Breast cancer is a malignant tumor that originates in the cells of the breast. Globally, it stands as the most frequently diagnosed cancer among women and is a leading cause of cancer-related deaths. In the United States, breast cancer accounts for about 30% of all new female cancers each year. (American Cancer Society). Early detection through regular screenings, such as mammograms, significantly enhances treatment success rates and reduces mortality. The American Cancer Society recommends that women aged 40 and older have the option to start annual breast cancer screening with mammograms. (American Cancer Society)
This article will delve into the causes, symptoms, types, stages, diagnosis, and treatment options for breast cancer, providing a comprehensive overview to promote awareness and understanding of this prevalent disease.
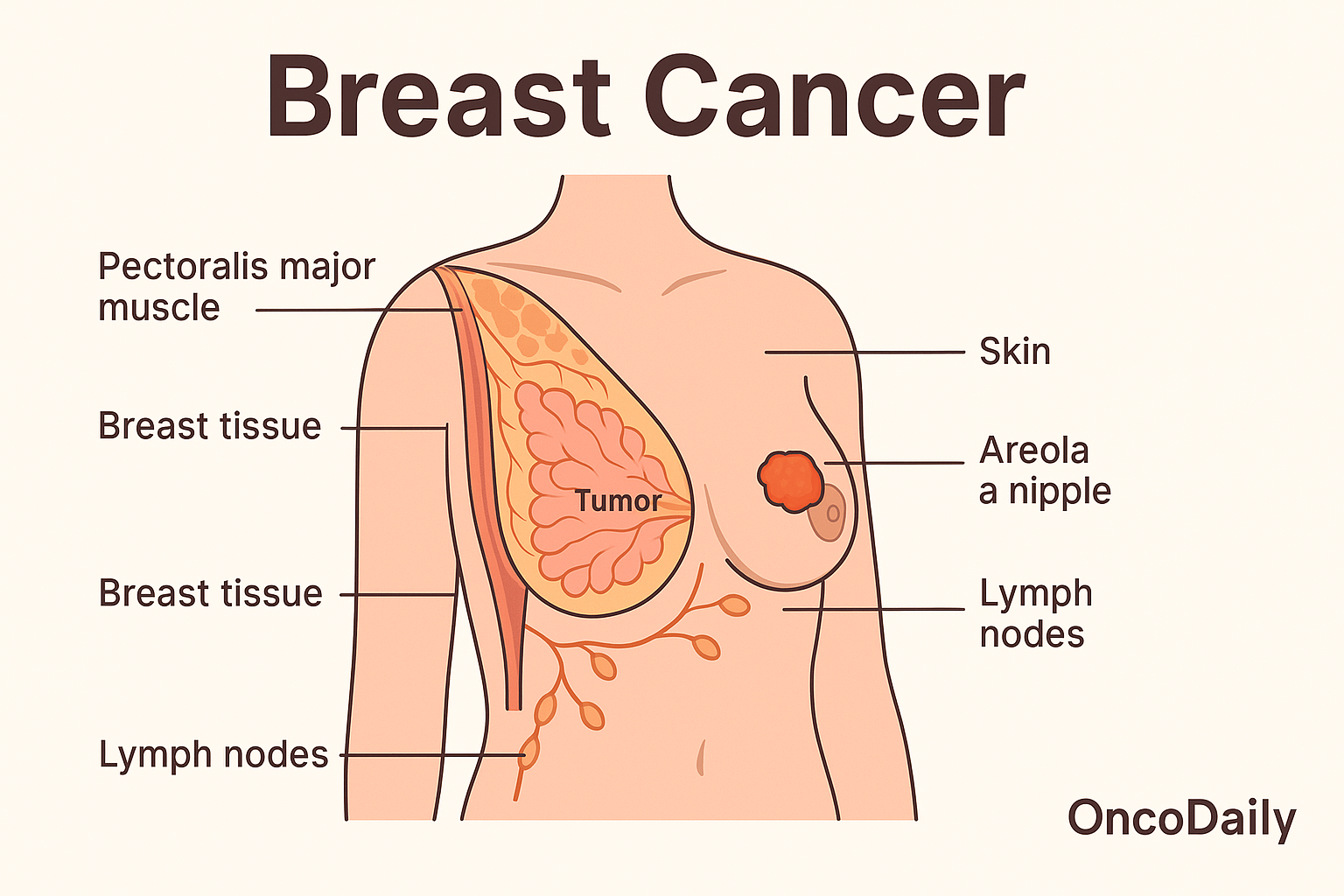
What Are the Symptoms of Breast Cancer?
Breast cancer manifests through various symptoms, with the most commonly reported being the presence of a lump in the breast. According to the National Breast Cancer Foundation, approximately 40% of diagnosed breast cancers are detected by women who feel a lump during self-examination.
Other notable symptoms include changes in breast shape or size, nipple discharge, and skin alterationssuch as dimpling. A survey commissioned by Breast Cancer Now revealed that the percentage of women regularly checking their breasts has decreased from 49% in 2022 to 45% in 2024, with 11% reporting never having performed a self-exam.
Becoming familiar with one’s own breast anatomy can aid in early detection of abnormalities. The Mayo Clinic emphasizes that understanding the typical look and feel of your breasts can help identify changes that should be reported to a healthcare professional.
What are the Causes and Risk Factors for Breast Cancer?
Breast cancer arises from a combination of genetic, environmental, and lifestyle factors. Inherited mutations, particularly in the BRCA1 and BRCA2 genes, significantly increase risk, with women carrying these mutations facing up to a 72% lifetime risk. (breastcancer.org).
Environmental exposures, such as radiation, and lifestyle choices, including high-fat diets, also contribute to risk. Key factors like family history, advancing age, reproductive history, and obesity further influence likelihood. For instance, the average American woman has about a 13% lifetime risk of developing breast cancer.( Cancer.org). Preventive actions, such as regular screenings and lifestyle modifications, are essential for early detection and risk reduction.
What Are the Types of Breast Cancer?
Breast cancer is classified into several types based on its origin and characteristics. The main types include:
- Ductal Carcinoma In Situ (DCIS)
- Invasive Ductal Carcinoma (IDC)
- Lobular Carcinoma In Situ (LCIS)
- Inflammatory Breast Cancer (IBC)
- Triple-Negative Breast Cancer (TNBC)
- HER2-Positive Breast Cancer
Each type has distinct features, influencing diagnosis, treatment, and prognosis.
Ductal Carcinoma in Situ (DCIS)
Ductal carcinoma in situ (DCIS) is an early form of breast cancer where abnormal cells are confined to the milk ducts, not invading surrounding tissues. While DCIS is non-invasive and highly treatable, it can progress to invasive breast cancer if left untreated. In a study published in Signal Transduction and Targeted Therapy, first author Dr. Yuchen Liu reported that untreated ductal carcinoma in situ (DCIS) progresses to invasive ductal carcinoma (IDC) in approximately 25–60% of cases.
Additionally, recent findings suggest that surgery might not be necessary for women with DCIS, as close monitoring with mammograms can be just as effective. Recent studies indicate that active monitoring could be a viable alternative to immediate surgery for certain low-risk DCIS patients. A clinical trial led by Dr. E. Shelley Hwang from Duke Cancer Institute involved nearly 1,000 women with low-risk, hormone-sensitive DCIS. The study found that after two years, the rates of invasive cancer development were similar between those who underwent standard treatment (surgery and radiation) and those who opted for active monitoring with regular mammograms. These findings suggest that nonsurgical approaches may be appropriate for some patients, though longer follow-up is necessary to confirm the safety of this approach.
Invasive Ductal Carcinoma (IDC)
Invasive ductal carcinoma (IDC) is the most prevalent form of breast cancer, accounting for approximately 80% of all invasive cases. IDC originates in the milk ducts and subsequently invades surrounding breast tissue. If not detected and treated promptly, IDC can metastasize to lymph nodes and other organs. According to the American Cancer Society, about 13% of women will develop invasive breast cancer in their lifetime.
Survival rates for IDC vary depending on the stage at diagnosis. According to the American Cancer Society, the 5-year relative survival rate for localized breast cancer is over 99%. However, if the cancer has spread to regional lymph nodes, the 5-year survival rate decreases to 87%, and further declines to 32% if distant metastasis occurs.
Early detection through regular screenings, such as mammograms, significantly improves prognosis. Advancements in treatment options, including targeted therapies and personalized medicine, continue to enhance outcomes for IDC patients.
Triple-Negative Breast Cance
Triple-negative breast cancer (TNBC) is an aggressive subtype characterized by the absence of estrogen, progesterone, and HER2 receptors, rendering it unresponsive to hormonal and HER2-targeted therapies. This lack of targeted treatment options contributes to its challenging prognosis. According to the American Cancer Society, TNBC accounts for about 10-15% of all breast cancers. The five-year relative survival rates for TNBC vary by stage at diagnosis:
- Localized (cancer confined to the breast): Approximately 91%
- Regional (spread to nearby lymph nodes): Approximately 65%
- Distant (metastasized to other organs): Approximately 12%
These statistics underscore the importance of early detection in improving outcomes for TNBC patients. Recent studies have explored potential prognostic biomarkers for TNBC. For instance, research published in Breast Cancer Research and Treatment by Cheng et al. found that the expression of fibroblast growth factor receptor 1 (FGFR1) is associated with poorer overall survival in TNBC patients, suggesting its potential as a prognostic marker.
Additionally, a study highlighted by the Mayo Clinic in 2024 indicated that early-stage TNBC patients with higher levels of immune cells within their tumors may have a lower risk of recurrence and better survival rates, even without chemotherapy. This finding suggests that the tumor microenvironment plays a significant role in TNBC progression and could inform future therapeutic strategies.
How Is Breast Cancer Diagnosed?
Breast cancer diagnosis relies on a combination of imaging and tissue analysis to detect abnormalities and confirm malignancy. Mammograms are the most common screening tool, helping to identify suspicious areas in breast tissue. When further evaluation is needed, ultrasounds can provide detailed imaging, especially in dense breast tissue. MRI scans offer high-resolution images, particularly for high-risk individuals or cases requiring more precise assessment. If an abnormality is detected, a biopsy is performed to extract tissue samples for definitive diagnosis. Together, these methods ensure accurate detection and guide treatment planning.
Mammograms for Breast Cancer Detection
Mammograms are the primary screening tool for breast cancer, particularly recommended for women over 40 and those at elevated risk. This low-dose X-ray procedure compresses each breast between two plates to capture detailed images, enabling the detection of abnormalities such as calcifications and masses. Regular mammography is advocated because it can identify cancerous changes before physical symptoms emerge, significantly enhancing treatment success. According to a study published in Cancer, women who participated in mammography screening experienced a 41% reduction in breast cancer mortality within 10 years.
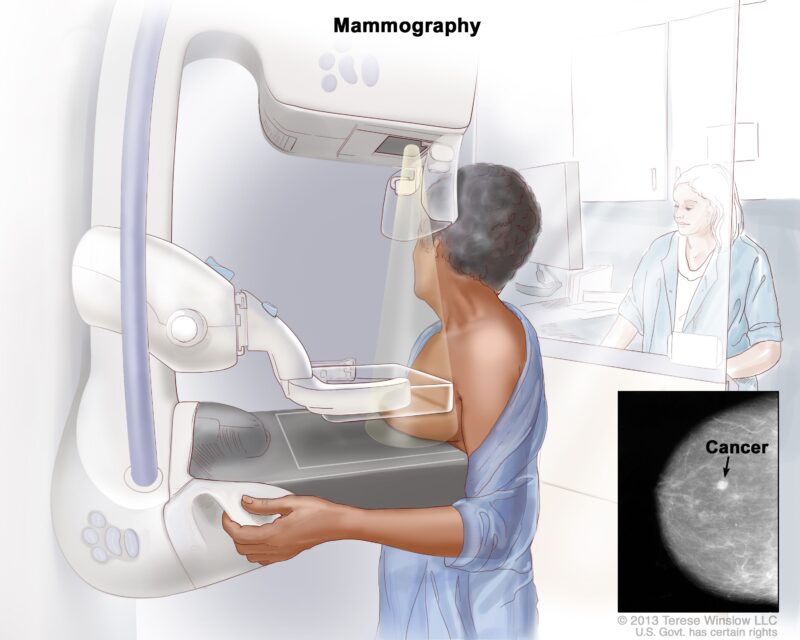
Furthermore, the National Breast Cancer Foundation reports that early detection of breast cancer, when it is localized, results in a 99% five-year relative survival rate. These statistics underscore the critical role of regular mammograms in early detection and improving survival outcomes.
Ultrasounds for Breast Cancer Diagnosis
Ultrasound is a valuable tool for further evaluating breast abnormalities detected during mammography. It effectively distinguishes between solid masses and fluid-filled cysts by using sound waves to create detailed images. A cyst appears as a well-circumscribed, anechoic (dark) area with posterior acoustic enhancement, while a solid mass typically presents as a hypoechoic (lighter) region without this enhancement.
In women with dense breast tissue, mammography’s sensitivity decreases significantly. A study by Dr. Solveig Hofvind, published in Breast Cancer Research and Treatment, found that sensitivity decreased with increasing density from 78% in women with BI-RADS 1 to 47% in those with BI-RADS 4.
To address this limitation, supplemental ultrasound is often employed. Research indicates that adding ultrasound to mammography can detect an additional 1.6 to 4 cancers per 1,000 women screened.
However, it’s important to note that while supplemental ultrasound can improve cancer detection rates, it may also increase the likelihood of false-positive results, leading to unnecessary biopsies
MRI Scans for Breast Cancer Diagnosis
Magnetic Resonance Imaging (MRI) is a crucial diagnostic tool for breast cancer, particularly beneficial for women with a high genetic risk, such as BRCA1 or BRCA2 mutation carriers, or those with inconclusive results from other screening methods. Unlike mammography, which utilizes X-rays, MRI employs strong magnetic fields and radio waves to generate detailed images of breast tissue, offering superior contrast between normal and abnormal tissues. This enhanced imaging capability allows for the detection of tumors that may be obscured in dense breast tissue or missed by other modalities.
For high-risk populations, incorporating MRI into routine screening has demonstrated significant benefits. A study by Dr. Janie M. Lee, published in the Journal of Clinical Oncology, found that combining MRI with mammography improved cancer detection rates and overall survival in women at elevated risk of breast cancer. The study reported a cancer detection yield of 24.8 per 1,000 screenings with combined MRI and mammography, compared to 15.0 per 1,000 with mammography alone. Furthermore, the overall survival rate was significantly higher in the combined screening group.
These findings underscore the importance of MRI as a supplemental screening tool for high-risk women, enhancing early detection and improving survival outcomes.
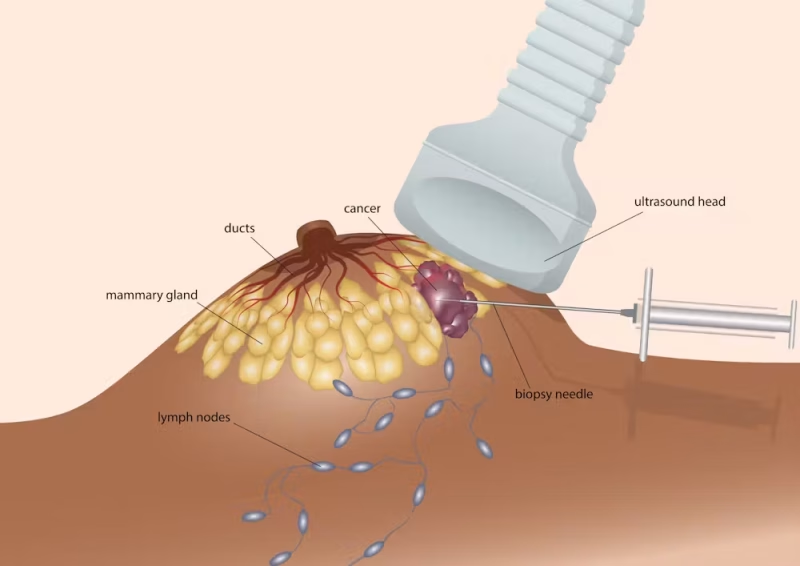
Biopsies for Confirming Breast Cancer
A biopsy is the definitive method for diagnosing breast cancer, involving the extraction of tissue or fluid from a suspicious area for microscopic examination. Various biopsy techniques are employed based on the lesion’s characteristics and location:
- Fine-Needle Aspiration (FNA): This minimally invasive procedure uses a thin needle to withdraw fluid or cells from a palpable lump. While FNA is less invasive, its sensitivity can vary. A review in BMC Cancer reported a sensitivity of approximately 92.7% when unsatisfactory samples were excluded.
- Core Needle Biopsy: Utilizing a larger, hollow needle, this method extracts small cylinders of tissue, providing more comprehensive samples than FNA. According to a study in the Journal of Clinical Pathology, core needle biopsy demonstrates a sensitivity ranging from 90% to 99% for invasive breast cancer.
- Excisional Biopsy: In cases where needle biopsies are inconclusive or the lesion is not easily accessible, an excisional biopsy involves surgically removing the entire lump or suspicious area. This method is more invasive but offers a comprehensive tissue sample for analysis.
The accuracy of these biopsy methods is generally high. A study highlighted by Breastcancer.org found that 96% of invasive breast cancer diagnoses from biopsies matched the final diagnosis, while 84% of ductal carcinoma in situ (DCIS) diagnoses were concordant.
Genetic Testing and Risk Assessment
Genetic testing for mutations in the BRCA1 and BRCA2 genes is a critical tool in assessing a woman’s risk of developing breast cancer. These genes produce proteins responsible for repairing DNA damage; when mutated, their function is compromised, leading to an increased likelihood of breast and ovarian cancers. Individuals with harmful BRCA mutations have a higher risk of developing these cancers, often at younger ages.
The testing process involves analyzing a blood or saliva sample to identify specific genetic alterations. It is particularly recommended for individuals with a personal or family history of breast, ovarian, tubal, or peritoneal cancer, or those of Ashkenazi Jewish descent, as they have a higher prevalence of BRCA mutations. The U.S. Preventive Services Task Force advises that primary care clinicians assess such individuals using appropriate familial risk assessment tools.
Identifying a BRCA mutation significantly influences medical decisions. For instance, women with these mutations may consider enhanced surveillance, chemoprevention, or prophylactic surgeries to reduce cancer risk. The Centers for Disease Control and Prevention notes that risk-reducing mastectomy and salpingo-oophorectomy are effective preventive measures for BRCA mutation carriers.
Breast Self-Examination (BSE)
Breast self-examination (BSE) is a method where individuals check for lumps, changes in size or shape, or nipple discharge. It involves visual inspection and manual palpation, ideally performed monthly at the same time in one’s menstrual cycle. While BSE helps individuals become familiar with their breasts, its effectiveness in reducing breast cancer mortality is debated.
The American Cancer Society no longer recommends BSE as a primary screening tool, emphasizing mammograms and clinical exams as more reliable for early detection. While BSE is useful for breast awareness, it should not replace professional screenings, which remain essential for early diagnosis and effective treatment.

What Are the Treatment Options for Breast Cancer?
Breast cancer treatment encompasses various modalities tailored to the tumor’s characteristics and patient-specific factors. Surgical interventions, such as lumpectomy and mastectomy, aim to remove cancerous tissue, often serving as initial treatment steps. Chemotherapy employs cytotoxic drugs to eradicate rapidly dividing cancer cells and may be administered before (neoadjuvant) or after (adjuvant) surgery, depending on the disease stage and tumor biology.
Radiation therapy utilizes high-energy rays to target and destroy residual cancer cells post-surgery, thereby reducing recurrence risk. This approach is particularly beneficial following breast-conserving surgery and in cases where cancer has spread to nearby lymph nodes. In a retrospective study published in Frontiers in Oncology, researchers evaluated the effectiveness of de-escalated radiotherapy in patients with T1-2N1M0 HER2-overexpressing breast cancer receiving anti-HER2 targeted therapy. The study specifically examined the outcomes of omitting regional lymph node irradiation (RNI) after breast-conserving surgery and only performing whole-breast irradiation, or omitting postmastectomy radiation therapy. The findings suggested that de-escalated radiotherapy might be feasible in this patient population, potentially reducing treatment-related side effects without compromising efficacy.
Hormonal (endocrine) therapy is effective for hormone receptor-positive breast cancers. Medications such as tamoxifen or aromatase inhibitors either block hormone receptors or decrease estrogen production, thereby inhibiting cancer cell proliferation. This therapy is typically administered over several years to diminish recurrence risk. According to the National Cancer Institute, hormone therapy is a common component of breast cancer treatment, particularly for hormone receptor-positive subtypes.
Targeted therapy has revolutionized the management of HER2-positive breast cancers. Agents like trastuzumab, a monoclonal antibody, specifically target the HER2 protein, impeding tumor growth and enhancing survival rates.
Regarding targeted therapy, trastuzumab has significantly improved outcomes for patients with HER2-positive breast cancer. A pivotal study published in the New England Journal of Medicine demonstrated that adding trastuzumab to adjuvant chemotherapy improved disease-free survival rates. However, the combination with anthracycline-based regimens was associated with an increased risk of cardiac toxic effects.
Surgical Options for Breast Cancer
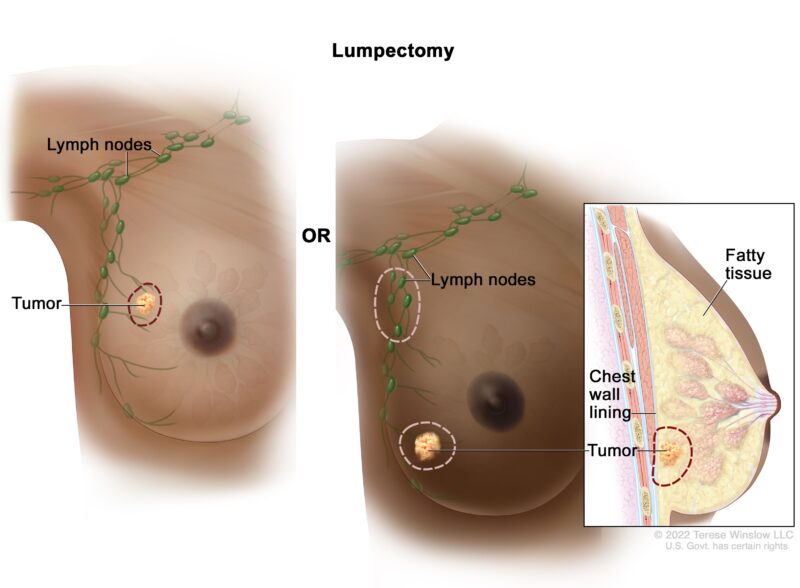
In the surgical management of breast cancer, two primary procedures are commonly considered: lumpectomy and mastectomy.
Lumpectomy involves the excision of the tumor along with a margin of surrounding healthy tissue, aiming to conserve as much of the breast as possible. This breast-conserving surgery is typically followed by radiation therapy to eradicate any residual cancer cells. Recovery from a lumpectomy is generally swift, with many patients resuming normal activities within a few days to a week. Risks associated with lumpectomy include potential changes in breast shape, scarring, and the possibility of local recurrence. A study published in JAMA Surgery found that breast-conserving surgery with postoperative radiotherapy offers comparable survival rates to mastectomy without radiotherapy.
Mastectomy entails the complete removal of one or both breasts and is often recommended for patients with multiple tumors, large tumor size relative to breast size, or genetic predispositions such as BRCA mutations. The recovery period for mastectomy is longer, typically spanning several weeks, and may involve more significant postoperative discomfort. Risks include infection, hematoma, seroma, and potential psychological impacts due to the loss of the breast.
Chemotherapy for Breast Cancer
Chemotherapy is a cornerstone in breast cancer treatment, utilizing potent drugs to target and eliminate rapidly dividing cancer cells. These agents interfere with the cancer cell’s ability to grow and divide, leading to cell death. Chemotherapy can be administered at various stages:
- Neoadjuvant Chemotherapy: Given before surgery to shrink tumors, making them easier to remove.
- Adjuvant Chemotherapy: Administered after surgery to eradicate any remaining cancer cells and reduce the risk of recurrence.
- Metastatic Setting: Used to control cancer that has spread beyond the breast to other parts of the body.
Chemotherapy drugs work by targeting rapidly dividing cells, a hallmark of cancer cells. However, they can also affect healthy cells that divide quickly, such as those in the bone marrow, digestive tract, and hair follicles, leading to various side effects.
The side effects of chemotherapy depend on the specific drugs used, dosage, and individual patient factors. According to the American Cancer Society, common side effects include: Hair loss, nail changes, mouth sores, loss of appetite or weight changes, nausea and vomiting, diarrhea, fatigue, increased risk of infections due to low white blood cell counts, easy bruising or bleeding from low platelet counts, nerve damage (neuropathy). These side effects are usually temporary and subside after the completion of treatment. Supportive care measures are available to manage many of these symptoms effectively.
Recovery from chemotherapy varies among individuals. Some patients may resume normal activities during treatment, while others might need more time to recover post-therapy. It’s essential to maintain open communication with healthcare providers to manage side effects and adjust treatment plans as needed.
The effectiveness of chemotherapy in breast cancer treatment depends on various factors, including the cancer stage, tumor characteristics, and individual patient health. According to the American Cancer Society, the 5-year relative survival rate for breast cancer is 91%, but it drops to 86% at 10 years and 81% at 15 years after diagnosis.
Recent Advancement in Breast Cancer
Recent advancements in breast cancer treatment have introduced novel therapies that offer promising outcomes for patients.
- Antibody-Drug Conjugates (ADCs): ADCs are an innovative class of targeted chemotherapy that combines an antibody specific to cancer cells with a cytotoxic drug. This design allows for direct delivery of chemotherapy to cancer cells, minimizing damage to healthy tissues. A notable example is Datopotamab deruxtecan (Datroway), recently approved by the FDA for adults with unresectable or metastatic hormone receptor-positive, HER2-negative breast cancer. In clinical trials, Datroway showed a median increase in progression-free survival (PFS) of 6.9 months compared to 4.9 months with standard chemotherapy.
- Selective Estrogen Receptor Degraders (SERDs): SERDs are a class of drugs that target estrogen receptors, leading to their degradation and inhibiting the growth of estrogen receptor-positive breast cancer cells. Elacestrant (Orserdu) is an oral SERD approved for postmenopausal women or adult men with estrogen receptor-positive, HER2-negative, ESR1-mutated advanced or metastatic breast cancer. Clinical studies have demonstrated its efficacy in patients with disease progression following prior endocrine therapy.
- Immunotherapy: The integration of immunotherapy into breast cancer treatment has shown encouraging results. A clinical trial led by the Peter MacCallum Cancer Centre investigated the addition of the immunotherapy drug nivolumab to pre-surgery chemotherapy in patients with early-stage, high-risk, estrogen receptor-positive, HER2-negative breast cancer. The study found that this combination nearly doubled the rate of pathological complete response, indicating no detectable cancer cells post-treatment.
- Liquid Biopsies: Liquid biopsies represent a less invasive method to detect tumor DNA in the bloodstream, facilitating personalized treatment strategies. The NHS in England has implemented liquid biopsies to identify specific genetic mutations in breast cancer patients, enabling the administration of targeted therapies such as elacestrant. This approach allows for more precise treatment and has the potential to improve patient outcomes.
What Are the Stages of Breast Cancer?
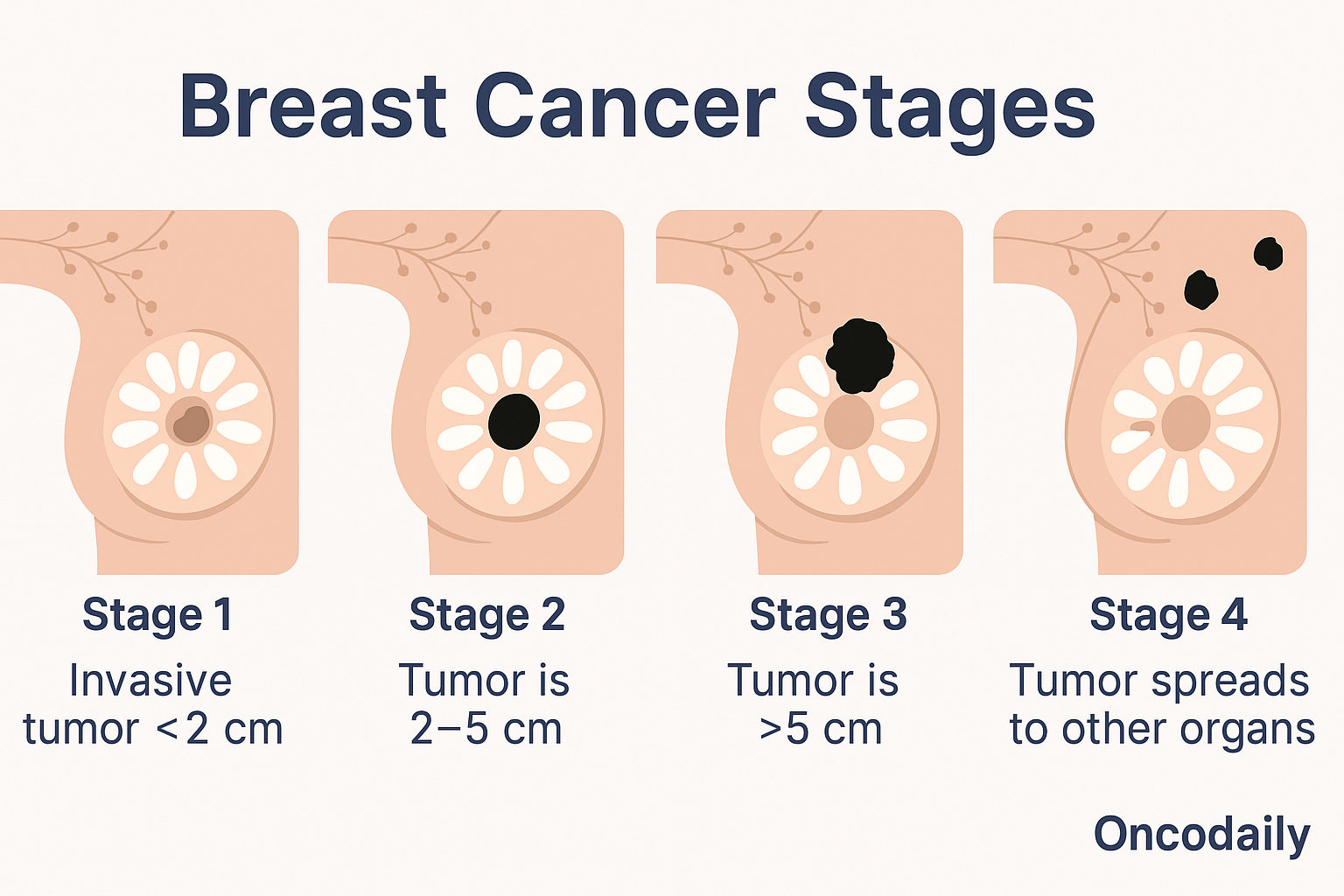
Breast cancer is classified into different stages based on tumor size, lymph node involvement, and whether the cancer has spread to other parts of the body. The staging system helps determine treatment options and prognosis. At Stage 0, known as ductal carcinoma in situ (DCIS), abnormal cells remain confined to the milk ducts and have not invaded surrounding tissue. While not yet invasive, DCIS can progress if left untreated.
Stage I marks the beginning of invasive breast cancer, where cancer cells have spread beyond the milk ducts into nearby breast tissue. In this early stage, tumors are typically small—no larger than 2 centimeters—and may or may not have reached the lymph nodes. Treatment at this stage is highly effective, often involving surgery and radiation.
As the disease progresses to Stage II, tumors grow larger, sometimes exceeding 5 centimeters, and cancer may spread to nearby lymph nodes. Despite its advancement, treatment options remain curative, with a combination of surgery, chemotherapy, and radiation commonly used to manage the disease.
In Stage III, the cancer is considered locally advanced, often spreading extensively to lymph nodes and nearby tissues such as the chest wall or skin. This stage may present more aggressive tumors, requiring intensive treatment, including chemotherapy, targeted therapy, and surgery.
By Stage IV, breast cancer has metastasized to distant organs such as the lungs, liver, bones, or brain. At this stage, the disease is no longer curable, but advancements in systemic therapies, including targeted treatments and immunotherapy, have significantly improved survival rates and quality of life for patients.
How to Live with Breast Cancer?
Managing daily life with breast cancer involves balancing physical, emotional, and psychological well-being. Fatigue and pain can be managed with rest, gentle exercise, and proper nutrition. Emotional health is crucial—seeking counseling or therapy can help cope with anxiety and stress. Support groups provide a sense of community, reducing feelings of isolation. Mental health care, including mindfulness and relaxation techniques, can improve overall well-being. Open communication with loved ones and healthcare providers ensures better emotional and medical support throughout treatment.
Can Breast Cancer Be Prevented?
Reducing breast cancer risk involves a combination of healthy lifestyle choices and regular screenings. Experts recommend a balanced diet rich in fruits, vegetables, and whole grains, along with regular exercise, which can lower risk by up to 20%. Limiting alcohol and avoiding smoking further reduces risk. Regular mammograms help detect cancer early, with annual screenings advised for women over 40. Genetic testing is crucial for those with a family history or BRCA mutations, allowing for preventive measures like enhanced screening or risk-reducing surgery. Early detection and proactive health choices are key to prevention (Cancer.org).
You Can Watch More on OncoDaily Youtube TV
Written by Toma Oganezova, MD
FAQ
What is breast cancer, and why is early detection important?
Breast cancer is a disease where abnormal cells in the breast grow uncontrollably. Early detection through screening methods like mammograms increases the chances of successful treatment and survival.
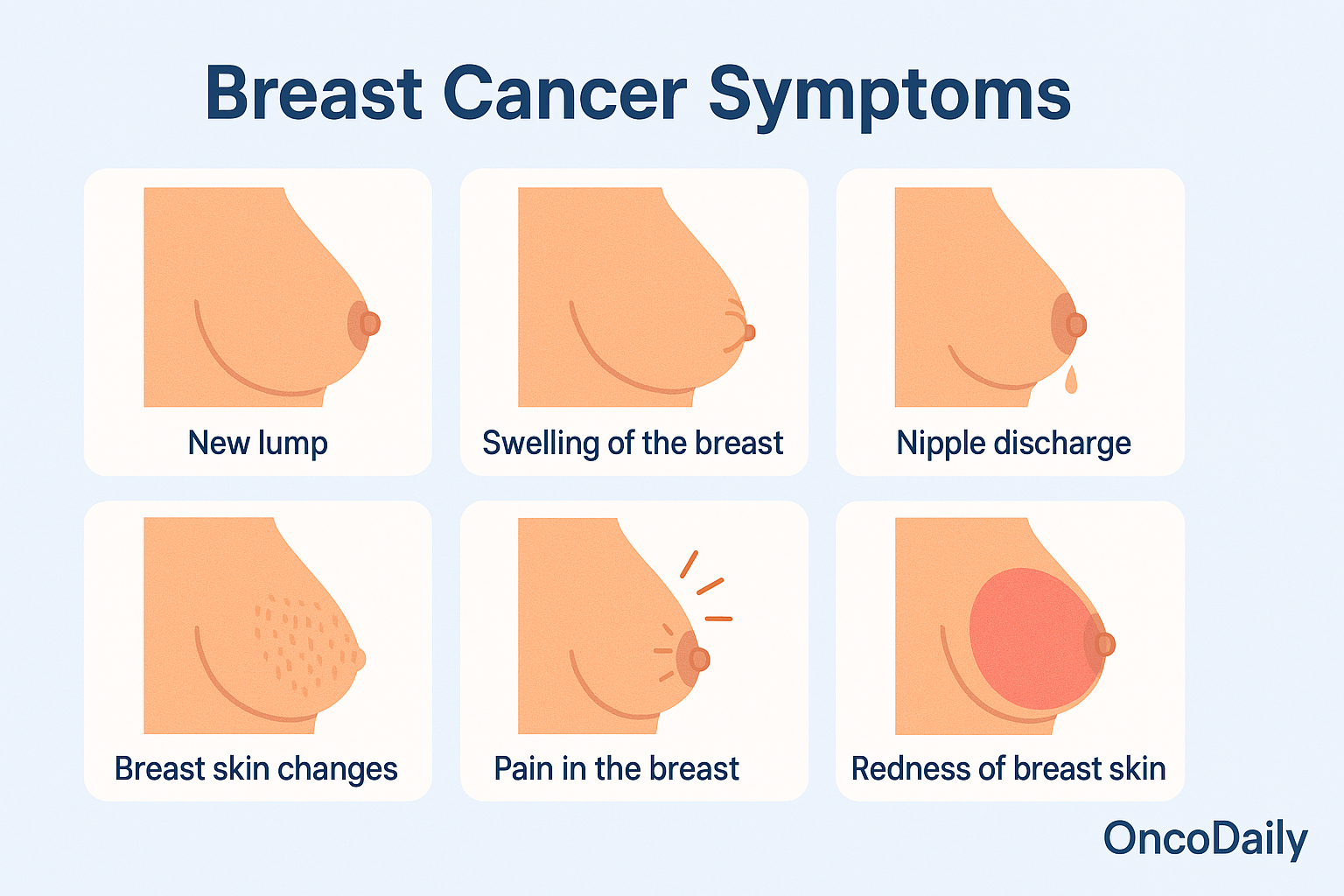
What are the common symptoms of breast cancer?
Breast cancer symptoms may include a lump in the breast, nipple discharge, skin dimpling, breast pain, and changes in breast shape or size.
What are the main risk factors for developing breast cancer?
Risk factors include age, genetics (BRCA1/BRCA2 mutations), family history, obesity, alcohol consumption, hormone therapy, and radiation exposure.
What are the different types of breast cancer?
Common types include invasive ductal carcinoma (IDC), invasive lobular carcinoma (ILC), ductal carcinoma in situ (DCIS), triple-negative breast cancer (TNBC), and inflammatory breast cancer (IBC).
How is breast cancer staged?
Breast cancer stages range from Stage 0 (non-invasive) to Stage IV (metastatic), based on tumor size, lymph node involvement, and spread to distant organs.
What are the main screening methods for breast cancer?
Screening includes mammograms, breast ultrasounds, MRI, and clinical breast exams to detect abnormalities before symptoms appear
What treatment options are available for breast cancer?
Treatment options include surgery (lumpectomy, mastectomy), chemotherapy, radiation therapy, hormone therapy, targeted therapy, and immunotherapy.
Can lifestyle changes help reduce breast cancer risk?
Yes, maintaining a healthy weight, exercising regularly, eating a balanced diet, limiting alcohol intake, and avoiding smoking can lower the risk.
How does genetic testing help in breast cancer prevention?
Genetic testing identifies BRCA1, BRCA2, and other gene mutations that increase breast cancer risk, helping high-risk individuals take preventive measures.
Can men get breast cancer?
Yes, although rare, male breast cancer can occur, especially in men with high estrogen levels, obesity, or genetic mutations like BRCA2.


