On the first day of the Breast Global International Cancer Conference (BGICC), during the plenary session, Prof. Giuseppe Curigliano, ESMO President-Elect (2025–2026), delivered a biologically focused lecture entitled “Breaking the Cycle: Overcoming CDK4/6 Inhibitor Resistance in ER+/HER2-Negative Metastatic Breast Cancer.”
At the outset, Prof. Curigliano clearly outlined the structure of his presentation. He first reviewed the clinical deployment of CDK4/6 inhibitors, then discussed translational approaches to study resistance, and finally focused on the key biological mechanisms that drive resistance in hormone receptor–positive, HER2-negative breast cancer.

Clinical Deployment of CDK4/6 Inhibitors
CDK4/6 inhibitors combined with endocrine therapy are widely used in HR+/HER2– metastatic breast cancer and have demonstrated consistent clinical benefit across randomized studies. Despite these advances, disease progression occurs in most patients, emphasizing the need to better understand the biological drivers of resistance.
Translational Approaches to Resistance
The lecture highlighted the role of translational research in characterizing resistance. Tissue biopsies allow assessment of receptor status and tumor heterogeneity, while liquid biopsy approaches enable non-invasive monitoring of molecular evolution over time. High concordance between tissue and plasma sequencing has been reported for several key genomic alterations, supporting the use of circulating tumor DNA analyses at progression.
Key Biological Mechanisms of Resistance
Resistance to CDK4/6 inhibitors does not arise from a single alteration, but rather from recurrent biological programsthat allow tumor cells to bypass cell-cycle arrest and maintain proliferation. As emphasized in the lecture, these mechanisms reflect adaptive cell-cycle reprogramming and activation of parallel oncogenic signaling pathways, highlighting the biological plasticity of hormone receptor–positive breast cancer.
Loss of RB1 function was highlighted as the most definitive and clinically relevant resistance mechanism to CDK4/6 inhibition. Because CDK4/6 inhibitors rely on an intact RB pathway to induce cell-cycle arrest, RB1 loss is associated with lack of meaningful benefit from continued CDK4/6 inhibition. The slides illustrated that RB1 dysfunction is predominantly detected in resistant disease and can arise through different biological routes. Across datasets, increasing resistance correlates with progressively reduced RB protein expression, reinforcing the central role of RB pathway disruption in treatment failure.
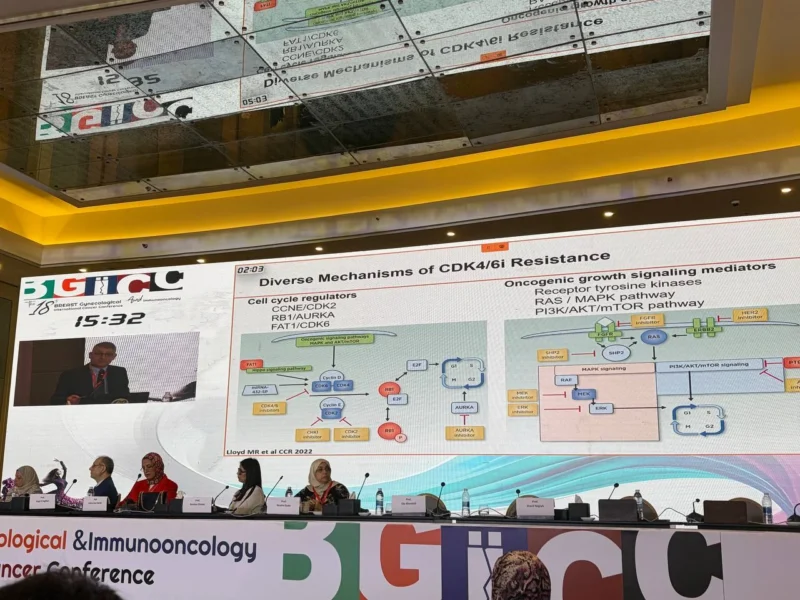
Beyond RB1 loss, the lecture focused on adaptive mechanisms that allow restoration of cell-cycle progression despite CDK4/6 blockade. One such mechanism is upregulation of CDK6, which enables tumor cells to bypass CDK4 inhibition and continue proliferating. The slides highlighted that CDK6 overexpression can be driven by upstream regulatory alterations affecting cell-cycle control pathways. This mechanism represents an inducible form of resistance that emerges under therapeutic pressure rather than a primary genetic event.
Another important bypass mechanism discussed was activation of the cyclin E–CDK2 axis. Increased CCNE1 activity supports CDK2-dependent cell-cycle progression and has been associated with reduced benefit from CDK4/6 inhibition in translational analyses. This pathway provides an alternative route for tumor proliferation when CDK4/6 activity is suppressed. The lecture emphasized that recognition of CDK2 dependency has direct implications for drug development and has informed the exploration of selective CDK2 inhibitors as a strategy to overcome resistance.
In addition to cell-cycle rewiring, resistance to CDK4/6 inhibitors is supported by activation of oncogenic signaling pathways. The slides highlighted involvement of the PI3K–AKT–mTOR pathway, which can sustain tumor growth and survival despite CDK4/6 blockade and often overlaps with endocrine resistance mechanisms. Activation of the RAS–MAPK pathway was also discussed as a contributor to resistance, reflecting broader signaling network activation that enables tumor cells to escape cell-cycle control.
Taken together, these mechanisms illustrate that resistance to CDK4/6 inhibitors reflects coordinated biological adaptation, rather than isolated genetic changes. Loss of RB1 function, adaptive CDK6 upregulation, activation of the cyclin E–CDK2 axis, and engagement of oncogenic signaling pathways collectively define the resistance landscape. Understanding these processes through translational and molecular approaches is essential to inform treatment strategies beyond progression.
Conclusion
In conclusion, genomic and molecular plasticity plays a central role in the development of resistance to CDK4/6 inhibitors. Advances in translational research over the past two years particularly in the metastatic and neoadjuvant settings have significantly improved our understanding of resistance biology and are increasingly shaping clinical practice. Continued integration of molecular insights into therapeutic decision-making will be essential to further improve outcomes for patients with HR+/HER2– breast cancer.