The third week of December brings important updates across GI oncology, spanning prognostic biomarkers, precision oncology, translational immunology, and emerging therapeutic strategies.
This week’s selection highlights how biological context—from liver fat and ctDNA dynamics to intratumoral immune architecture—continues to refine risk stratification and guide treatment decisions across colorectal, gastric, and pancreatic cancers. Advances in biomarker-driven therapy, investigator-led clinical research, and next-generation immunotherapies further underscore the accelerating pace of innovation in the field.
Together, these ten posts reflect another week of clinically relevant, practice-shaping progress across the GI oncology landscape.
Deborah Ophoff, PhD Candidate – Nutrition and Cancer, Wageningen University
“𝐓𝐡𝐞 𝐟𝐢𝐫𝐬𝐭 𝐩𝐚𝐩𝐞𝐫 𝐨𝐟 𝐦𝐲 𝐏𝐡𝐃 𝐢𝐬 𝐨𝐮𝐭!
In this paper, we investigated liver fat at time of diagnosis, reflected by liver radiodensity on computed tomography (CT) scans, in relation to cancer recurrence and survival in 1596 patients with stage I-III colorectal cancer.
We found that that more liver fat was associated with a higher risk of cancer recurrence and worse survival among patients with colon cancer (n=1080), but not in those with rectal cancer (n=516). These findings may be explained by differences in cancer dissemination patterns (i.e. preferred routes for spread of cancer cells) for colon and rectal cancer.
These results need to be confirmed in future studies, but our findings suggest that liver fat is associated with colon cancer prognosis.”
Kohei Shitara, MD, PhD – Medical Oncologist, National Cancer Center Hospital East, Japan
“One of the most exciting papers I have shared this year: 51 cases with durable complete response and “potential cure” in metastatic gastric/GEJ cancer.
Biomarker-driven therapy is expanding curative possibilities.”
Shivan Sivakumar, MD, PhD – Associate Professor of Oncology, University of Birmingham; Honorary Consultant in Medical Oncology, NHS
“Happy to see that Nature highlighted one of our papers as one of six highlights of pancreatic cancer research in 2025. It was a great team effort to understand the intricacies of the intratumoural immune system in this disease to help develop better therapies.”
Annalice Gandini, MD – Resident in Medical Oncology
“Available online our original paper PANICET on the switch from cetuximab to panitumumab during encorafenib-based therapy in metastatic colorectal cancer.
Outcomes with ENCO-PANI were comparable to ENCO-CET in the BEACON trial and these results support this combination as a valid option in patients unable to continue CET.”
Anirban Maitra, MBBS – Physician-Scientist; Pancreatic Cancer Research
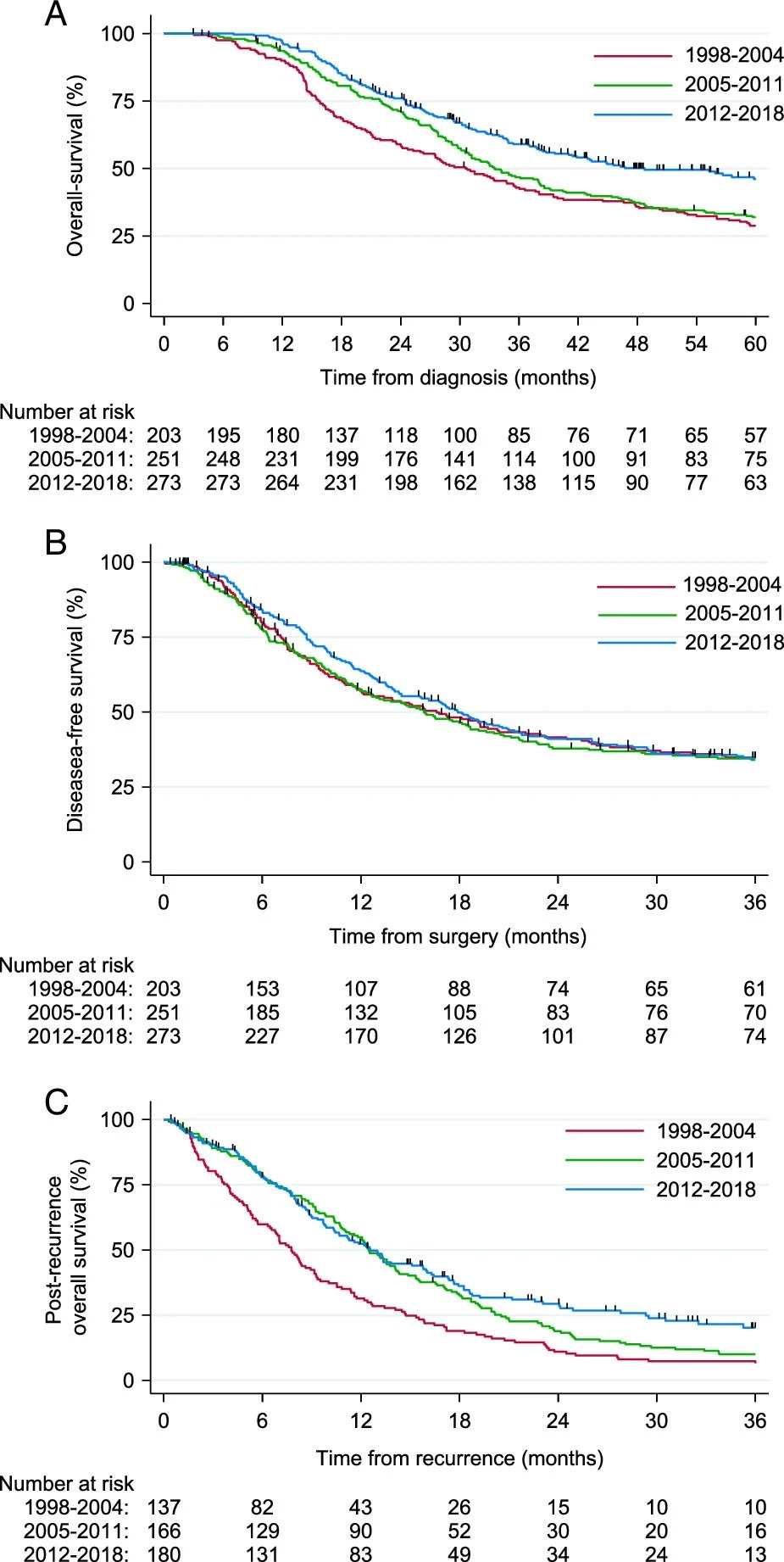
“Trends Over Time in Recurrence Patterns and Survival Outcomes after Neoadjuvant Therapy & Surgery for Pancreatic Cancer MD Anderson News series shows improved overall survival (~50months) & post recurrence OS, reinforcing impact of multimodality therapies.”
Amy Huang, MD – Medical Oncologist; Gastrointestinal Cancers
“Our Conquer Cancer Merit Award-winning meta-analysis on EGFR inhibitor rechallenge for metastatic colorectal cancer has been published in JCOOP_ASCO
We showed that EGFR inhibitor rechallenge was associated with a significantly longer PFS, with the greatest benefit seen in patients with RAS/RAF wild-type disease confirmed by ctDNA testing. The response rates exceeded FDA-approved historical controls in the third-line setting, with manageable toxicity even in later-line use.”
Catherine Alix-Panabières – Full Professor of Oncology, Faculty of Medicine, University of Montpellier, France; Visiting Professor, University of Hamburg, Germany; Working Group Leader, ELBS
“Biology is changing. And last week, in Paris, we felt the momentum.
Not in a lab, not in a research center, but at the National Institute for Deaf Youth — a symbolic place to talk about something that has long remained unheard: the strategic future of Medical Biology.4 intense hours. A packed auditorium.
‘Medical Biology – Future, Challenges and Perspectives’
Biologists, clinicians, industry leaders, institutions, and patient advocates… all sitting at the same table. Not to observe change, but to ignite it.Thanks to Ortus – Communication et information en Santé, we didn’t just exchange ideas — we built a shared vision where biology is no longer hidden behind machines and lab reports, but front and center in diagnosis, care decisions, and therapeutic innovation.
I had the privilege to contribute to this story with a talk on:
‘Meeting the Oncology Challenge Through Biological Testing: the Case of Liquid Biopsy’Because cancer care is no longer only about treating a tumor —
It’s about detecting its whispers in the blood,
guiding decisions faster,
and offering patients truly personalized treatment, when it matters most.Across three round tables, one conviction emerged clearly:
Biology must become visible, strategic, innovative — and deeply human-centered.”

Noelia Tarazona, MD, PhD – Research Fellow, Mass General Brigham Cancer Center
“AFTER adding DYNAMIC III – When used at a single postoperative timepoint, tumor-informed and tumor-agnostic ctDNA assays show similar performance; however, with serial monitoring, tumor-informed assays clearly outperform tumor-agnostic approaches in sensitivity for recurrence detection.
This work moves beyond survival associations and focuses on what truly matters in daily practice: diagnostic accuracy, developed by our expert biostatistics Juan Antonio Carbonell Asins.”
Nicholas DeVito, MD – Assistant Professor of Medicine, Division of Medical Oncology, Duke University
“Very grateful for the opportunity to present our two concepts, one in the neoadjuvant setting and the other MRD+ CRC, neither of which have any standard of care option for patients. I opened to the audience with the reminder of the importance of investigator initiated trials, and how the K-SPY platform is transformative in this respect as well.
Most trials are not run by the physicians on the ground, who are seeing the patients and trying to come up with practical, scientifically justified solutions for them. In the hands of investigators, the patient is front and center. The Colorectal Cancer Alliance not only knows this but has done something to change it, empowering collaboration in the process.
The mission is obvious. The time is now. Let’s Cure Colorectal Cancer.”

Hung Trinh – Managing Director, Cell & Gene Therapy (CGT), Oncology, Vaccines, CMC/MFG
“UCLA scientists develop one-product-fits-all immunotherapy for pancreatic cancer
Pancreatic cancer is among the deadliest forms of cancer, with most patients diagnosed after the disease has already spread throughout the body. The five-year survival rate for metastatic cases hovers around 2–3%, and median survival is often measured in months rather than years.Now, UCLA researchers have engineered a novel immunotherapy that could offer new hope for a disease that has remained stubbornly resistant to treatment advances for decades. In a study published in PNAS, the team details how the therapy, called CAR-NKT cell therapy, can track down and destroy pancreatic tumors even after they’ve metastasized to other organs.
Targeting orthotopic and metastatic pancreatic cancer with allogeneic stem cell–engineered mesothelin-redirected CAR-NKT cells
Pancreatic cancer (PC) is one of the deadliest cancers, often diagnosed at advanced, hard-to-treat stages. Current cell-based therapies like CAR-T cells face major hurdles, including tumor variability, immune escape, and limited scalability. In this study, we developed an off-the-shelf immunotherapy using gene-engineered natural killer T cells derived from stem cells—called Allo15MCAR-NKT cells.
These cells target pancreatic tumors through multiple killing mechanisms, resist immune exhaustion, and avoid rejection by the patient’s immune system. In preclinical models, they effectively controlled tumor growth and spread. This work offers a promising step toward scalable, next-generation immunotherapy for PC, with the potential to address current treatment limitations and improve outcomes for patients with advanced disease.”

You can also read about 10 Must-Read Posts in GI Oncology from the Second week of December on OncoDaily.


