Runcie C.W. Chidebe, Executive Director at Project PINK BLUE, shared a post on LinkedIn:
“Most high-income countries (HICs) have adopted precision medicine and targeted therapies, thereby increasing personalised care and treatment; however, in most low-income countries (LMICs), oncology diagnosis and treatment remain one-size-fits-all. Despite the potential of targeted therapies, access remains a significant challenge in most of the LMICs, including Nigeria. Barriers include limited availability of diagnostic technologies, restricted access to targeted therapies, inadequate funding, and insufficient infrastructure.
For example, pertuzumab, a HER2-targeted monoclonal antibody for breast cancer, was not available in Nigeria until five years after its introduction in the United States and Europe. Similarly, pembrolizumab was approved in the United States in 2016, but as of 2021, it was still not readily available in Nigeria. These challenges perpetuate inequities in cancer care, leading to poor patient outcomes, ethical dilemmas for clinicians, strain on health systems, and severe financial hardship for patients and families.
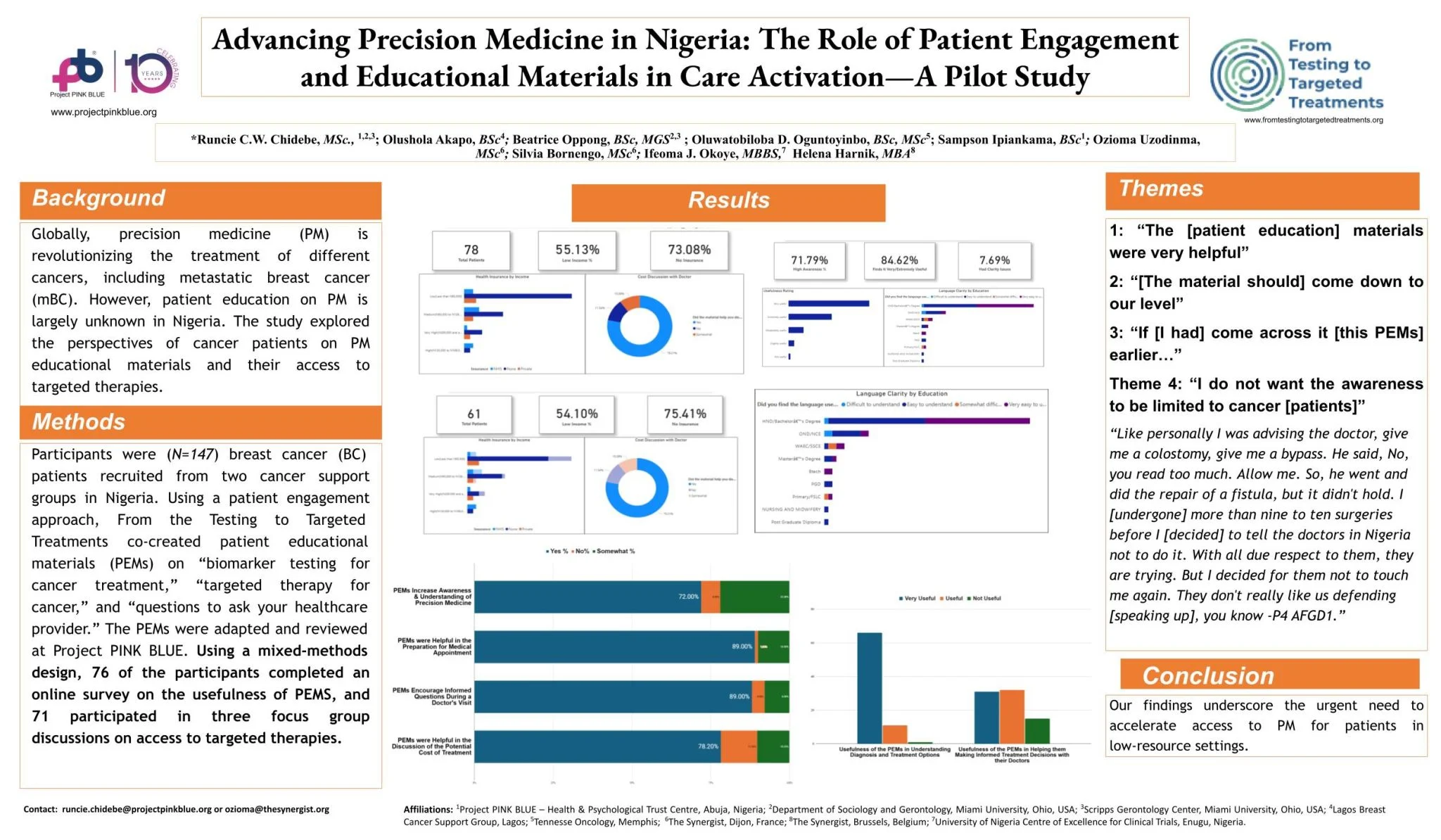
Project PINK BLUE, in partnership with From Testing to Targeted Treatments (FT3), wanted to accelerate access to precision medicine in Nigeria through different approaches(I.e., advocacy, policymakers engagement, HCP meetings). First, we decided to explore the bottom-top approach, that is, patient engagement: to explore the perspectives of cancer patients on precision oncology and test FT3 adaptable patient educational materials (PEMs).
We conducted a pilot mixed-method study and provided three FT3 PEMs (i.Targeted Therapy for Cancer, ii. Biomarker Testing for Cancer Treatment, and iii. Questions to Ask your Healthcare Provider About Your Cancer Diagnosis and Treatment) to all the patients. The pilot study was conducted in Enugu, Abuja and Lagos. The participants received a questionnaire and participated in a focus group.
Our findings show that many patients are on targeted therapy but are unaware of the specific treatment or its difference from chemotherapy. Themes were: ‘financial barriers to targeted therapies,’ ‘poor awareness of targeted therapies,’ and ‘lack of access to PEMs.’ A participant said, ‘We feel the cost is too high, and even when we have the money, it’s still not affordable.’
Our quantitative results showed that 71% of participants reported increased awareness of PM after reading the FT3 materials, 80% found the FT3 patient educational materials helpful for making informed decisions, and 90% rated the FT3 materials highly for clarity.
Our findings underscore the urgent need to educate patients about precision medicine and to accelerate access to it for patients in low-resource settings.
To our knowledge, this is the first study in Nigeria exploring patients’ perspectives on targeted treatments and the usefulness of FT3 materials.
Thanks to FT3 for making it possible to present this very important work at SABCS. Special thanks to all the patients who supported the study.”
More posts featuring Runcie C.W. Chidebe.