Olubukola Ayodele, Breast Cancer Lead at University Hospitals of Leicester NHS Trust, shared a post on LinkedIn:
“I had written a post earlier in the week about how a cancer diagnosis is trauma and we should communicate better and pace information appropriately, however, how can we give excellent care when the system doesn’t allow for this to happen?
Yes, some clinicians need to improve how they communicate. Yes, emotional intelligence matters. But I think we are missing a bigger and more uncomfortable truth.
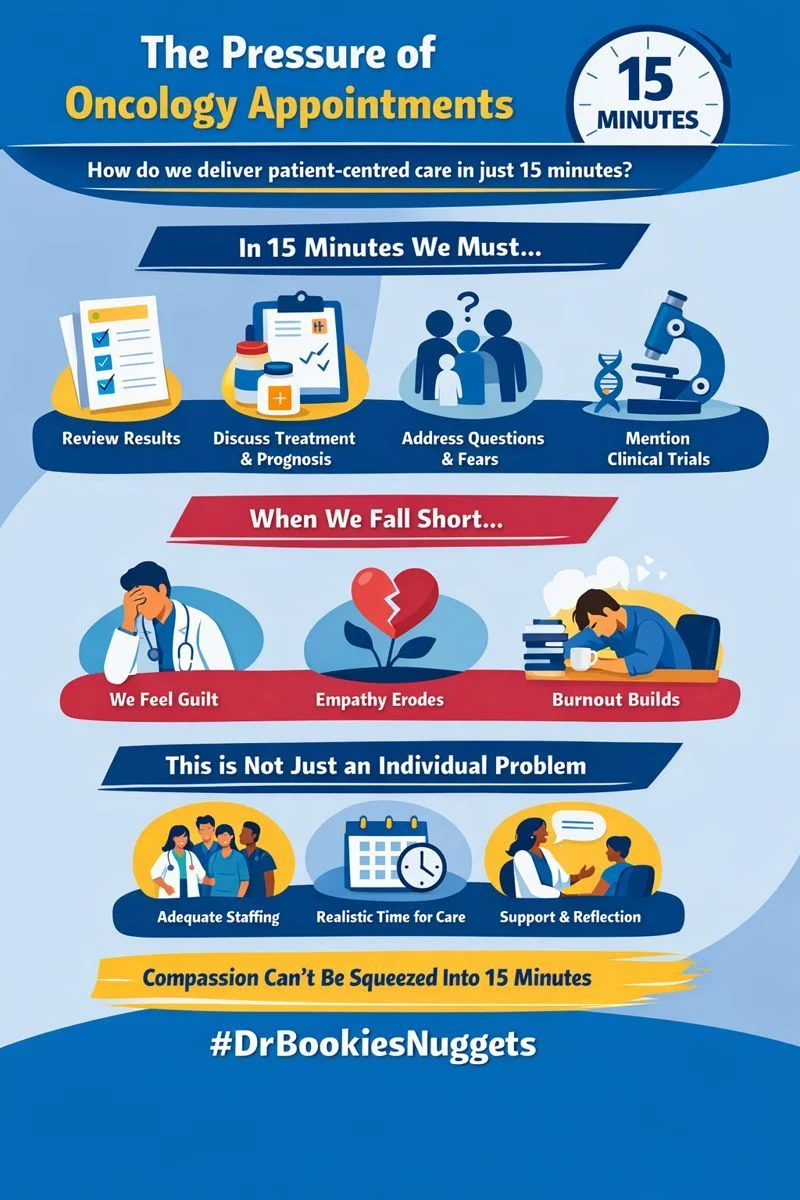
How do we genuinely deliver patient-centred care in a system that gives 15 minutes for a follow-up oncology appointment?
Fifteen minutes to review results.
Fifteen minutes to discuss treatment, side effects, prognosis, uncertainty.
Fifteen minutes to explore questions, fears, family dynamics, work, finances.
Fifteen minutes to mention clinical trials, when appropriate, and ensure true understanding. Add on the dynamics of needing interpreter services.
When we fall short, many doctors do not shrug and move on. They carry guilt. Guilt that they rushed an answer. Guilt that they did not explore a concern. Guilt that they did not raise a trial or sit a little longer with distress.
Over time, that guilt becomes exhausting.
We are on a slippery slope. Not because clinicians do not care, but because repeatedly knowing what good care looks like and being structurally unable to provide it creates MORAL DISTRESS. Without spaces for clinical supervision or emotional processing, especially in a specialty as intense as oncology, empathy can quietly erode. Burnout then follows.
We need to stop framing this purely as an individual communication problem.
This is a system problem. A system that prioritize quantity over quality.
If we want better communication, we need realistic clinic structures, adequate staffing, protected time, multidisciplinary support, and safe spaces for clinicians to reflect on the emotional weight of this work.
Compassion cannot be squeezed indefinitely into shrinking time slots.
As we await the UK National Cancer Plan it’s important that the wellbeing of those expected to implement the plan is factored and considered.
If we truly value patient-centred care, we must also care about the conditions in which clinicians are expected to deliver it.”
More posts featuring Olubukola Ayodele.


