Anas Younes, Senior VP, Global Head of Hematology (Early and Late Stage), Oncology R&D at AstraZeneca, shared a post on LinkedIn:
“In hematology, we’ve seen incredible progress over the past decade, yet for many patients, the need for more efficacious and tolerable treatments remains. At AstraZeneca, we’re working to translate scientific advances into therapies that could change what it means to be diagnosed with blood cancers. Core to our efforts are approaches that aim to harness the immune system to recognize and eliminate cancer cells.
At the American Society of Hematology (ASH) annual meeting 2025, the AstraZeneca team will share new data that reflects two of the most exciting areas in hematology: T cell engagers (TCEs) and cell therapy.
Evolution and Innovation of T Cell Engagers
TCEs represent a fundamental breakthrough in immunotherapy. These multispecific antibodies are engineered to bring a patient’s T cells into direct contact with cancer cells, enabling the body’s own defenses to recognize and eliminate the tumor. Our ambition is to extend their potential beyond current indications to a broad spectrum of blood cancers where unmet needs remain high.
The evolution of TCEs tells a story of continuous innovation. First-generation therapies, which activate the immune systems T cells via the CD3 receptor, that is found on the surface of all T cells, have been foundational. However, widespread activation of T-cells can cause unwanted side effects including cytokine release syndrome (CRS), which is dose-limiting and requires close inpatient monitoring.
Second-generation TCEs have brought molecular refinements such as attenuated CD3 binding, designed to reduce CRS by weakening the connection between a therapeutic antibody and the CD3 protein while maintaining potent anti-tumor activity. Alongside this, novel approaches in the clinic are helping to mitigate side effects. Step-up dosing protocols to gradually prime the immune system and prophylactic co-medications* are helping transform TCEs into therapies that could potentially be tolerable in outpatient settings, aiming to bring care close to patients and reduce the treatment burden.
But the innovation doesn’t stop there. We’re aiming to build upon the current work on TCEs with our Target Induced T-cell Activating Nanobodies (TITANs) platform, designed to selectively engage CD8+ T-cells, which have the greatest potential to fight cancer. With TITANs, we aim to deliver a highly targeted immune response against cancer.
With the improvement of generally tolerable TCEs comes the opportunity to combine them with other modalities, such as antibody-drug conjugates (ADCs), a type of targeted therapy, which may drive deeper, more durable responses.
Cell Therapy: Beyond the First Wave
While CAR T therapy has improved outcomes for some patients living with relapsed/refractory disease, studies indicate that only approximately 25% of eligible patients receive these treatments due to high costs, lengthy manufacturing timelines and complex infrastructure (i).
Expanding access requires a multi-pronged approach, including enhanced manufacturing processes, the ability to deliver CAR Ts at scale, and health system readiness. Bringing cell therapy into the outpatient and community setting will also be critical to support widespread adoption. Early reports demonstrate that transitioning CAR T therapy to the outpatient setting is feasible, a shift that could be further enabled by the development of well-tolerated treatments with predictable safety profiles, alongside technologies that support remote patient monitoring.
A key area of focus at AstraZeneca is bringing the potential of cell therapy to more people living with multiple myeloma, the second most common blood cancer.
Our data at ASH will highlight the promise of our FasTCAR technology, which aims to shorten manufacturing timelines to deliver higher quality T cells and potentially more effective therapies. Unlike conventional CAR T production, where lengthy replication in the laboratory can cause T cell exhaustion and reduce cancer-fighting activity, early data suggest that FasTCAR‘s rapid manufacturing andin vivo expansion keeps T cells “fitter” (younger and less exhausted) (ii).
This progress brings us closer to a future where autologous cell therapies (created using a patient’s own T cells), once limited to specialized hospital settings, could be delivered within community treatment centers, reducing wait times and potentially improving access for patients who urgently need therapy.
Looking ahead, I am particularly excited at the promise of allogeneic andin vivoapproaches. These emerging modalities could transform cell therapy into mainstream care, helping with the aim of delivering scalable, off-the-shelf treatments that are more accessible, reach patients faster and are less burdensome.
The Path Ahead
Progress in hematology isn’t measured just by the molecules we develop. It’s defined by impact on people’s lives. We’re seeing a fundamental shift away from hospital-intensive, last-line treatments toward earlier, scalable and more patient-centric options. We’re committed to transforming hematologic care, which means aiming to reduce treatment burden, advocating for greater access to medicines and ultimately enabling patients to spend fewer days in hospital and more time living their lives.
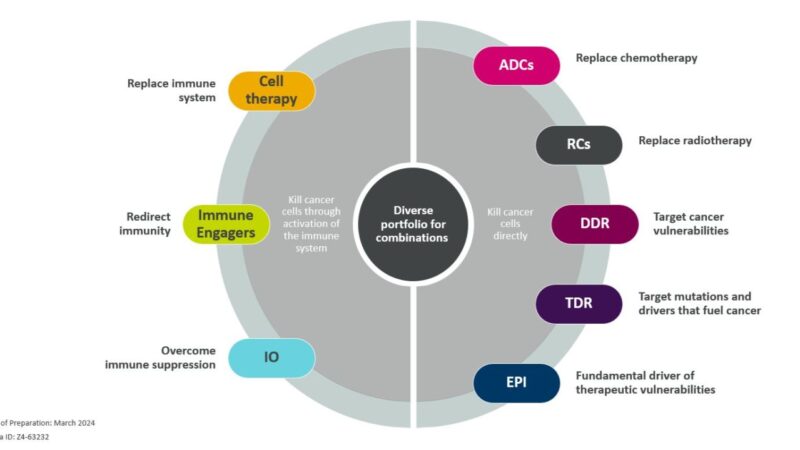
TCEs and cell therapy are just two modalities helping to shape the future of hematology. At AstraZeneca, we’re advancing a diverse toolkit that includes ADCs, small molecules and epigenetic modulators, each offering their own individual mechanisms to help combat the heterogeneity of blood cancers. In a future blog, I’ll explore how courage and calculated risk-taking are essential to developing these breakthroughs, and why progress in hematology requires not just brilliant science, but the boldness to pursue it.
[1] Kourelis T, Bansal R, Patel KK, et al: Ethical challenges with CAR T slot allocation with idecabtagene vicleucel manufacturing access. J Clin Oncol 40, 2022 (16_suppl; abstr e20021)
[2] Zhang, C., He, J., Liu, L. et al: Novel CD19 chimeric antigen receptor cells manufactured next-day for acute lymphoblastic leukaemia. Blood Cancer J 12, 2022
*Medicines taken in advance of a primary treatment to prevent or reduce anticipated adverse effects or complications associated with that treatment.”
More posts featuring Anas Younes on OncoDaily.


