During the general session, Prof. Jessica Leung, speaking from the perspective of a practicing radiologist, focused her remarks on how breast imaging language and nodal anatomy are being operationalized in the newest BI-RADS update—particularly for ultrasound-driven regional nodal assessment. She positioned the talk as practical: how radiologists describe nodes, how that language maps to surgical planning, and where advanced imaging adds value versus cost.
BI-RADS 2025
BI-RADS as a Shared Language—and Why the 2025 Manual Matters
Prof. Leung framed BI-RADS as a standardized communication system designed to improve interpretation and consistency across teams. As she put it, “a bar stands for worst imaging, reflecting a data system,” emphasizing that standardized language supports “proper interpretation” and “communication care.”
She also highlighted the recency of the update: “This is the B 2025 manual… and that just came out. December 1st, 2025.” In her view, the newest version reflects deeper alignment with contemporary nodal staging frameworks and more detailed guidance for regional nodal basins.
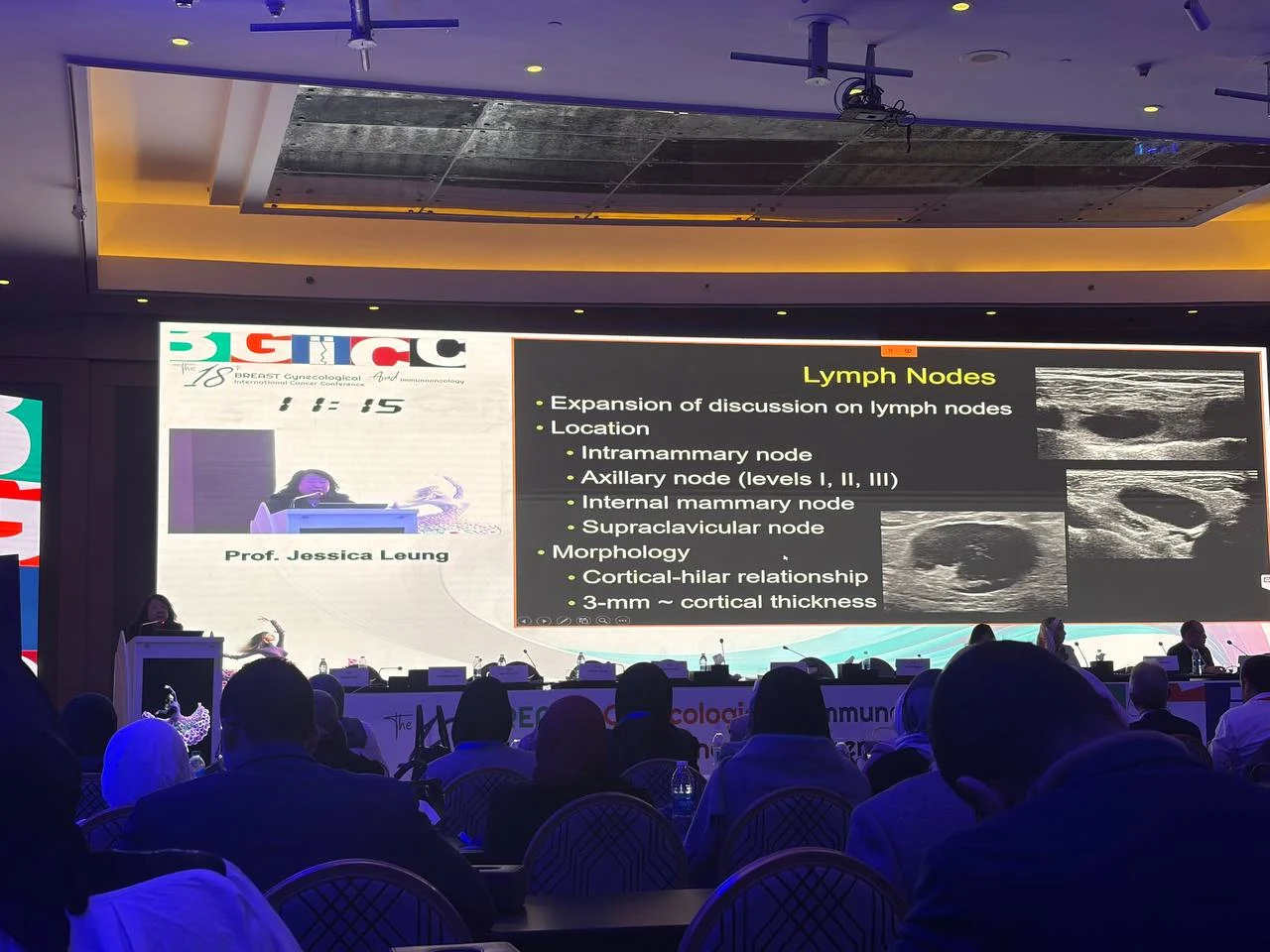
Regional Nodal Anatomy: The Axilla in Levels—and Beyond
A central portion of the talk reviewed the axillary nodal map in three levels, anchored to anatomic landmarks used across imaging and surgery. She described a layered approach—level I, II, and III—organized around the pectoralis musculature and the relative position of nodal groups.
Beyond the axilla, she brought attention to additional basins that matter in breast cancer staging and treatment planning, including the internal mammary chain and the supraclavicular region, noting that these regions must be clearly defined and consistently assessed when clinically relevant.

BI-RADS 2025
Ultrasound as the “Workhorse” for Nodal Assessment
Prof. Leung repeatedly emphasized ultrasound as the core modality for nodal evaluation, portraying it as the most actionable tool for day-to-day staging decisions and biopsy triage. In her discussion of morphology, she returned to the importance of cortical assessment and practical thresholds that trigger concern.
She also described the workflow logic of scanning: starting with key axillary levels and extending the protocol depending on clinical suspicion and available visualization—particularly when higher-risk territories are implicated.
MRI: Useful, But Not a Universal Answer
While acknowledging MRI’s role, she clearly separated its strengths from ultrasound’s direct utility. Her framing was pragmatic: MRI can add information, but it also brings scheduling complexity, cost, and variable incremental yield.
To support this, she referenced contemporary practice-based evidence suggesting that the number of additional nodal findings detected by MRI after ultrasound may be modest in many scenarios, describing an incremental detection figure and reinforcing that more imaging does not always translate into meaningful changes for every patient.
Morphology Over Size: Why “Bigger” Is Not Always “Worse”
Prof. Leung stressed that nodal size alone can mislead. She argued that morphology—especially the cortex and hilum appearance—drives suspicion more reliably than diameter. She illustrated how benign enlarged nodes can exist, while smaller nodes may still be pathologic depending on cortical configuration and loss of normal architecture.
In practical terms, she discussed recognizable patterns radiologists use every day: preserved fatty hilum versus abnormal hilum, cortical thickening patterns, and more globally suspicious shapes that shift management toward targeted sampling.
BI-RADS 2025
A “Goldilocks” Principle in the Axilla: Not Too Much, Not Too Little
One of the memorable teaching moments in the talk was her use of a “Goldilocks” analogy—explicitly connecting the story framework to modern surgical de-escalation and imaging-guided precision. The message was clear: the goal is a balanced approach to nodal management—accurate staging and control, while avoiding unnecessary morbidity.
She linked this to the concept of targeted axillary dissection, describing it as a strategy that relies on imaging localization, landmark-based planning, and selective removal of key nodes rather than maximal dissection in all patients.
When Patterns Break: Nodal “Skipping” and Why It Matters
Toward the end, Prof. Leung challenged the classic assumption of orderly nodal spread (“first to level I, then onward”) and discussed that real-world dissemination does not always follow textbook progression. She described this as clinically meaningful because it influences where radiologists look, what they sample, and how confidently staging can be inferred from a single basin.
Conclusion
Prof. Jessica Leung’s message was method-driven and clinically anchored: BI-RADS 2025 is not just a document update, but an opportunity to tighten how the imaging team communicates nodal findings, standardize anatomic language, and apply morphology-first decision rules—especially in ultrasound-based regional staging. She reinforced that advanced imaging can help, but value depends on incremental yield and clinical consequence, and that modern axillary management increasingly rewards a “just right” balance guided by imaging precision.