Douglas Flora, Executive Medical Director of Yung Family Cancer Center at St. Elizabeth Healthcare, President-Elect of the Association of Cancer Care Centers, and Editor in Chief of AI in Precision Oncology, shared a post on LinkedIn:
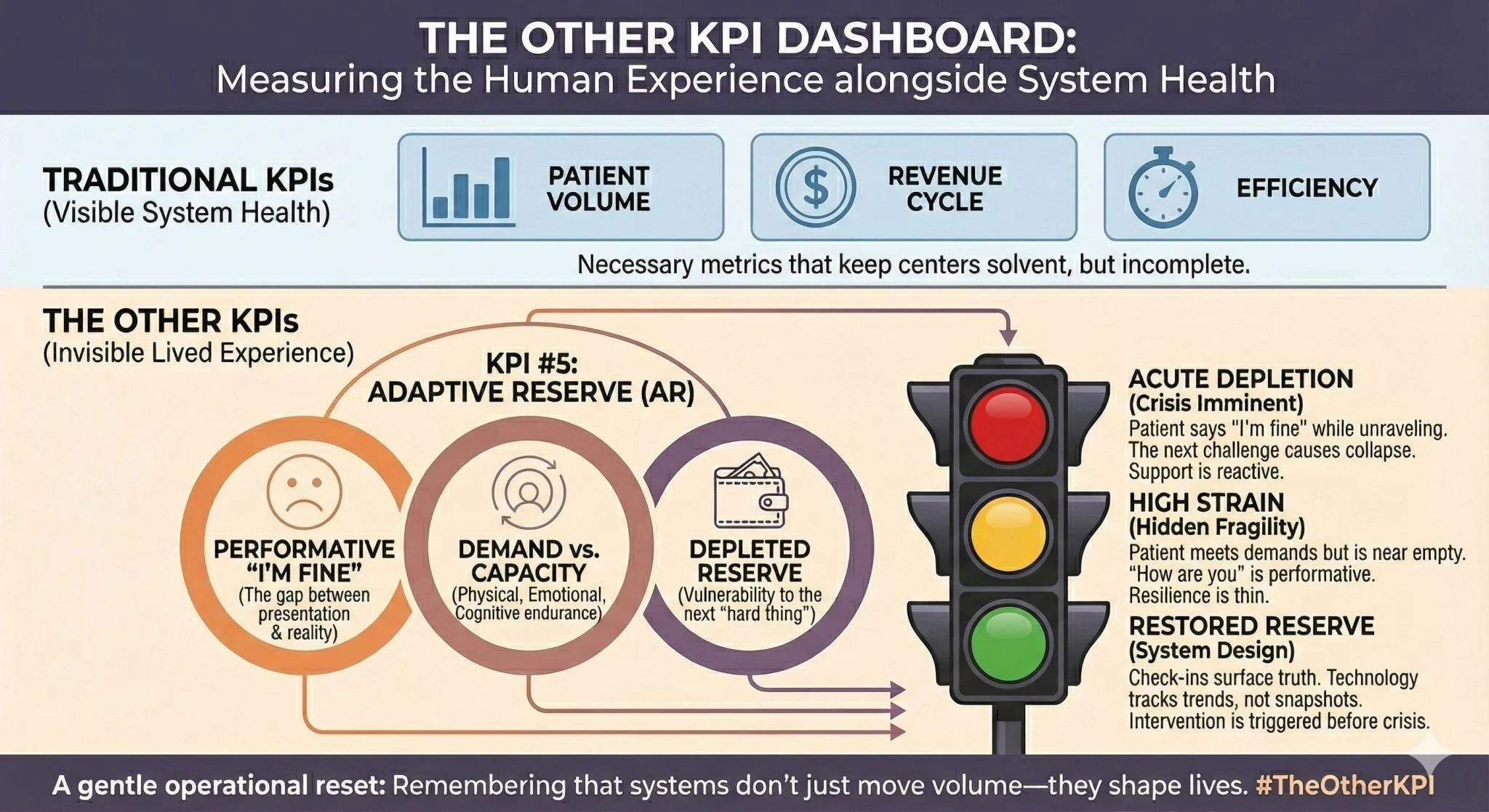
“THE OTHER KPI 5: ADAPTIVE RESERVE (AR)
Continuing our series on hospital KPIs I wish we followed—from a cancer doc and cancer patient’s perspective.
“I’m fine” is often the least truthful thing a cancer patient says.
Oncology has gotten remarkably good at measuring disease.
Tumor markers. Response rates. Progression-free survival. These matter. They guide treatment. They predict outcomes.
But there’s another kind of measurement we rarely attempt.
Adaptive Reserve (AR): the gap between how a patient presents and their actual capacity to keep going.
Every oncologist has seen it. The patient who says “I’m fine” while their hands shake. The caregiver who insists ‘we’re managing’ while visibly unraveling. The family that nods understanding while terror fills the silence.
We chart their weight. Their performance status. Their reported pain on a scale of one to ten.
We don’t chart the ratio of terror to determination. Grief to hope. What’s being demanded versus what remains in reserve.
This matters because cancer care makes enormous asks.
Physical endurance through treatment. Cognitive capacity to understand options. Emotional resilience through uncertainty. Financial stability under pressure. Social support that doesn’t collapse.
Most patients say yes to all of it. Even when their reserve is nearly gone.
As both oncologist and patient, I learned: the answer to “how are you doing” is almost always performative.
The real question is: how much adaptive reserve remains? What happens when the next hard thing arrives—because in cancer, it always does.
This is measurable. Not perfectly. But meaningfully.
Regular check-ins designed to surface truth rather than reassurance. Validated screening tools for distress, financial toxicity, caregiver burden. Clinical intuition given permission to override reported status.
Technology can help. Patient-reported outcomes that track trends rather than snapshots. Predictive models that notice when reserve is depleting before crisis hits.
But the real work is cultural. Creating space for patients to stop performing. To admit they’re not fine. To ask for help before they break.
What if adaptive reserve appeared on our treatment planning discussions? Not as a soft metric. As essential data.
What if depleted reserve triggered intervention the way depleted blood counts do?
Patients would get support before catastrophe. Clinicians would make better decisions about treatment intensity. Families would know when to mobilize help.
The system would work better. Care would feel more human.
Last call: what Other KPI do you wish your organization measured and actually addressed?
Share it below. I’m compiling everything for next week’s reflection.
Let’s build a dashboard that reminds us why we’re here. Then make 2026 the year we actually use it.”
More posts featuring Douglas Flora.