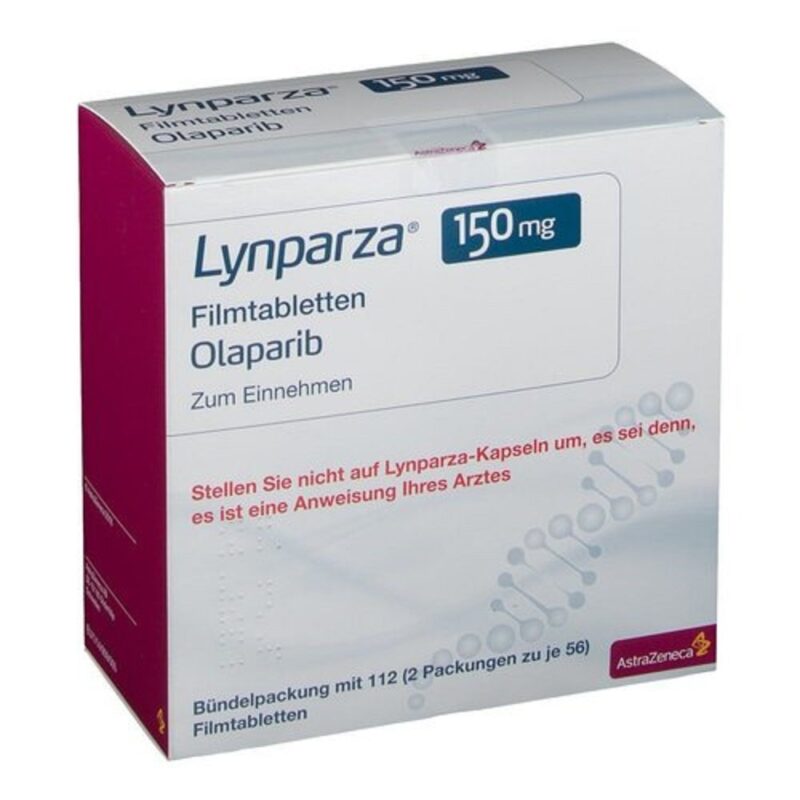
The ICR strongly welcomed the decision made by the National Institute for Health and Care Excellence (NICE) to recommend olaparib as a treatment option for patients with locally advanced or metastatic breast cancer.
The decision was groundbreaking as it made this pioneering targeted therapy available through the NHS. Olaparib is specifically for patients with HER2-negative breast cancer that is linked to faulty BRCA1 or BRCA2 genes, a group of patients who have had limited treatment options until now.
The recommendation by NICE applied to those who had undergone chemotherapy, and whose cancer had continued to progress or spread. Olaparib works by targeting cancer cells that rely on these faulty genes for their growth and survival. By inhibiting this mechanism, the drug can help to slow or stop the cancer’s progression, offering patients a crucial opportunity for extended survival and a better quality of life. This approval represents a significant advancement in personalized cancer treatment, providing tailored therapies that can significantly improve outcomes for specific patient populations.
The approval of olaparib also highlighted the growing importance of targeted therapies in cancer care. It reinforced the potential of precision medicine, which focuses on individual genetic profiles to develop more effective and less toxic treatments. For patients with advanced breast cancer caused by BRCA1 or BRCA2 mutations, olaparib offers a new and promising option, and its availability through the NHS is a significant step forward in providing access to life-saving treatments for those who need it most.
About Olaparib
Olaparib is a targeted therapy belonging to a class of drugs known as PARP inhibitors, which work by blocking the action of the PARP enzyme. This enzyme is involved in repairing DNA damage in cells. By inhibiting PARP, olaparib makes it difficult for cancer cells, particularly those with BRCA1 or BRCA2 mutations, to repair their damaged DNA. As a result, the cancer cells accumulate DNA damage and eventually die. This makes olaparib an effective treatment for cancers with these specific genetic mutations, as it selectively targets the defective repair mechanism in cancer cells while sparing healthy cells.
Olaparib was approved for use in patients with inherited mutations in the BRCA1 or BRCA2 genes who have early-stage, high-risk breast cancer. Since April 2023, women with these mutations in England and Wales have been able to access the drug through the NHS. Olaparib has demonstrated substantial benefits in this group, helping to reduce the risk of cancer recurrence and offering a more personalized treatment approach. By using genetic profiling to identify those who would benefit most, the drug ensures a more effective and tailored treatment plan, improving survival rates in patients with high-risk breast cancer.
The recent expansion of olaparib’s availability to patients with advanced or metastatic breast cancer represents another critical step forward in precision medicine. For those whose cancer has recurred after previous treatments, this approval offers a new line of defense. The drug targets the underlying genetic faults driving the cancer, making it a vital option for patients with HER2-negative breast cancer, which is more challenging to treat with traditional therapies. This approval broadens the accessibility of a potentially life-saving treatment, improving the outlook for patients whose cancer has not responded to other therapies, and ensuring that more individuals benefit from the advancements in cancer treatment.
The ICR’s Role in the Development of Olaparib
The Institute of Cancer Research (ICR) has played a pivotal role in the development of olaparib, significantly contributing to its emergence as a groundbreaking treatment for certain types of cancer. ICR scientists were the first to identify that cancer cells with mutations in the BRCA1 or BRCA2 genes were particularly vulnerable to PARP inhibitors like olaparib. This discovery was a crucial milestone, as it provided a scientific basis for using PARP inhibitors in treating cancers with these specific genetic defects. By targeting the DNA repair mechanisms that are already compromised in cancer cells with BRCA mutations, olaparib could effectively prevent these cells from repairing further damage, leading to their death and providing a new avenue for treatment.

Clinical trials of olaparib were led by researchers from the ICR and The Royal Marsden NHS Foundation Trust, providing the necessary evidence to support its clinical use. These trials demonstrated the drug’s efficacy across a variety of cancers associated with BRCA1 and BRCA2 mutations, including breast, ovarian, and prostate cancers. Through rigorous testing and analysis, the trials showed that olaparib was not only effective in treating these cancers but also helped extend patients’ survival and improve their quality of life. This success has made olaparib a standard treatment option for patients with BRCA-related cancers and continues to inspire further research into targeted therapies.