Sarcopenia in NSCLC has gained increasing attention as a potential prognostic marker, particularly in the context of systemic therapies. Making a notable presentation at MASCC 2025, Julia Kooser (United States) introduced new findings on the prognostic relevance of sarcopenia and CT-derived fat metrics—such as visceral and subcutaneous fat area—in patients with non-small cell lung cancer (NSCLC) undergoing immunotherapy.
Background
Body composition has emerged as a potential biomarker in oncology, with growing interest in the prognostic significance of skeletal muscle mass and fat distribution. Sarcopenia—characterized by low skeletal muscle mass—has been associated with poor treatment tolerance and worse survival outcomes in several cancers.
Similarly, increased visceral adiposity has been linked to systemic inflammation and impaired immune responses. However, the role of these metrics in predicting response to immune checkpoint inhibitors remains unclear, particularly in non-small cell lung cancer (NSCLC). This study sought to determine whether CT-based measures of muscle and fat composition could serve as prognostic indicators in NSCLC patients undergoing checkpoint inhibitor therapy.
Study Design and Methods
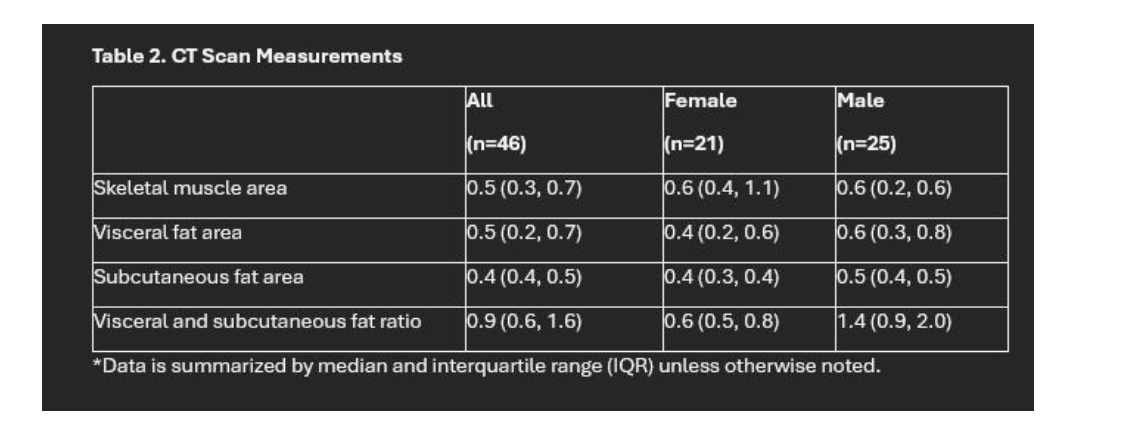
The investigators conducted a retrospective analysis of NSCLC patients who received immune checkpoint inhibitors, focusing on CT scans obtained within 60 days before or after initiation of treatment. Body composition was assessed at the third lumbar vertebra (L3) level, a standard anatomical reference for evaluating muscle and fat compartments. Using TeraRecon software, a single trained reader quantified skeletal muscle area (SMA), subcutaneous fat area (SFA), and visceral fat area (VFA). These values were normalized to patient height in meters squared to calculate indices such as the skeletal muscle index (SMI).
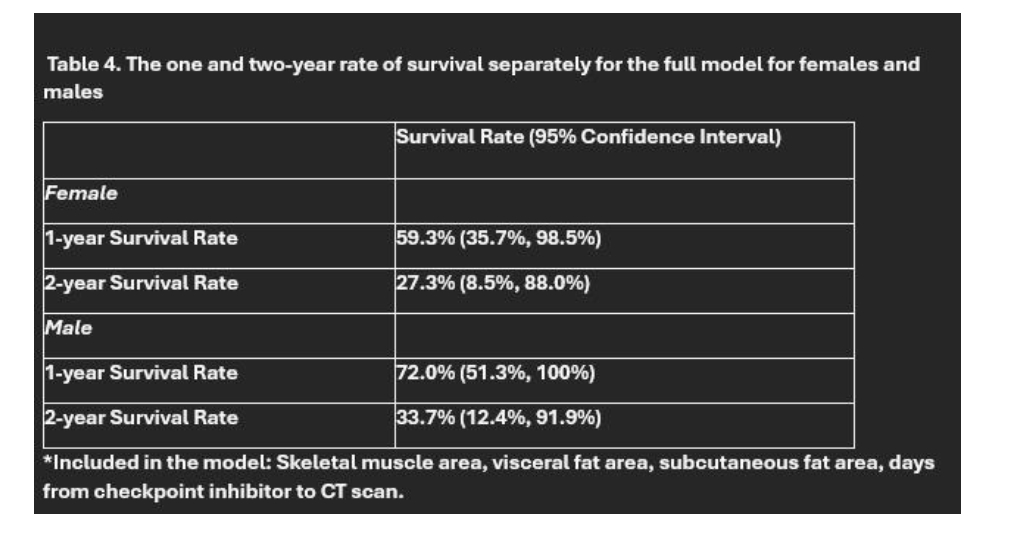
The primary endpoint was overall survival, defined as the number of days from the baseline CT scan to death. The researchers utilized Cox proportional hazards models to analyze the relationship between body composition metrics and survival outcomes at one and two years. Additionally, multivariable regression models were applied, incorporating all body composition parameters simultaneously.
Results
Among the 46 NSCLC patients analyzed:
- Skeletal Muscle Index (SMI) showed no statistically significant association with survival at 1 or 2 years.
- Subcutaneous Fat Area (SFA) and Visceral Fat Area (VFA) also did not correlate with overall survival.
- The visceral-to-subcutaneous fat ratio, often hypothesized to reflect systemic inflammation, did not impact survival outcomes.
- Gender-specific analyses revealed no significant associations between body composition and survival in either male or female patients.
- The time interval between CT imaging and checkpoint inhibitor initiation (up to 60 days) did not influence prognostic value.
- Results remained consistent in multivariate models, adjusting for all CT-derived parameters.
Interpretation
These findings suggest that, in this small cohort, pre-treatment levels of muscle and fat as measured by CT imaging do not offer predictive value regarding patient survival during checkpoint inhibitor therapy. While sarcopenia has been associated with poor outcomes in patients receiving chemotherapy or targeted therapy, its role in the immunotherapy context may be more nuanced. Similarly, although visceral adiposity is known to contribute to systemic inflammation and immunosuppression, it did not appear to influence outcomes in this population.
There are several potential explanations for the null results. The relatively small sample size may have limited the statistical power to detect subtle associations. In addition, the retrospective nature of the study and variability in timing of CT scans relative to treatment initiation could have introduced confounding. Finally, the biological interplay between host metabolism, body composition, and immune response may be more complex than currently understood.
Conclusion and Future Directions
This study highlights the need for caution when interpreting the prognostic value of body composition in NSCLC patients treated with immune checkpoint inhibitors. While CT-based metrics such as SMI, SFA, and VFA are easy to derive and potentially informative, this analysis did not find evidence to support their routine use as biomarkers in this setting. Larger, prospective studies are needed to validate these findings and explore whether body composition can meaningfully contribute to personalized treatment strategies in lung cancer immunotherapy.
Understanding the interaction between nutrition, muscle mass, fat distribution, and the immune system remains an important area of investigation in the era of precision oncology. With advances in imaging analytics and artificial intelligence, future research may uncover more sophisticated composite markers that better predict immunotherapy response.
You can read the full abstract here.