Cancer remains a persistent global health challenge, with substantial variation in both incidence and mortality across countries and regions. According to recent data, from the GLOBOCAN 2022 report by the International Agency for Research on Cancer (IARC) approximately 20 million new cancer cases were recorded worldwide in 2022, with projections estimating a nearly 77% increase by 2050, reaching over 35 million cases annually.
This escalating burden is attributed to population growth, aging, and shifts in exposure to risk factors such as tobacco use, alcohol consumption, obesity, and environmental pollution. Notably, disparities in cancer rates are observed across the Human Development Index (HDI) spectrum: while very high-HDI countries currently report the highest age-standardized incidence rates e.g., Australia with over 460 cases per 100,000 persons low-HDI countries face a disproportionately rapid rise in cases and cancer-related deaths projected to nearly triple by mid-century. These variations are further complicated by differences in healthcare infrastructure, cancer detection, reporting accuracy, and access to treatment.

This article presents a detailed examination of countries reporting the highest and lowest cancer incidence and mortality rates, with an emphasis on the epidemiological, socioeconomic, and environmental determinants underpinning these disparities. It also addresses methodological challenges in comparing global cancer statistics. Readers will gain insight into the complex interplay of factors influencing cancer epidemiology worldwide and the implications for prioritized health policies aimed at cancer prevention, early detection, and equitable management to mitigate this growing global burden.
How Cancer Rates Vary Dramatically Across Countries: Exploring Global Disparities
Cancer incidence rates exhibit profound and complex variations across countries worldwide, influenced by a multitude of interrelated factors. As of recent 2025 data, Australia records the highest age-standardized cancer incidence rate globally, at approximately 452 cases per 100,000 population. This places it ahead of other high-incidence countries such as New Zealand and Ireland, which report rates of about 423 and 373 per 100,000, respectively. The United States also ranks notably high, with an incidence rate around 362 per 100,000, followed by European nations such as Denmark, the Netherlands, Belgium, and France, all reporting rates above 340 per 100,000.
These elevated rates in high-income countries largely reflect advanced healthcare systems capable of comprehensive cancer detection and reporting, alongside lifestyle factors prevalent in these societies, including tobacco use, obesity, dietary patterns, and environmental exposures like pollution and UV radiation. Moreover, aging populations in these countries contribute significantly to higher cancer incidence, as cancer risk increases sharply with age.
Conversely, many low-income countries, particularly in regions like West Africa and the Himalayas, report markedly lower cancer incidence rates. For example, Niger exhibits an age-standardized rate below 80 per 100,000, with similar low levels seen in the Gambia, Nepal, Bhutan, and several other nations. However, these lower figures often mask a more troubling reality.
Limited access to healthcare infrastructure, deficient cancer registries, and barriers to early diagnosis contribute to substantial underreporting and underdiagnosis of cancer cases in these regions. In some instances, cultural factors and lower health literacy further delay detection and treatment, leading not only to fewer recorded cases but also to higher mortality rates relative to incidence. For example, certain cancers like cervical cancer remain prevalent and deadly in low-income settings due to inadequate screening and vaccination coverage.
Genetic predispositions also play a role in the geographical variation of cancer types and rates. For instance, prostate cancer incidence shows large variability, with historically lower rates in East Asia but increasing trends possibly linked to Westernized lifestyles. Similarly, infections such as hepatitis B and human papillomavirus (HPV) contribute heavily to liver and cervical cancers, respectively, particularly in parts of Africa and Asia.
Understanding these disparities involves recognizing the interplay of socioeconomic development, healthcare system capacity, environmental risk factors, lifestyle behaviors, and genetics. Addressing the global cancer burden requires comprehensive strategies tailored to the context of each country, improving access to prevention, early detection, and treatment services. Enhanced cancer registry systems and epidemiological research are critical to accurately measuring and combating cancer worldwide.
Countries with the Highest Cancer Incidence: Why Rates Could Worsen in the Coming Years
Cancer incidence rates in high human development index (HDI) countries are among the highest globally, driven primarily by aging populations and a combination of lifestyle and environmental risk factors. Countries such as Australia, New Zealand, Denmark, the United States, and France currently report elevated age-standardized cancer incidence rates, ranging from about 339 to 745 cases per 100,000 people in 2022. These high rates are influenced by widespread tobacco use, obesity, alcohol consumption, and environmental pollution, all of which contribute significantly to cancer risk.
Projections indicate a worrying trend: by 2050, global cancer cases are expected to rise by approximately 77%, reaching over 35 million new cases annually. This surge will be partially driven by demographic factors, such as an aging global population and continued population growth. Moreover, increasing exposure to cancer risk factors particularly in low- and middle-HDI countries will accelerate the rise in cancer incidence. For example, India and China show projected cancer rate increases of roughly 142% and 99%, respectively, by 2050. Even in high-HDI nations like Australia and the U.S., projected increases of 40-42% in cancer incidence reflect ongoing lifestyle and environmental challenges.
Key risk factors remain consistent across these countries: tobacco use is still the leading preventable cause of many cancers, followed closely by obesity, alcohol consumption, and exposure to air pollution. Air pollution is classified as a human carcinogen for lung cancer, and its role in cancer incidences is growing alongside urbanization and industrial emissions.
Without comprehensive and aggressive prevention strategies, the expanding global cancer burden will substantially strain healthcare systems worldwide, increasing demands on cancer detection, treatment, and care infrastructure.
Countries with the Highest Cancer Incidence: Why Rates Could Worsen in the Coming Years
- Overview of Countries with Highest Current Cancer Incidence Rates (2022)
- Key Risk Factors Driving Cancer Incidence in High HDI Countries
- Projected Increase in Cancer Rates by 2050 and Implications
- The Impact of Aging Populations and Lifestyle Changes on Cancer Incidence
- Strategies for Prevention and Healthcare System Preparedness
- Cancer Incidence Rates per 100,000 Population: Current vs. Projected (Selected Countries)
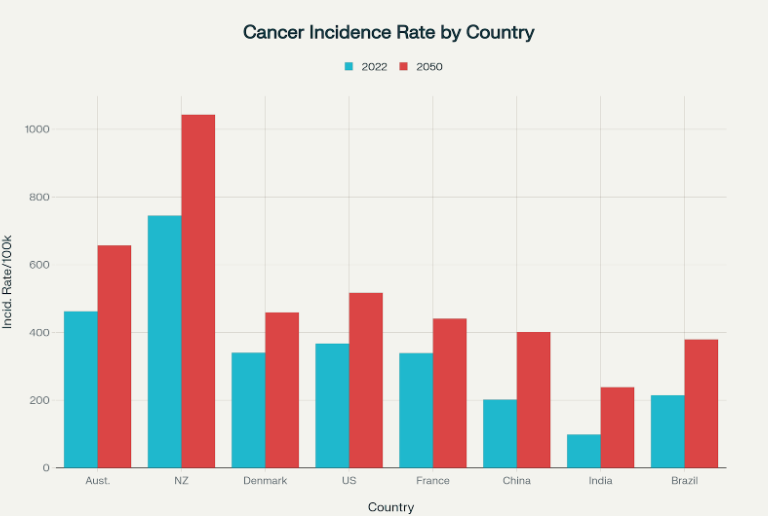
Cancer incidence rates per 100,000 population in 2022 and projected for 2050 in selected high and middle HDI countries.
This chart illustrates the current (2022) and projected (2050) cancer incidence rates per 100,000 population in selected high and middle HDI countries. For example:
- Australia’s cancer incidence is projected to rise from about 462 to 657 cases per 100,000.
- New Zealand faces a significant increase from around 745 to over 1,040 per 100,000.
- The United States is expected to see an increase from 367 to 517 cases per 100,000.
- Middle-HDI countries like India and China also show steep relative increases, reflecting expanding cancer risks with socio-economic development.
Solutions and Strategies to Combat the Growing Cancer Burden Globally
Addressing the escalating global cancer burden requires an integrated, multisectoral approach that spans prevention, early detection, treatment, and system strengthening. Tobacco control remains paramount, as tobacco use is the single largest preventable cause of cancer worldwide. Comprehensive policies including taxation, smoking bans, and public education have proven effective in reducing smoking rates. Vaccination programs against oncogenic viruses such as hepatitis B and human papillomavirus (HPV) are critical preventive measures that can significantly reduce liver and cervical cancers, respectively. Additionally, public health campaigns promoting healthy lifestyle behaviors such as balanced diets, regular physical activity, reduced alcohol consumption, and obesity prevention can avert up to 40% of cancer cases by addressing modifiable risk factors.
Beyond prevention, enhancing early detection through widespread screening programs and improving diagnostic infrastructure is essential, especially in low- and middle-income countries where delayed diagnosis leads to higher mortality rates. Equitable access to quality cancer treatment including surgery, radiotherapy, and chemotherapy must be prioritized to reduce disparities in outcomes. Strengthening healthcare infrastructure involves investing in trained workforce, cancer registries, and supply chains for essential medicines and technologies. National cancer control plans, adequately funded and supported by governments, provide structured frameworks for these efforts. Furthermore, fostering international collaboration facilitates knowledge exchange, technology transfer, and coordinated research efforts, which are vital to implement effective cancer control strategies globally and mitigate future cancer-related morbidity and mortality.
Insights from One Health Studies: Bridging Animal and Human Cancer Research for Innovative Treatments
The One Health approach to cancer research underscores the interconnectedness of human, animal, and environmental health, fostering innovative breakthroughs by bridging these domains. Multiple countries, including the United States, Australia, and European nations, have been pioneers in this integrated effort, leveraging comparative oncology especially studies involving naturally occurring cancers in pet dogs to accelerate advancements in cancer treatment for both humans and animals.
Comparative oncology uses canine cancer trials as valuable models due to the genetic, histological, and biological similarities between canine and human tumors. For example, countries like the U.S. have developed major research programs, such as the Flint Animal Cancer Center’s “One Cure” initiative, which has conducted over 35 clinical trials since 2019 investigating treatments for osteosarcoma, lymphoma, and other cancers. These trials enable faster evaluation of novel therapies in a fraction of the time needed for human trials because of dogs’ shorter lifespans. This approach has already yielded significant advancements; immune modulators like liposome-encapsulated muramyl tripeptide (L-MTP-PE) first tested in dogs were subsequently shown to delay metastasis in human osteosarcoma patients.
Furthermore, recent studies at institutions such as the University of California, Davis, have administered human cytokines (e.g., IL-15) to dogs with cancers like osteosarcoma and melanoma, showing promising therapeutic responses without adverse side effects. These advances are informing new human immunotherapies, while the flexibility in veterinary treatments allows for rapid experimental drug application that would be more restricted in human clinical trials.
The collaborative One Health research has led to a stabilization and improvement in survival outcomes for canine cancer patients, with ongoing genomic analyses of over 2,000 tumor-bearing dogs revealing prognostic concordance with human cancers. This opens the door for precision medicine approaches benefiting both species. Countries engaged in One Health cancer studies are increasingly establishing frameworks such as the One Health Joint Plan of Action adopted by global health organizations including WHO and FAO to institutionalize multisectoral collaboration and capacity building.
Beyond treatment, comparative oncology offers insights into tumor suppression mechanisms across species, helping to understand natural cancer resistance as seen in large or long-lived animals, which may inspire novel prevention and therapeutic strategies for humans.
In sum, the One Health approach exemplifies how cross-species cancer research conducted across countries fosters accelerated discovery, improves treatment outcomes, and enriches our understanding of cancer biology. This integrated model not only expedites translational research but also contributes to global cancer control efforts in a way that benefits humans, animals, and ecosystems alike.
You Can Also Read How Aging Populations Are Reshaping Global Cancer Trends or The Silent Shift by OncoDaily

Emerging Breakthroughs in Cancer Diagnosis and Treatment Offer New Hope
Emerging breakthroughs in cancer diagnosis and treatment in 2025 are rapidly transforming the oncology landscape through the integration of precision medicine, artificial intelligence (AI), and innovative therapeutic approaches. Precision oncology is advancing with next-generation mutant-specific drugs targeting previously “undruggable” oncogenes such as KRAS variants, which are common in difficult-to-treat cancers like pancreatic cancer.
Therapeutic cancer vaccines and T-cell receptor therapies are also nearing clinical implementation, offering new ways to enhance immune system targeting of tumors. AI and machine learning are playing a pivotal role by analyzing tumor microenvironments and genetic data to predict treatment responses early, particularly refining the identification of biomarkers critical for immunotherapy efficacy. Tools like DeepHRD, an AI-powered system, now detect specific tumor deficiencies with up to three times greater accuracy than traditional genomic tests, guiding more effective targeted therapies such as PARP inhibitors.
Furthermore, multi-omics integration combining genomics, proteomics, metabolomics, and other molecular data enables comprehensive patient profiles that enhance personalized treatment strategies. Cell and gene therapies, including CAR-T treatments, are transitioning from experimental to mainstream care, showing promising outcomes beyond blood cancers, now extending to solid tumors. Emerging digital health technologies and real-time genomics also contribute to early cancer detection and individualized treatment, while AI streamlines clinical trials and optimizes treatment planning.
In conclusion, the global variation in cancer incidence reflects a complex interplay of demographic, lifestyle, environmental, and healthcare factors. While high-HDI countries exhibit some of the highest cancer rates due to advanced detection and risk exposures, many low-HDI countries face underdiagnosis and rising cancer burdens fueled by changing risk profiles. Projected increases in cancer cases worldwide underscore the urgent need for comprehensive prevention, early detection, and equitable treatment strategies. Integrating innovative research approaches and leveraging emerging technologies offer promising pathways to improve outcomes. Ultimately, coordinated global efforts are essential to reduce cancer disparities and alleviate its growing health and societal impacts across all nations.
Written by Marine Marashlian
FAQ
What are the most common types of cancer worldwide?
Breast, lung, colorectal (colon and rectum), and prostate cancers are the most common globally, with lung cancer being the leading cause of cancer death.
Why do cancer rates vary so much between countries?
Cancer rates differ due to variations in lifestyle, environmental exposures, healthcare infrastructure, genetics, and accuracy of cancer detection and reporting systems.
Which countries have the highest cancer incidence rates?
High human development index (HDI) countries like Australia, New Zealand, the United States, and several European nations report some of the highest cancer rates, often above 400 cases per 100,000 population.
Can cancer rates worsen in the coming years?
Yes, global cancer cases are projected to increase by about 77% by 2050, driven by aging populations, population growth, and increasing exposure to risk factors like tobacco, obesity, and pollution.
What are the main risk factors for cancer?
Tobacco use, high body mass index (obesity), alcohol consumption, poor diet, lack of physical activity, infections (e.g., HPV, hepatitis), and environmental pollutants are major contributors.
How much cancer can be prevented through lifestyle changes?
About 30-40% of cancers could potentially be prevented by quitting smoking, maintaining a healthy weight, eating a balanced diet, being active, and avoiding harmful alcohol use.
Why do some low-income countries report lower cancer rates?
Underreporting due to limited healthcare access, lack of cancer registries, late diagnosis, and cultural barriers often mask the true cancer burden in low-HDI countries.
What advances are helping improve cancer detection and treatment?
Precision oncology, immunotherapies, personalized cancer vaccines, and artificial intelligence for early detection are key emerging innovations improving cancer care worldwide.
How does the One Health approach contribute to cancer research?
By integrating human, animal, and environmental health research, One Health propels faster discovery of treatments through comparative oncology, particularly using canine cancer models.
What is being done globally to reduce cancer disparities?
Multisectoral strategies including tobacco control, vaccination programs (e.g., HPV), strengthened healthcare infrastructure, and international collaborations aim to improve prevention, diagnosis, and treatment.


