Olubukola Ayodele, Breast Cancer Lead at University Hospitals of Leicester NHS Trust, shared a post on LinkedIn:
“Continued reflections from SABCS25.
- Oral novel endocrine therapies
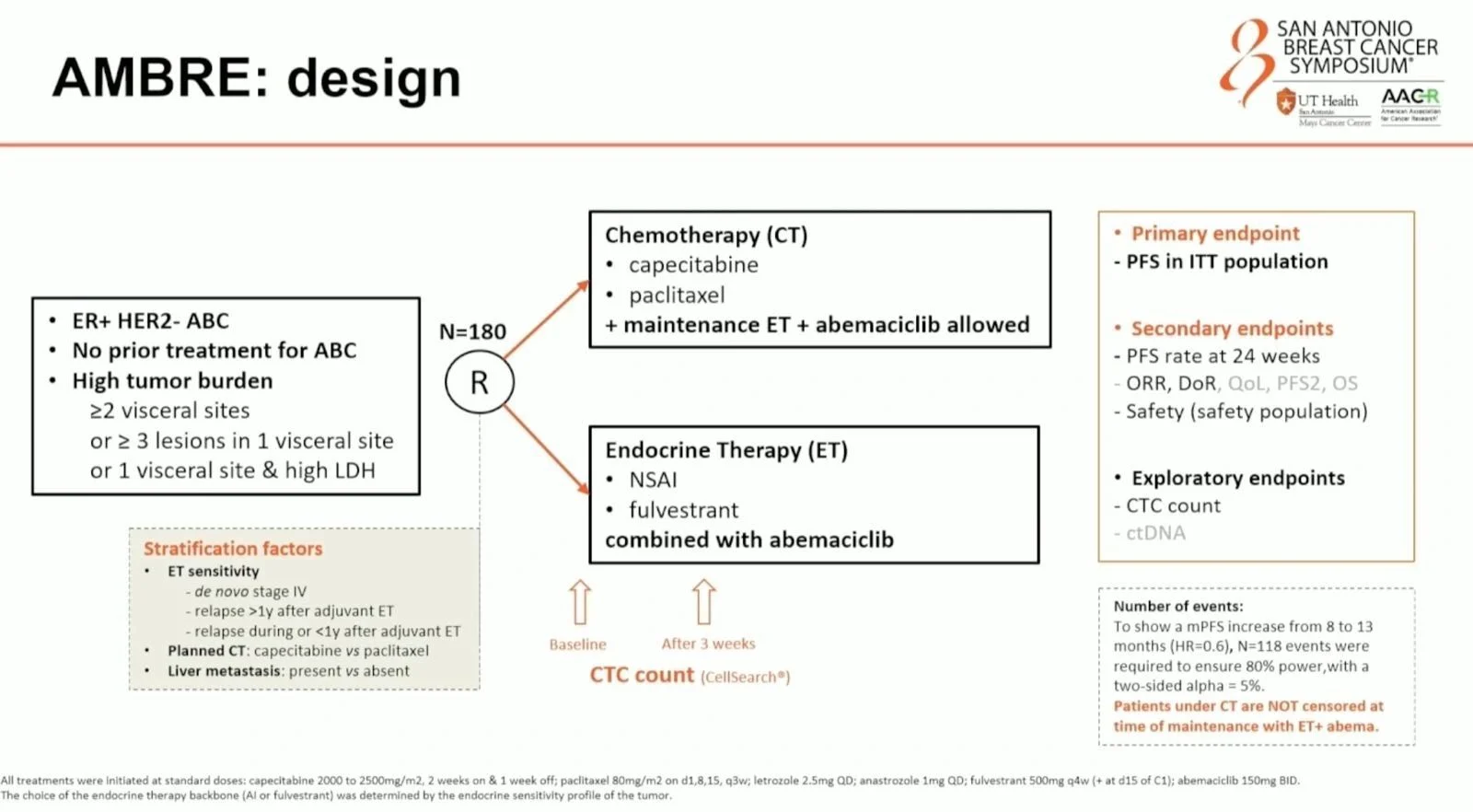
We are clearly entering an era where oral novel endocrine agents, such as SERDs, are beginning to replace aromatase inhibitors and tamoxifen, much as ADCs have reshaped chemotherapy. These agents will be used as monotherapy and in combinations. In metastatic disease, the evidence is already clear that combination strategies outperform monotherapy. - Reframing chemotherapy in visceral disease
Even in patients with heavy visceral burden, we should no longer default to chemotherapy. Trials such as ABIGAIL, RIGHT CHOICE, PADMA and now AMBRE consistently show superior outcomes with first-line CDK4/6 inhibitors compared with chemotherapy, with important implications for both survival and quality of life. - ALLTO in triple positive early breast cancer
ALLTO finally provides clarity in HR+/HER2+ early breast cancer, a group not adequately addressed in SOFT and TEXT.
At 10-year follow-up: improved DFS and time to distant recurrence with AI (HR 0.65), seen in both premenopausal patients receiving OFS plus AI and in postmenopausal patients. There was no OS difference. Importantly, there was no benefit from adding OFS to tamoxifen. The message is clear: AI plus OFS is preferred. If not feasible, tamoxifen alone is reasonable. The middle ground of tamoxifen plus OFS adds no benefit. - PATINA and CNS outcomes
PATINA reinforces the benefit of adding palbociclib to anti-HER2 therapy + ET after induction chemotherapy in HR+/HER2+ metastatic disease. Notably, there were lower rates of CNS progression, including in patients with baseline brain metastases. Median PFS improved from 29.1 to 44.3 months (HR 0.7), with CNS progression or death delayed at 3 years. - Rising incidence in younger women
Breast cancer incidence continues to rise in younger women, with annual increases of around 1.1% in those under 40 and 1.4% in those <50. What is particularly concerning is that we still lack appropriate screening tools for women in their 20s and 30s. Age-based screening alone is no longer sufficient. Many younger women at risk are missed using current criteria. A personalised, risk-stratified approach incorporating genetics, breast density and clinical risk factors is urgently needed, rather than blanket age cut-offs. - Alcohol and breast cancer risk
There is no safe level of alcohol when it comes to breast cancer risk. Data continue to show a dose-dependent relationship, particularly for hormone receptor + disease. Patterns of binge drinking, increasingly common in younger women, appear especially harmful. Even episodic intake, such as 4 glasses of wine or 5 pints of lager within a few hours once a month, increases risk. This is a modifiable factor we must be more confident discussing with patients.
Plenty to reflect on, and much that should prompt us to rethink how we counsel patients and design services.”
More posts about SABCS25.


