Olubukola Ayodele, Consultant Medical Oncologist at the University Hospitals of Leicester NHS Trust, posted on LinkedIn:
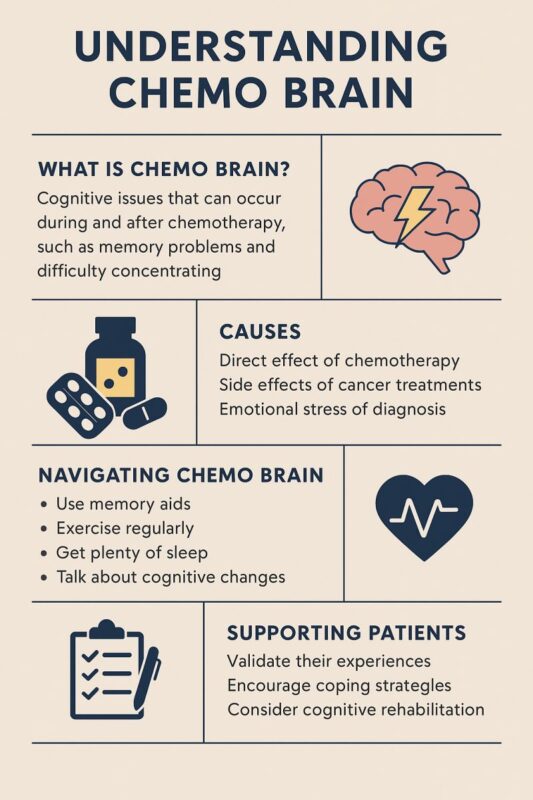
““Chemo brain” It’s real, it’s frustrating, and it’s often misunderstood.
As a breast oncologist, I see how cancer impacts far more than the body. One of the most commonly overlooked but deeply felt effects of treatment is Cancer-Related Cognitive Impairment, often called “chemo brain.”
For many patients, it’s more than just being forgetful. It’s:
– Struggling to find the right words
– Losing your train of thought mid-sentence
– Difficulty concentrating or multitasking
– Feeling mentally “foggy” even months after treatment ends
And while we’ve traditionally labelled it “chemo brain,” the reality is more complex.
It can be caused by:
– Chemotherapy
– Hormonal therapies (like tamoxifen or aromatase inhibitors)
– Immunotherapy or targeted therapy
– Radiation therapy
– Sleep disturbances
– Anxiety, depression and fatigue
– Hormonal abnormalities such as thyroid issues, diabetes, nutrient disorders
– The cancer itself
For those living through it, the cognitive challenges can affect everything from work and relationships to confidence and independence. And yet, it’s often under-recognised and under-discussed in clinics. In some cases, cognitive changes may persist for months or even years after treatment.
So what can we do?
For patients:
– Know that you’re not imagining it. This is valid and it’s common
– Keep a journal to track memory lapses or triggers
– Try cognitive exercises, puzzles, or mindfulness apps
– Don’t be afraid to ask for accommodations at work or home
– Keep active
– Keep hydrated
– Talk to your healthcare team
For healthcare professionals:
– Acknowledge it openly, validation is therapeutic.
– Ensure no organic causes
– Integrate screening for cognitive symptoms into follow-up.
– Offer referrals to occupational therapy or cognitive rehabilitation services.
– Support research that explores both the mechanisms and solutions.
For all of us: We must broaden our understanding of survivorship. Survival is just the beginning, quality of life matters. And that includes brain health.
Let’s normalise talking about chemo brain and ensure our care models support the whole patient.
Remember, let’s keep up the conversations on cancer. Together, we can move beyond the silence and into supportive, informed care.”
More posts featuring Olubukola Ayodele on OncoDaily.


