Talha Badar, Hematology/Oncology Specialist at Mayo Clinic, shared a post on X:
“When is CML truly “resistant” or “relapsed,” and how should it be managed?
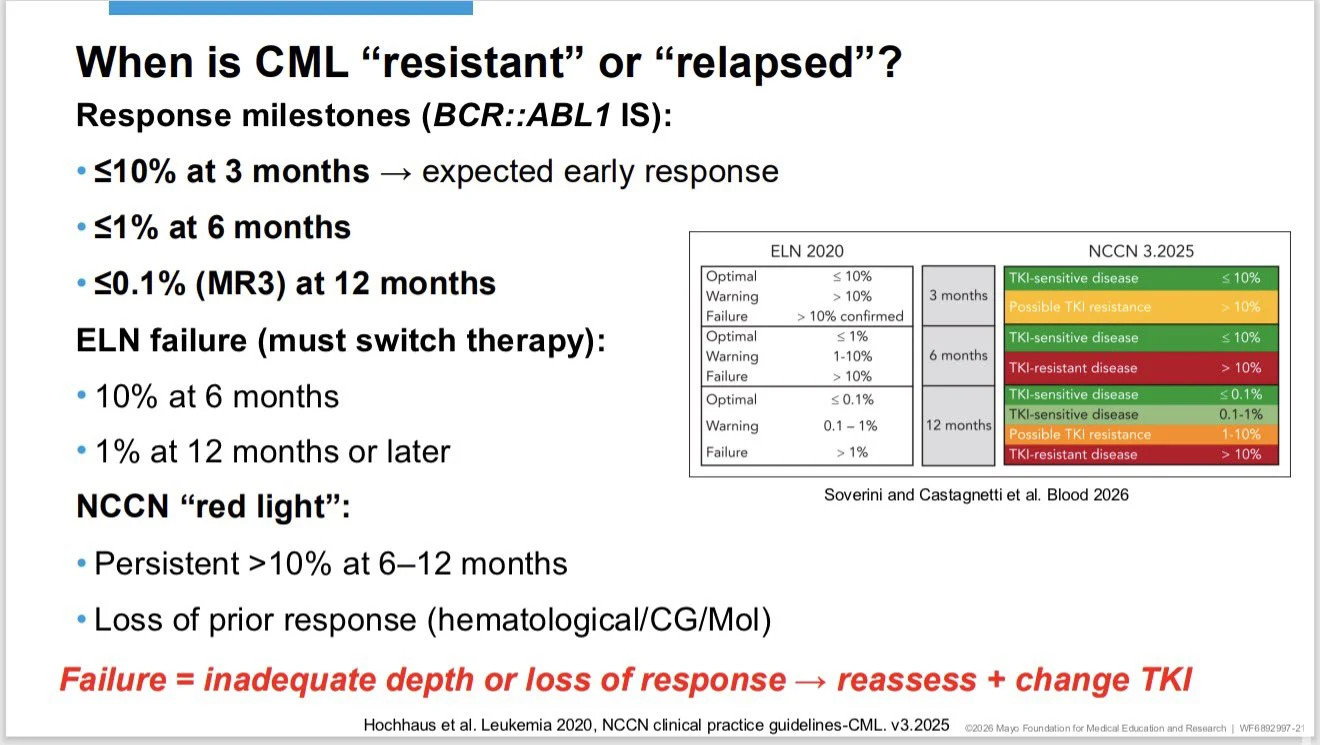
1. CML resistance is defined by molecular response milestones, not by symptoms.
Key BCR::ABL1 (IS) targets:
• ≤10% at 3 months (expected early response)
• ≤1% at 6 months
• ≤0.1% (MR3) at 12 months
ELN failure (therapy change required):
• >10% at 6 months
• ≥1% at 12 months or later
NCCN “red flags”:
• Persistent >10% at 6–12 months
• Loss of prior hematologic, cytogenetic, or molecular response
Failure = inadequate depth OR loss of response → reassess and change TKI
2. Before calling it resistance, rule out pseudo-resistance (very common):
- Non-adherence
- Drug–drug interactions
- Dose reductions or interruptions due to toxicity
- Poor monitoring or lab variability
Always correct these before switching TKIs.
3. Mutation testing is the single most important next step
• Perform NGS (preferred) at any failure or loss of response
• Mutations mainly exclude TKIs (what NOT to use) rather than selecting one perfect drug
Choosing the next TKI (stepwise, risk-adapted):
• Imatinib failure → 2G TKI (dasatinib, nilotinib, bosutinib) or asciminib
•2G TKI failure → ponatinib or asciminib preferred
• ≥2 TKIs or T315I → dose-adjusted ponatinib OR asciminib
• Consider allo-HCT only for true multi-TKI resistance
Asciminib now has a growing role across multiple lines, including earlier use in selected patients.
4. Big picture takeaway:
- In chronic-phase CML, survival is driven by TKIs.
- Transplant is reserved for failure, not choice.
Failure → reassess milestones → fix pseudo-resistance → test mutations → change therapy.”
More posts featuring Talha Badar on OncoDaily.


