Achyut Saroj, Founder, Consultant, and Author at AwareOnc, KOL Engagement and Medical Affairs Liaison at Tatva Health, shared a post on LinkedIn:
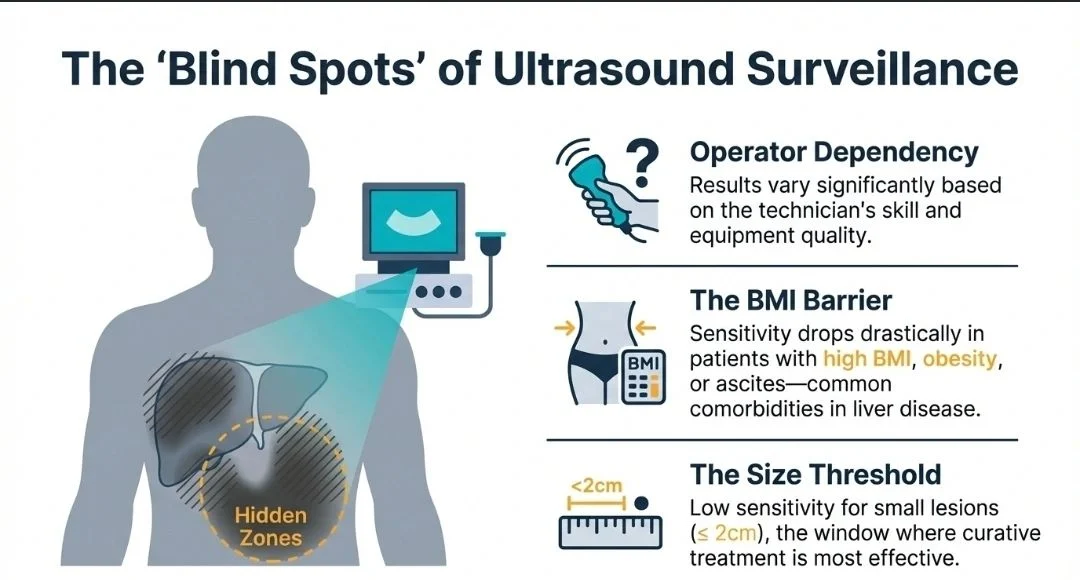
“The Blind Spot of Ultrasound Surveillance in Early-stage HCC
Are we missing early-stage Hepatocellular Carcinoma (HCC) because of the inherent limitations of our current surveillance tools?
While ultrasound is the current standard of care for HCC surveillance, it has significant ‘blind spots’ that can lead to delayed diagnoses. According to the evidence, these limitations include:
1) Low Sensitivity for Small Lesions:
Ultrasound has a notably low sensitivity for lesions < 4 cm and often fails to detect very small lesions < 2 cm.
2) Patient Factors:
Ultrasound is significantly less effective in patients with a high BMI.
3) Operational Barriers:
Ultrasound accuracy varies with the operator’s skill and the quality of the equipment. Additionally, the need for specialized imaging centers can lead to poor patient adherence.
Liquid biopsy tests like HelioLiver Dx are designed to solve these blind spots.
By combining cfDNA methylation patterns, serum protein markers (AFP, AFP-L3%, and DCP), and patient demographics, this simple blood test offers a more comprehensive view of a patient’s risk.
The CLiMB trial (NCT03694600), the largest prospective multi-center blinded study of its kind in the U.S., demonstrated the clinical superiority of this approach:
1) Superior Sensitivity:
HelioLiver was proven to be 4X more sensitive to smaller T1 lesions (most treatable) than ultrasound.
Ultrasound failed to detect any tumors <2 cm, whereas HelioLiver showed 28.6% detection sensitivity for the same size.
2) Early Detection:
It showed superior sensitivity for detecting HCC lesions < 4 cm and remained effective regardless of the patient’s BMI or the etiology of their cirrhosis.
3) Increased Adherence:
Because it only requires a simple blood draw that can be integrated into routine check-ups, it removes the accessibility barriers associated with imaging centers.
Early-stage patients have significantly better outcomes, with 5-year survival rates of over 70% compared to less than 1.5 years for those diagnosed at a late stage.
It is time to advocate for diagnostic tools that provide the adherence, accessibility, and early detection our high-risk patients deserve.”
More posts featuring Achyut Saroj.


