Introduction
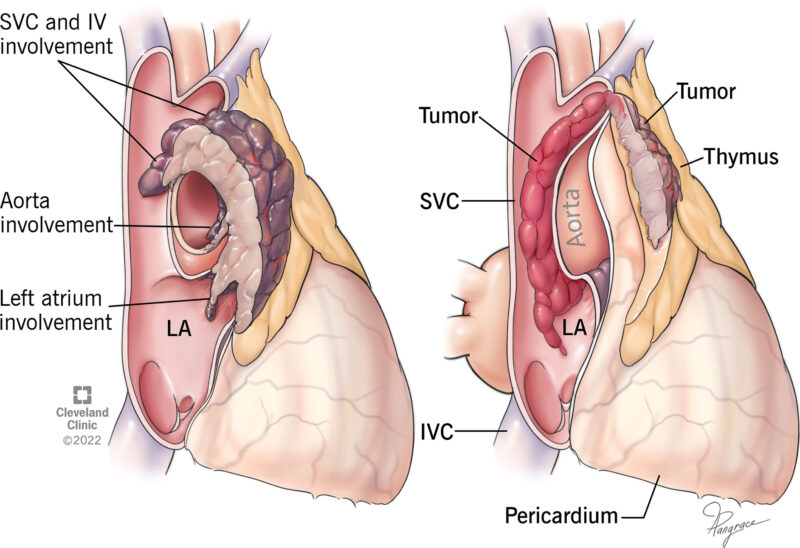
The thymus is a small, butterfly-shaped organ located in the upper chest, just behind the sternum. It is part of the lymphatic system and plays a crucial role in the body’s immune system. The thymus is vital for T-lymphocyte maturation and selection, a type of white blood cell that helps fight infections and diseases.
In infants and young children, the thymus is relatively large and actively produces T-cells. As a person grows older, the thymus gradually becomes smaller and less active, but it continues to play a role in the immune system throughout life.
A thymoma is a type of tumor that develops in the thymus gland. It is a rare cancer that can occur at any age, but it is most commonly diagnosed in adults between the ages of 40 and 60. Thymomas are generally slow-growing tumors, and they can be either non-cancerous (benign) or cancerous (malignant). Thymic carcinoma, on the other hand, is a more aggressive and rarer form of cancer that originates in the thymus.
This image is taken from frontiersin.org
Causes and risk factors
The exact cause of thymomas is not well understood, but researchers believe that a combination of genetic and environmental factors may play a role. There are no known specific risk factors for developing a thymoma, but certain conditions have been associated with an increased risk:
- Autoimmune disorders: Many autoimmune diseases are associated with Thymoma, such as myasthenia gravis, pure red cell aplasia, or hypogammaglobulinemia
- Age: Thymomas are more common in older adults, with the highest incidence occurring between the ages of 40 and 60.
- Gender: Thymomas are slightly more common in women than in men.
- Ethnicity: In the United States, thymomas are more common in Asian Americans and Pacific Islanders than in other ethnic groups.
It is important to note that having one or more of these risk factors does not necessarily mean that a person will develop a thymoma. Additionally, some people with thymomas may not have any known risk factors.
Symptoms
Many people with thymomas do not experience any symptoms, especially in the early stages of the disease. When symptoms do occur, they may include:
Due to the tumor compressing the airways
- Persistent cough
- Shortness of breath
Due to tumor mass effect in the mediastinum
- Chest pain or discomfort
Possibly due to accompanying Myasthenia Gravis
- Muscle weakness
- Fatigue
- Drooping eyelids
- Double vision
Can be a sign of esophageal compression or muscle weakness
- Difficulty swallowing
Due to Superior Vena Cava Syndrome
- Swelling in the face, neck, or upper body
If accompanied with pure red blood cell aplasia (low erythrocytes)
- Skin paleness
- Weakness
- Decreased energy
Diagnosis
If a thymoma is suspected, several tests may be performed to confirm the diagnosis and determine the extent of the disease:
- Imaging tests: Chest X-rays, computed tomography (CT) scans, magnetic resonance imaging (MRI), and positron emission tomography (PET) scans can help detect the presence of a tumor in the thymus and determine its size and location.
- Biopsy: In some cases, a small sample of the tumor may be removed (biopsy) and examined under a microscope to confirm the diagnosis of a thymoma.
- Blood tests: Blood tests may be performed to check for autoimmune disorders or other conditions associated with thymomas.
This informative video is taken from Medical Centric
Prevention
There are no known specific ways to prevent thymomas, as the exact cause is not well understood. However, maintaining a healthy lifestyle and avoiding known risk factors for cancer, such as smoking and excessive alcohol consumption, may help reduce the overall risk of developing various types of cancer, including thymomas.
Prognosis
The prognosis (outlook) for people with thymomas depends on several factors, including the type and stage of the tumor, the person’s age and overall health, and the effectiveness of the treatment. In general, the earlier a thymoma is detected and treated, the better the prognosis.
Non-cancerous (benign) thymomas have a better prognosis than cancerous (malignant) thymomas. Malignant thymomas that have not spread beyond the thymus gland (localized) also have a better prognosis than those that have spread to other parts of the body (metastatic).
Treatment and Side Effects of Thymomas
Surgery
Surgical Removal of the Tumor (Thymectomy)
Thymectomy is the surgical removal of the thymus gland, which is often necessary when thymoma, a type of cancer, is present. There are several approaches to thymectomy:
- Traditional Open Surgery: This involves a large chest incision, typically through a median sternotomy, which is a vertical cut down the middle of the chest. This method provides excellent access to the thymus but results in a longer recovery period and more noticeable scarring.
- Minimally Invasive Surgery: Techniques such as robotic-assisted surgery or video-assisted thoracoscopic surgery (VATS) use smaller incisions. These methods result in less pain, fewer scars, and quicker recovery times. Robotic-assisted thymectomy, for example, uses advanced technology to provide a high-definition, three-dimensional view of the surgical site and allows for precise movements.
Side Effects of Surgery
- Pain and Discomfort: Common but manageable with pain medications.
- Temporary Side Effects: These can include difficulty swallowing or speaking and shortness of breath.
- Complications: Rare but can include bleeding, infection, or damage to nearby organs.
- Long-Term Effects: There may be potential impacts on immune function, though these effects are not fully understood.
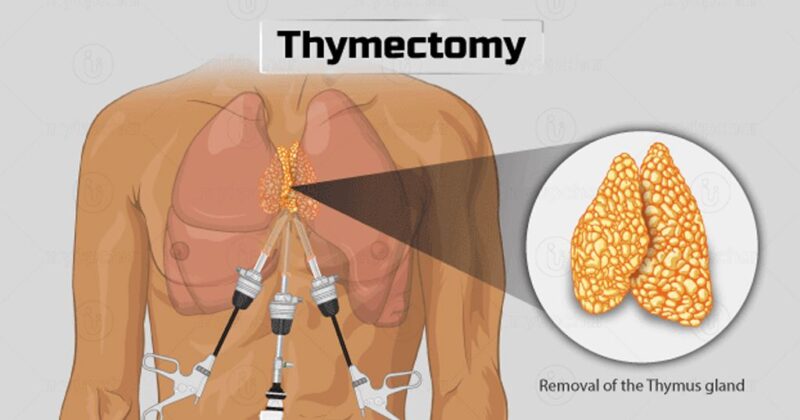
This image is taken from drshashithoracicsurgeon.com
Radiation Therapy
Using High-Energy Beams to Destroy Cancer Cells
Radiation therapy uses high-energy radiation to kill cancer cells. It can be used in various ways to treat thymomas and thymic carcinomas:
- External Beam Radiation Therapy (EBRT): This is the most common type, using X-rays from a machine outside the body.
- Three-Dimensional Conformal Radiation Therapy (3D-CRT): This technique allows precise targeting to reduce exposure to healthy tissue.
- Intensity-Modulated Radiation Therapy (IMRT): This method uses varying intensities of radiation from different angles.
- Image-Guided Radiation Therapy (IGRT): Real-time images guide the delivery of radiation.
- Stereotactic Radiosurgery: Delivers high-dose radiation to a precise area.
- Brachytherapy: Involves placing radioactive implants near the tumor.
Side Effects of Radiation Therapy
- Short-Term: Fatigue, skin irritation, nausea, vomiting, and mouth or throat sores.
- Long-Term: Potential lung damage, increased risk of heart disease, and secondary cancers.
Chemotherapy
Using Anti-Cancer Drugs to Kill Cancer Cells
Chemotherapy involves using drugs to kill cancer cells and is often used for advanced thymomas or thymic carcinomas. Common chemotherapy agents include cisplatin, doxorubicin, cyclophosphamide, etoposide, carboplatin, and paclitaxel.
Side Effects of Chemotherapy
- Hair Loss: Usually temporary.
- Mouth Sores: Can make eating and drinking uncomfortable.
- Loss of Appetite: Can lead to weight loss.
- Nausea and Vomiting: Manageable with medications.
- Fatigue and Weakness: Common but usually temporary.
- Blood Cell Counts: Increased risk of infection, easy bruising, and anemia.
Targeted Therapy
Targeting Specific Molecules Involved in Cancer Growth
Targeted therapy focuses on specific molecules involved in the growth and spread of cancer cells. Examples of targeted therapy drugs include sunitinib, lenvatinib, everolimus, and milciclib.
Side Effects of Targeted Therapy
- Fatigue: Common.
- Diarrhea: Can lead to dehydration.
- Nausea and Vomiting: Often milder than with chemotherapy.
- Anorexia: Loss of appetite.
- Hematological Effects: Low blood cell counts, increasing the risk of infection and bleeding.
Supportive Care
Managing Symptoms and Improving Quality of Life
Supportive care aims to manage symptoms and improve the quality of life for patients undergoing treatment for thymomas. This includes:
- Pain Management: Using medications and therapies to manage pain.
- Nutritional Support: Ensuring adequate nutrition to maintain strength and health.
- Emotional and Psychological Support: Counseling and support groups to help cope with the emotional impact of cancer.
- Physical Therapy: Maintaining strength and mobility through exercises and physical activities.
Side Effects of Supportive Care
Generally, supportive care does not cause side effects but helps manage those from primary treatments. Open communication with the healthcare team is essential for effective management.
Newest options and ongoing trials
Researchers are continuously working to develop new and more effective treatments for thymomas. Some of the newest options and ongoing clinical trials for thymomas include:
- Immunotherapy: Immunotherapy is a type of treatment that helps the body’s immune system recognize and attack cancer cells. Several immunotherapy drugs, such as checkpoint inhibitors and monoclonal antibodies, are being studied for the treatment of thymomas.
- Targeted therapy: Researchers are investigating new targeted therapies that target specific molecular pathways involved in the growth and spread of thymomas.
- Combination therapies: Clinical trials are exploring the use of different combinations of treatments, such as surgery, radiation therapy, chemotherapy, and targeted therapies, to improve outcomes for people with thymomas.
- Minimally invasive surgical techniques: Advances in minimally invasive surgical techniques, such as robotic-assisted surgery, may offer improved outcomes and faster recovery times for people undergoing surgery for thymomas.
It is important to note that clinical trials are ongoing, and the availability and eligibility criteria for these trials may vary. Patients should discuss with their healthcare team if participating in a clinical trial is an appropriate option for their specific situation.
More information about ongoing clinical trials can be found on clinicaltrials.gov
Patient survivorship
Emotional and Psychological Challenges
Emotional Well-Being
The emotional toll of cancer diagnosis and treatment can be profound. Survivors often face anxiety, depression, and fear of recurrence. The psychological impact can be long-lasting, requiring ongoing support and counseling.
- Anxiety and Depression: The fear of cancer returning can cause significant anxiety and depression. Survivors may benefit from counseling, support groups, and mental health services to manage these feelings.
- Post-Traumatic Stress: Some patients may experience post-traumatic stress disorder (PTSD) due to the trauma of their cancer journey. This can manifest as flashbacks, severe anxiety, and emotional numbness.
Social and Practical Challenges
Social Isolation
Cancer treatment can lead to social isolation due to prolonged hospital stays, weakened immune systems, and the need to avoid infections. This isolation can be exacerbated by the physical and emotional toll of the disease.
- Support Networks: Building and maintaining a strong support network is crucial. Family, friends, and support groups can provide emotional and practical support.
- Work and Financial Challenges: Returning to work can be challenging due to ongoing fatigue and physical limitations. Financial stress from medical bills and loss of income can also be significant.
This informative video is taken from cancerVme.
Resources
- National Cancer Institute – cancer.gov
- Treatment of Advanced Thymoma and Thymic Carcinoma- PubMed
- Survivorship: Late Effects After Radiation for Thymoma. | OncoLink.org
- Systemic treatments for thymic tumors: a narrative review – Mediastinum
- Estimated Risk of Radiation-Induced Cancer after Thymoma Treatments with Proton- or X-ray Beams – PubMed
- Targeted Therapy for Advanced Thymic Tumors – PubMed
- American Society of Clinical Oncology – cancer.net
- Thymoma: Results of treatment and role of radiotherapy – PubMed
- American Cancer Society – cancer.org
- Immunotherapy for Management of Thymic Epithelial Tumors
- Complications and efficacy of transsternal thymectomy in Myasthenia Gravis – PubMed
- Oncodaily – News, Insights, stories and everything about Cancer