Massoud Toussi, Real-World Evidence and Epidemiology Leader at Toussilver and Editor-in-Chief at Epidemiology Open Access Journal, shared a post on LinkedIn:
“Once viewed as a supplementary data source, Real‑World Evidence (RWE) has rapidly evolved into a strategic cornerstone across the life sciences ecosystem. From informing regulatory approvals to shaping market access strategies and guiding clinical care, RWE is no longer “nice-to-have”—it’s mission-critical.
Professionals in pharmaceutical companies, CROs, medtech firms, regulatory agencies, health technology assessment (HTA) bodies, healthcare systems, and patient advocacy organizations are all navigating a new reality: evidence generated outside traditional clinical trials now drives decisions that impact patients, payers, and product lifecycles.
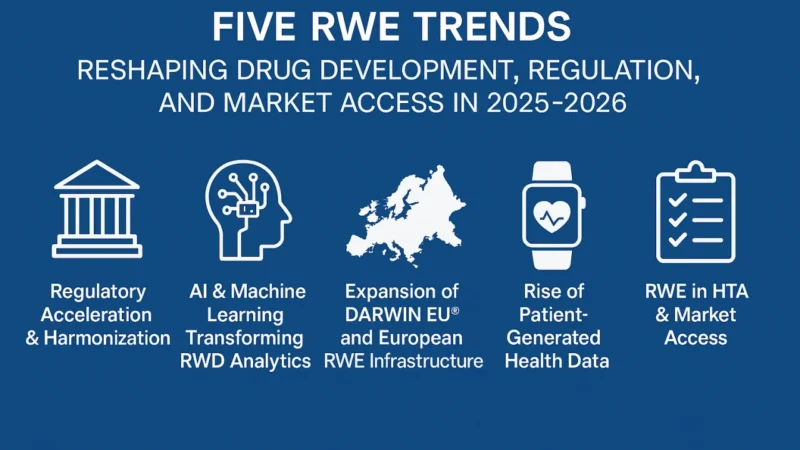
As we move deeper into 2026, five transformative trends are accelerating RWE adoption—and redefining what’s possible in drug development, safety monitoring, and value demonstration.
1. Regulatory Acceleration & Global Harmonization
Regulators are not just accepting RWE—they’re actively encouraging it.
In the U.S., the FDA’s RWE Framework, bolstered by provisions in the 21st Century Cures Act, continues to mature, with recent guidance clarifying how RWE can support label expansions, post-approval studies, and even pivotal evidence in select cases (e.g., rare diseases or oncology).
Across the Atlantic, the European Medicines Agency (EMA) has embedded RWE into its scientific advice process and is leveraging it through initiatives like the Big Data Steering Group. The MHRA in the UK and PMDA in Japan are similarly advancing their own frameworks.
Critically, there’s growing momentum toward international alignment. Collaborative efforts—such as those under the International Council for Harmonisation (ICH)—aim to standardize RWE methodologies, endpoints, and quality criteria. This harmonization reduces redundancy, lowers development costs, and creates a more predictable pathway for global submissions.
For sponsors: The message is clear—design your RWE strategy early, align with evolving regulatory expectations, and treat RWE generation as integral to your development plan—not an afterthought.
2. AI & Machine Learning: Unlocking the Full Potential of Real‑World Data
The volume, velocity, and variety of real-world data (RWD) have long outpaced traditional analytical approaches. Enter artificial intelligence (AI) and machine learning (ML)—now indispensable tools in the RWE toolkit.
Advanced algorithms are transforming unstructured data from electronic health records (EHRs), claims, social determinants, and clinical notes into structured, analyzable insights. Natural language processing (NLP) can identify disease progression or adverse events buried in physician narratives. Deep learning models predict treatment response or hospital readmission risk with increasing accuracy.
Beyond efficiency, AI enhances scientific rigor: it helps control for confounding, impute missing data, and simulate counterfactuals—bringing RWE closer to the causal inference standards of randomized trials.
The result? Faster signal detection in pharmacovigilance, earlier identification of high-value patient subgroups, and more agile clinical development.
But with great power comes great responsibility: robust validation, transparency, and bias mitigation remain non-negotiable. The industry must champion “responsible AI”—auditable, explainable, and ethically grounded.
3. Europe’s Federated Future: DARWIN EU® and the Rise of Integrated RWE Infrastructure
Europe is building one of the world’s most ambitious RWE ecosystems—and DARWIN EU® is at its heart.
Operationalized by the EMA, DARWIN EU® connects anonymized health data from over 181 million patients across 16 countries (as of their website checked today), enabling rapid, reproducible studies without moving raw data across borders—a critical advantage under GDPR.
This federated model preserves data sovereignty while delivering scalable, regulator-ready evidence. Recent use cases include drug utilisation studies, vaccine effectiveness, and natural of history of disease studies.
Looking ahead, DARWIN EU® is expected to integrate with national health data platforms (e.g., France’s Health Data Hub, Germany’s SMITH consortium) and link to patient registries, genomics databases, and digital health tools. The vision? A pan-European learning health system where evidence generation is continuous, collaborative, and policy-relevant.
For industry stakeholders: Engaging with DARWIN EU® isn’t optional—it’s a strategic imperative for timely European approvals and HTA submissions.
4. The Patient as Data Generator: Wearables, Apps, and PROs Redefine RWD
The definition of “real-world data” is expanding—literally—from clinic walls to everyday life.
Patient-generated health data (PGHD) from wearables (e.g., Apple Watch, Fitbit), mobile health apps, remote monitoring devices, and validated patient-reported outcome (PRO) tools are capturing continuous, granular insights into symptoms, adherence, functional status, and quality of life.
These data streams offer unprecedented temporal resolution—revealing patterns invisible in episodic clinic visits. For example, digital biomarkers from gait sensors can track Parkinson’s progression; sleep and activity metrics can signal early signs of depression or treatment toxicity.
Regulators are taking note: the FDA’s Digital Health Center of Excellence and EMA’s reflection papers on digital endpoints signal growing openness to PGHD in regulatory decision-making—provided data are validated, reliable, and clinically meaningful.
The shift isn’t just technological—it’s philosophical: placing the patient at the center of evidence generation.
However, challenges remain around data interoperability, equity (avoiding “digital divides”), and ensuring diverse representation. Inclusive study design and co-creation with patients will be key.
5. RWE as the Linchpin of HTA and Market Access
As healthcare systems face mounting cost pressures, demonstrating real-world value is non-negotiable.
HTA bodies—including NICE (UK), G-BA (Germany), HAS (France), and the pan-European joint clinical assessment (JCA) under the EU HTA Regulation—are increasingly demanding RWE to complement trial data on comparative effectiveness, long-term outcomes, and budget impact.
- RWE now informs:
- Pricing negotiations
- Risk-sharing agreements
- Coverage with evidence development (CED) schemes
- Post-launch performance monitoring
Crucially, the EU HTA Regulation mandates early dialogue between manufacturers and HTA bodies. Companies that delay RWE planning until Phase III—or worse, post-approval—risk delayed reimbursement or unfavorable pricing.
Forward-thinking organizations are embedding RWE into their value dossier development from Phase II onward, aligning endpoints with payer priorities and designing hybrid trial-RWE strategies.
Conclusion: Entering the Era of Strategic RWE
We’ve moved beyond the question of whetherto use RWE. The new questions are:
- How robust is your evidence?
- Is it fit-for-purpose across regulators, HTAs, and clinicians?
- Are you leveraging the full spectrum of data and technology available?
Finally, I would like to suggest 3 “i”s as drivers shaping the next phase of RWE: integration, intelligence, and impact
- Integrationacross data sources, functions, and geographies
- Intelligencepowered by AI, analytics, and methodological rigor
- Impacton patient outcomes, access, and sustainable innovation.”
More from Massoud Toussi on OncoDaily.


