional cancer, and less than 5% for metastatic cancer.
Can esophageal cancer be prevented?
Prevention strategies include managing acid reflux, quitting smoking, reducing alcohol intake, maintaining a healthy weight, and eating a diet rich in fruits and vegetables. Regular screenings are advised for high-risk individuals.
What is Barrett’s esophagus, and how is it related to esophageal cancer?
Barrett’s esophagus is a condition where the lining of the esophagus changes due to chronic acid reflux. It increases the risk of developing esophageal adenocarcinoma, a type of esophageal cancer.
How does esophageal cancer impact quality of life during and after treatment?
Esophageal cancer and its treatments can affect swallowing, nutrition, and overall well-being. Supportive care, including dietary changes, therapy, and rehabilitation, can help improve quality of life.
Written by Toma Oganezova, MD