Nina Niu Sanford, Assistant Professor and Chief of Gastrointestinal Radiation Oncology at Harvard/Brigham and Women’s Hospital/Massachusetts General Hospital, shared a post on X:
“Happy Sunday! Back with another teaching video: ~20 min on managing toxicity from upper GI radiotherapy.
I discuss these 5:
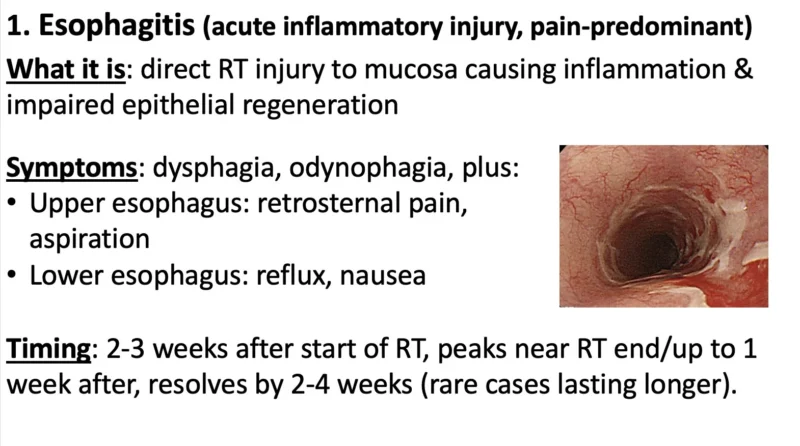
- esophagitis
- stricture
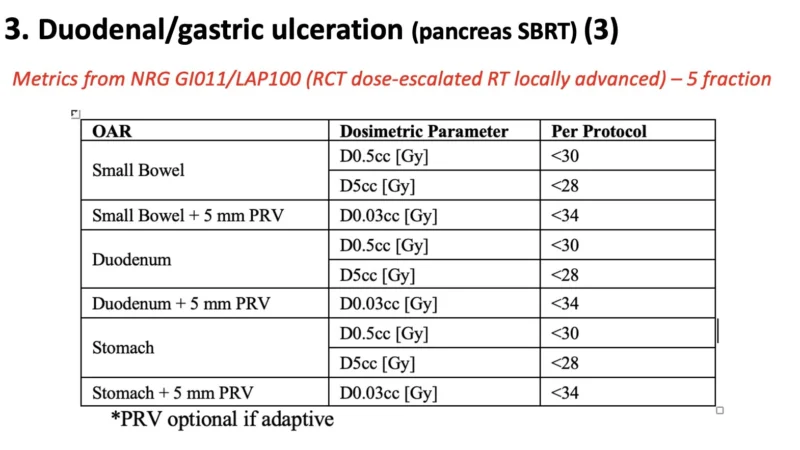
- duodenal/gastric ulcer (pancreas SBRT)
- nausea/vomiting
- abdominal pain
Full video and slides (with some more thoughts).
Esophagitis. An acute/sub-acute toxicity caused by direct RT injury to mucosa. High dose/volume to circumferential/long segment esophagus increases risk.
Management summarized. Note premade MMW can be $$$ (or not on formulary), so the EPIC script for mixing is below.
Esophageal stricture. Same risk factors as acute esophagitis, which itself increases stricture risk.
Pts should be warned, so they don’t automatically assume progressive dysphagia = recurrence (but get EGD). Dilation is treatment, often need multiple (rule of 3’s).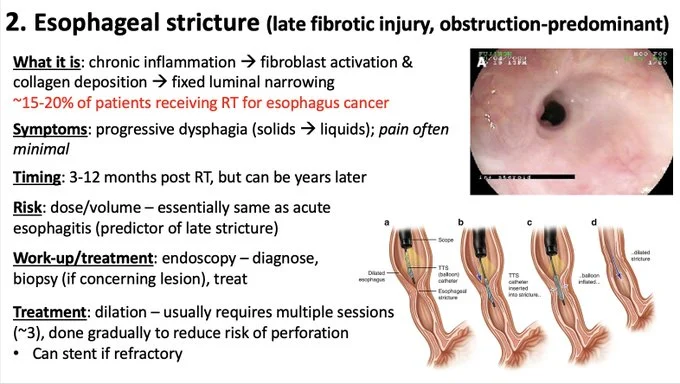
Duodenal/gastric ulceration. This is the dose-limiting toxicity of pancreas SBRT. Uncommon, delayed, but serious & largely preventable. Importantly can happen even if no acute symptoms. Here is my empiric med reg (PPI & carafate). Also metrics from NRG-GI011 (5 fx).
Nausea/vomiting and abdominal pain. Many meds for nausea. My algorithm below. Curious other experience with olanzapine.
For pain, important to try to discern etiology. Timing matters. I don’t avoid narcotics, but note can worsen symptoms. Pancreatic insufficiency often missed.
Obviously there is variability in management. Let me know what I missed. Thanks as always to Chris Anker for insights.”
More posts featuring Nina Niu Sanford.