Bernard Fox, Co-founder, President, and CEO of UbiVac, shared highlights from Immunotherapy Bridge 2025 on LinkedIn:
“Prof. Paolo A. Ascierto opens Immunotherapy Bridge2025!
My High level takeaways!
Tomas Kirchhoff, New York University – I did not know any of this.. interesting data showing a correlate with mitochondrial haplotype T and resistance to nivolumab 15% RR vs the standard 45+%. Interestingly, the stronger binder pembrolizumab gives much higher RR.
Eric Vivier, Innate Pharma Marseille Immunology Biocluster Paris Saclay Cancer Cluster (PSCC) –
1) lots of insights into 3 subsets of NK cells – NK1, NK2, and NK3.
2) Also described updates to their Ab NK engagers / tri and tetra NK engagers.
3) Their phase III trial of monalizumab – with AstraZeneca reads out next year
Tullia Bruno at UPMC talks B cells: Great background on role of B cells in anti-cancer immunity and that of TLS. Reviewed historical data on TLS and improved outcome. Went onto studies in Ovarian Cancer and ways B cells can be educated outside the TLS.
Jennifer Guerriero, PhD gave great talk with lots of new data – Labelled Do not post. Wanted to post – image of there is more to Mac’s than M1 & M2. Please to better characterize Macs beyond simplistic M1/M2 designation. Went onto studies to talk about CAR- Monocytes that have increased lifespan and traffic to tumor. Nice work and promising data!”

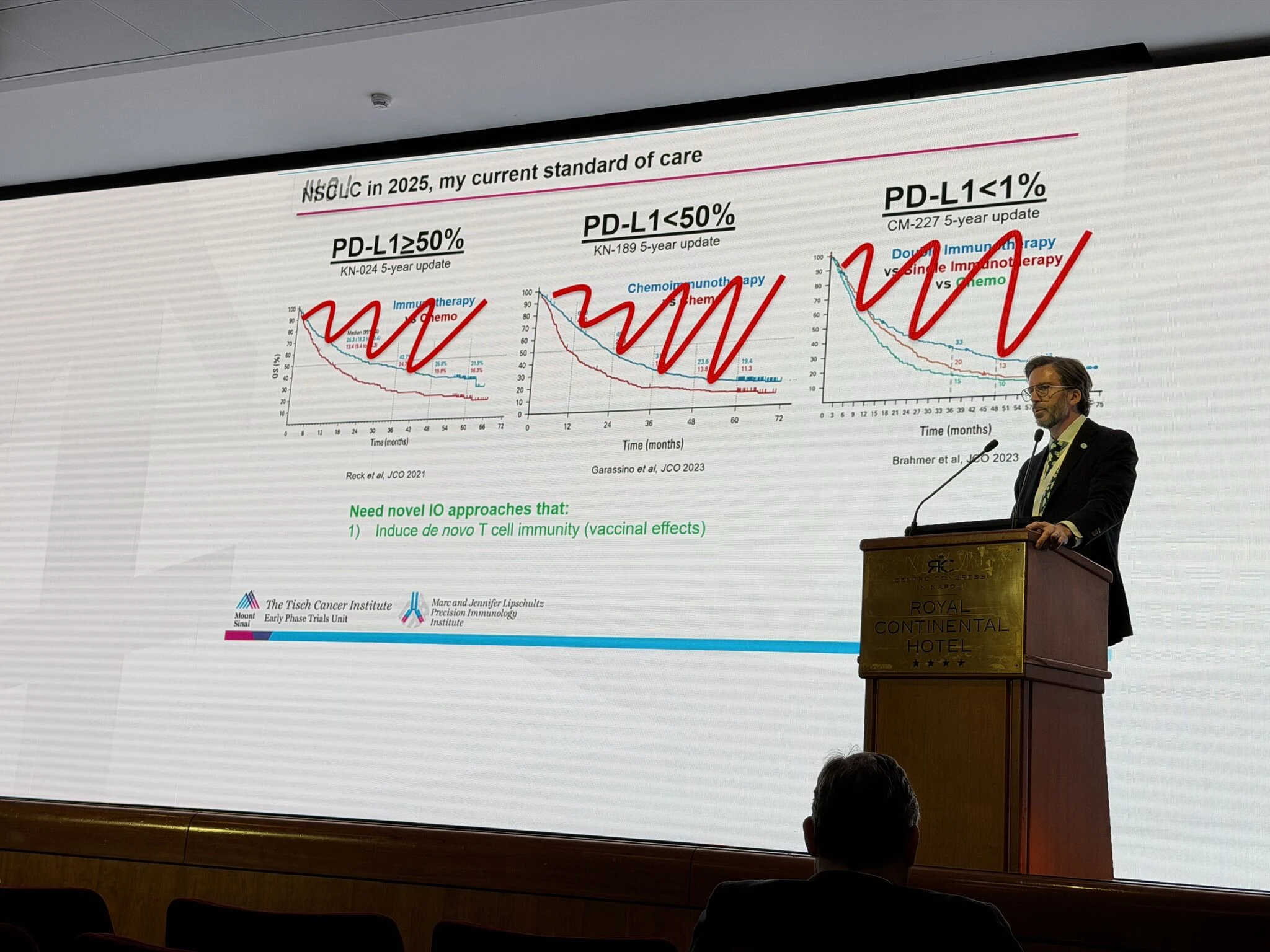
“Prof. Thomas Marron at Icahn School of Medicine at Mount Sinai
My high level takeaways
Hats off to Dr. Marron for attacking hepatic cancer metastases.
Provided a great intro to role of IL-4 in driving type 2 immune responses
Also discussed IL1 and tha anakinra failure..
Got into background and design of current trials..
In preclinical models: Activated macrophages mediate resistance to checkpoint blockade – anti-IL4 reverses this. They have moved this to clinical trials..
I am very excited about their current combination immunotherapy clinical trials for patients with tumors in the liver – THE SITE WHERE T CELLS GO TO DIE! We need good, innovative, well-monitored studies in this disease.
The’s The slides were listed as unpublished – DO NOT POST – so I am not posting.
If I had colon cancer liver Mets I would check out their trials..”
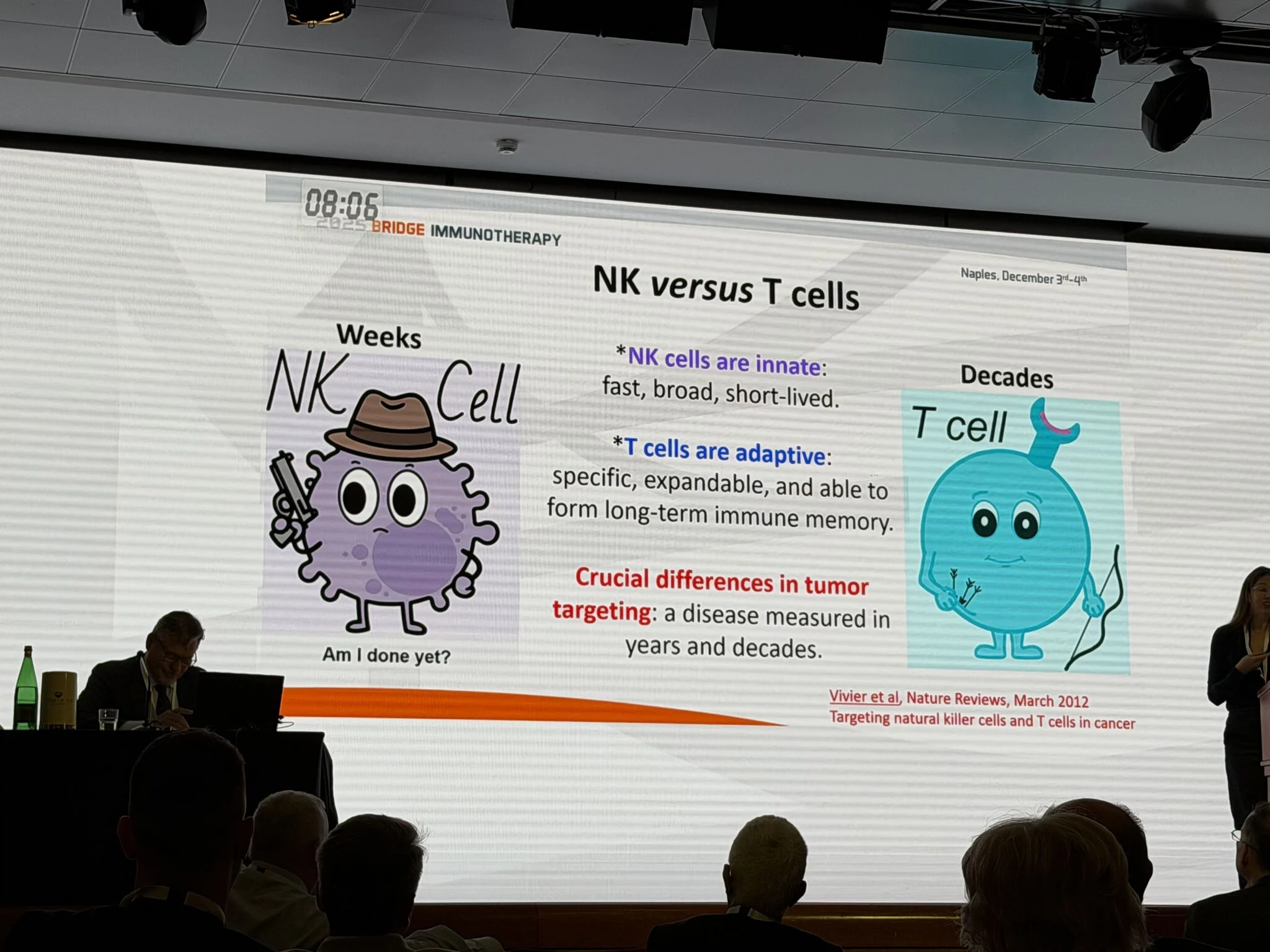
“Prof. Chrystal Paulos & Dr. Tim Lu
Provide an entertaining and educational background and numerous arguments in support of their premise!
“Targeting T cells versus NK cells”
My Takeaway – T cells cure but “off-the-shelf” NK cells can play a critical role – particularly in AML!
More at ASH2025.”
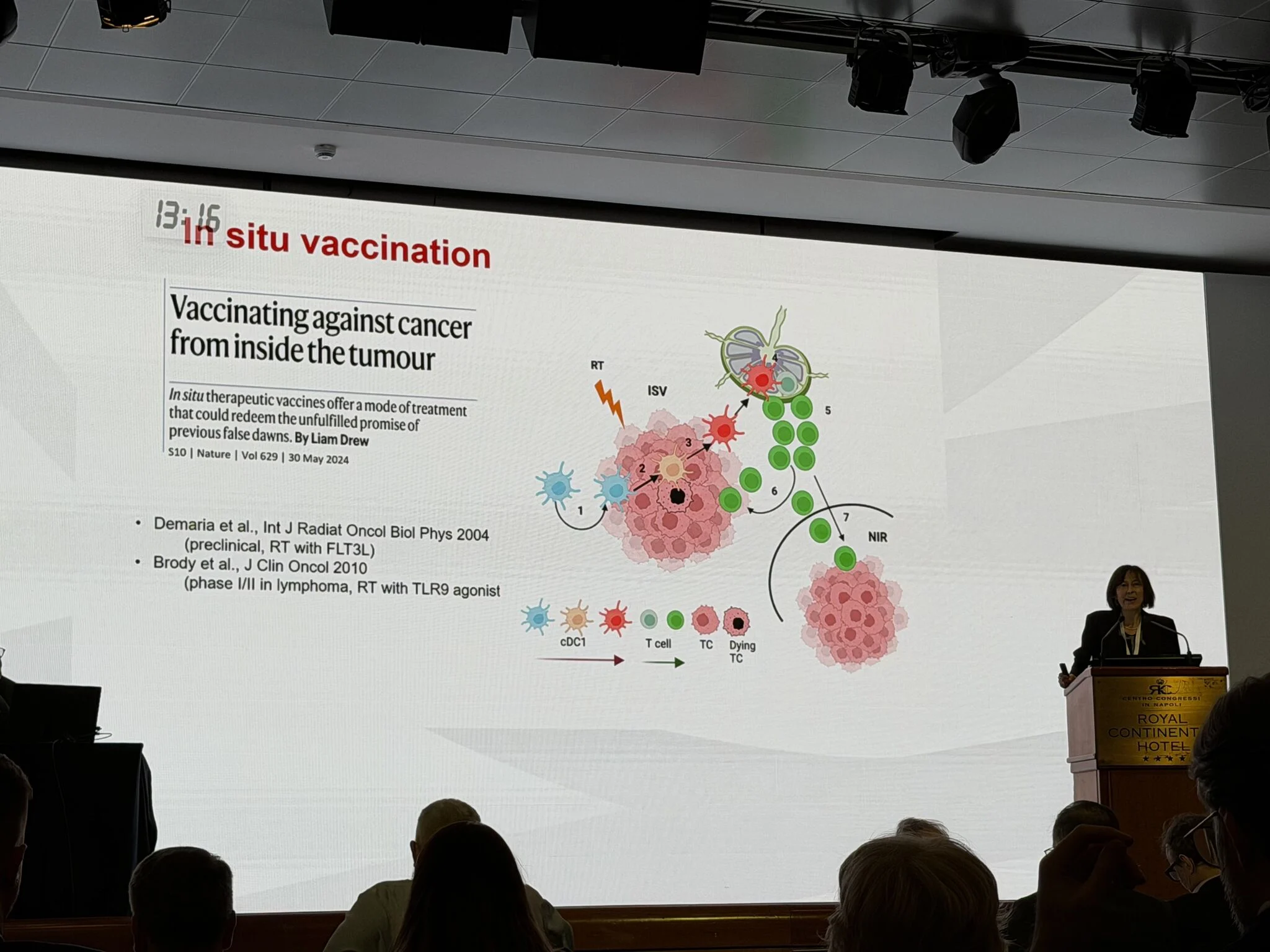
“Prof. Sandra Demaria at Weill Cornell Medicine talks on impact of oncogenic alterations on radiation induced anti-cancer T cell responses / much is do not post..
Radiation induced cGAS/STING increasing tumor immunogenicity & immune response, but it can also have negative effects.
Lots more covered in slides.”
“Prof. Roberta Zappasodi discusssed the relationship between tumor glycolysis, angiogenesis, and immune responses in human tumors and suggested how this might be modified to increase effectiveness of immunotherapy. Used 4T1 preclinical model as a basis. Really nice work – But.. MAJORITY OF SLIDES “DO NOT POST” – ya gotta come to Napoli!”

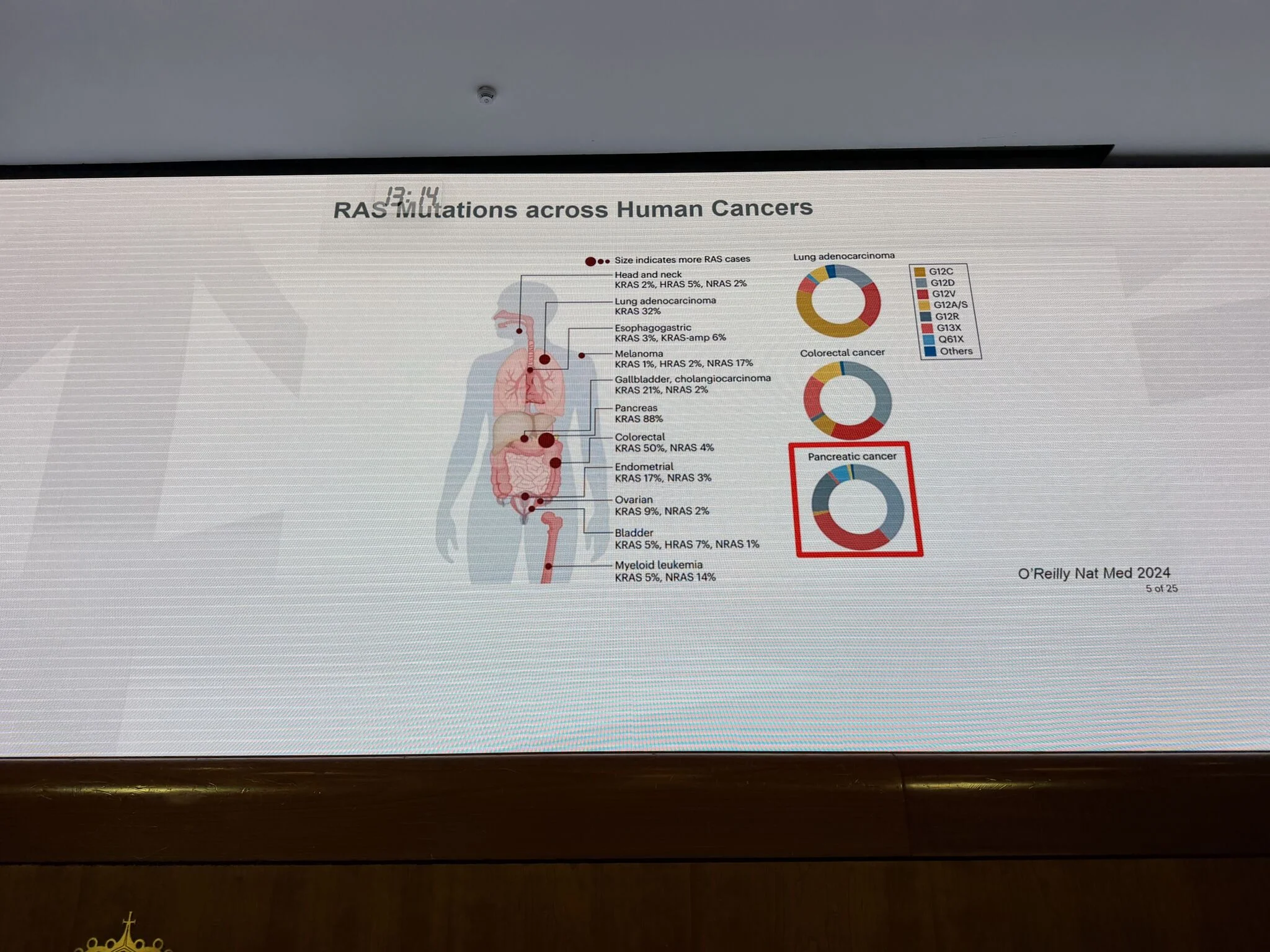
“Dr Tim Heffernan provides a great talk on KRAS and impact of small molecule inhibitors on the immune response!
Great story..
Lots of data –
Reviews drugs in clinic.
Lots of agents..
KRAS inhibitors, ~80% disease control rate but progress at ~8 months
Preclinical modeling –
KRAS drives immunosuppression!
combo with anti-PD-1 doesn’t help. Anti-CTLA-4 works GREAT.. Has impact on Tregs.
Does it also have effect on priming??
Very cool impact of combo on development of TLS.
Where is the clinical trial of the combo?”
“Dr Giusy Gentilcore immunomonitoring expert at Sidra Medicine shows lots of data on kids with AML..
Dr Gentilcore covered Immuno-profiling of Pediatric Cohort of Patients Affected by Acute Lymphoblastic Leukemia in the Middle East: A Step Towards Precision Medicine
Takeaways:
1) Immune microenvironment shifts toward immunosuppression during treatment.
2) Clinical correlation is needed to assess prognostic relevance.
3) Dynamic TME reveals potential biomarkers.”

“Prof. Cristina Maccalli Maccalli – Genoa
Deep characterization of CD19-CAR-T cells upon engagement of the CARs
Takeaways:
> UCB (umbilical chord blood) can represent an appealing source of T lymphocytes to generate off the shelf” CAR cells;
• CD19-CAR-T cells can be efficiently isolated from UBC exerting in vitro and in vivo anti-tumor activity;
› The functional and transcriptomic analysis can reveal different sub-populations of CAR-T cells endowed with variable profile.
Interestingly, differential phenotype, molecular and functional profile are detected upon antigen specific
stimulation of CD19-CAR-T cells activated with Beads vs. T cell TransAct.
* Superior pro-inflammatory profile was detected in PBMC vs. UCB-derived CAR-T cells, indicating the lower risk of CRS and other toxicities by UBC-CAR-T cells
* The deep genomic (scRNAseq) and metabolomic profiling of CAR-T cells upon the antigen-specific engagement of the
CD19-CAR reveals molecular and functional features that cannot be identified in resting CAR-T cells and lead to the identification of target genes for ad hoc genetic manipulation (gene editing) of off-the-shelf CD19-CAR-T cells.”
“Prof. Gregory Lesinski cancer immunologist Extrordinaire Emory University School of Medicine give a wonderful talk on their efforts to CURE pancreatic Cancer – This talk focused on role of IL-6
What is the I mpact of Dual IL-6/PD-1 Blockade in Patients?
• 1. Impact of IL-6/PD-1 blockade on fibroblast populations?
• 2. Do we see a similar degree of T cell infiltration in patients as we did in murine models?
• 3. What is the nature of the T cells?
• 4. Does IL-6 blockade modulate the Myeloid component
Findings:
Metastatic Human PDAC Harbors:
Fewer T cells; Those present are highly suppressed
– More CD68+CCR2+ TAMs
– Fewer CAFs and less collagen
– Trend toward more B cells
Conclusions and Future Directions
– Dual IL-6/PD-1 blockade is safe and feasible as a therapy in heavily pre-treated patients with metastatic PDAC.
• The metastatic PDAC TME is particularly hostile for T cells!
– Many strategies to invigorate the metastatic PDAC TME
• KRAS inhibition to reprogram the PDAC TME?
• Vaccine approaches to elicit endogenous T cell response?
• Adoptive Cellular Therapy to introduce tumor-Ag specific T cells?
• Could IL-6 or other cytokine modulatory therapies play a role earlier in disease intervention or in selected populations?”
“Prof. Myriam Chalabi cancer immunotherapy expert at The Netherlands Cancer Institute
BEYOND MSI HIGH!!!
Very cool ! Saw a response in Undifferentiated pleiomorphic sarcoma – see scans
Key take-aways
• Short course neoadjuvant ICB is extremely effective in dMMR colon cancers and is associated with excellent long-term outcomes
• Optimal combinations, duration of treatment and organ preservation
• ICB is effective in a subgroup of pMMR colon cancers
• Validation of potential predictive (attainable) biomarkers in future trials
• Additional avenues →
- Modulation
- Chemotherapy
- Targeting
- Immunosuppression
- Novel treatments
• Potential neoadjuvant ICB in non-CRC dMMR and pMMR tumors ongoing.”
“Prof. Andy Futreal rare cancer expert at MD Anderson Cancer Center gives a great talk on development of treatment strategies for patients with rare cancers.
Interesting concept – should we think about “Pan Rare Cancer” eg.. maybe hot vs cold..
WHAT ARE RARE CANCERS & WHAT ARE THR PROBLEMS?
WHO Rare Cancer definition: <6 per 100,000 individuals
›Patients with rare cancers experience challenges in diagnosis accuracy, treatment delays, later stage diagnosis compared to common cancers, and have lower 5-year survival compared to those with common cancers. 1,2
› Represent nearly 25% of all new cancer diagnoses & cancer deaths, annually.?
-Development of new therapeutic options stymied by pharma neglect, limited trial numbers, and siloed research efforts.
> Fragmented nature of existing research efforts and the scarcity of comprehensive data hinder collaboration and slow progress
>Requires considerations of histology agnostic therapeutic development
• Limited by availability of high quality and quantity contemporary “omics” data
—
Immunotherapy in sarcomas – loud and quiet ( HOT AND COLD TUMORS)
• SARCO28 – ORR: UPS 40% (4 of 10) and DDLPS 20% (2 of 10)
• Complex, highly copy number and rearrangement altered genomes
– further studies corroborating
• Alveolar soft part sarcoma ORR: 73% (64 of 88, pooled analysis)
• Pathognomonic der(17)t(X;17)(p11;25), usually unbalanced translocation giving rise to an ASPSCR1::TFE3 fusion gene, little else
• Angiosarcoma – ORR 25-59%, hight.”

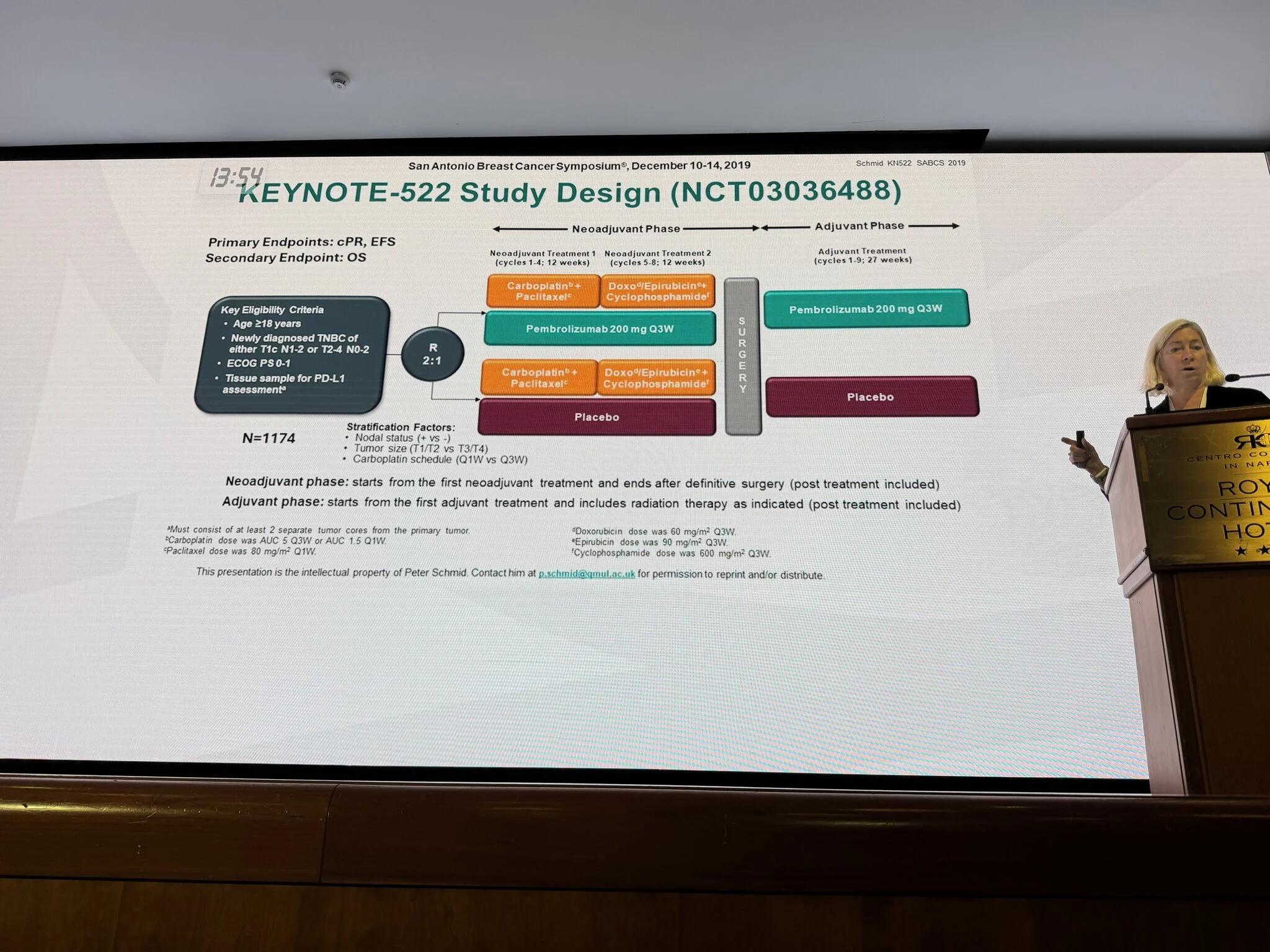
“Prof. Leisha A. Emens, MD PhD breast cancer immunotherapy
Guru Calico Life Sciences reviews standard of care for Triple Negative Breast Cancer ( TNBC )
Current State: Neoadjuvant Immunotherapy for TNBC
The addition of pembrolizumab to standard neoadjuvant chemotherapy, followed by pembrolizumab to complete one year is approved by the FDA as standard of care for high risk early TNBC regardless of PD-L1 status
• Side effects are consistent with those of the individual drugs
• Adrenal function should be evaluated prior to surgery
Questions:
• Biomarkers of response, resistance, toxicity
• Patient selection for de-escalation to surgery alone, neoadjuvant chemotherapy without immunotherapy
• Patient selection for carboplatin with AC/T and immunotherapy
• Optimal management of patients who do not achieve a pCR: capecitabine, PARPI, additional immunotherapy, other
• Optimal duration of immunotherapy in distinct patient populations based on risk analysis, pCR
• Chemotherapy-free immunotherapy
• Novel IO Combinations
–
SEE BIOMARKERS SLIDE
SEE NEW TREATMENTS SLIDES
GREAT DATA WITH ADC
–Sacituzumab
Overall Conclusions
• For the patient, neoadjuvant therapy affords multiple advantages over upfront surgery followed by systemic therapy
-down-staging to minimize the extent of surgery
-de-escalation of radiotherapy
-pCR/ctDNA-based de-escalation or escalation of systemic therapy
-prompt initiation of systemic therapy
• PCR correlates with improved long-term clinical outcomes at the patient evel but not the trial level
• Adaptive neoadjuvant (platform) trials can accelerate drug development by rapidly evaluating novel agents relative to the standard of care
• Novel combinations with potential to improve outcomes are emerging
• Chemotherapy-free neoadjuvant regimens are promising for patients selected for immune-activated disease
–ipilimumab +nivolumab
–datopotomab + durvalumab
–Sacituzumab + pembrolizumab?”
“Prof. Liz Burton, PhD, MBA drug development expert at MD Anderson Cancer Center reviews timeline of immunotherapy approvals for melanoma – GREAT Review OF LAG3 data and outlines CD276 / B7H3
Lots of great slides
Conclusions
• Neoadjuvant platform continues to provide valuable insight into biomarkers associated with outcomes.
• In melanoma: Neoadjuvant nivo + rela demonstrates durable benefit for patients after 4 years and High B7-H3 at baseline is associated with poor pathologic response and recurrence
• In non-responders, in addition to tumor cells, B7-H3 is expressed by cancer-associated fibroblasts (CAFs), monocytes, and macrophages in spatial analysis
• In responders, spatial analysis reveals tissues have higher frequencies of LAG3+ and TIGIT+ CD&+ T cells at baseline
• Biomarkers associated with pathologic response and favorable clinical outcomes (INy and B Cells) in the context of anti-PD1 +/- anti-CTLA-4 are also seen in some cohorts with anti-LAG-3 treatment.
• LAG3+ at baseline also associated with MPR
• Immunotherapy clinical development and translational insights need to be dramatically accelerated.”
More posts featuring Bernard A. Fox on OncoDaily.


