Achyut Saroj, Founder, Consultant, and Author at AwareOnc, KOL Engagement and Medical Affairs Liaison at Tatva Health, shared a post on LinkedIn:
“What gastritis taught me about Liver Cancer?
Early in my research career (PhD and Postdoc fellowship at NCI), I spent years studying how cancer actually develops, not as a sudden event, but as a slow, predictable process.
In gastric disease, the pattern was clear: chronic inflammation leads to precancerous changes, then ulcers, and eventually gastriccancer.
That same pattern is impossible for me to ignore when I look at hepatocellular carcinoma (HCC).
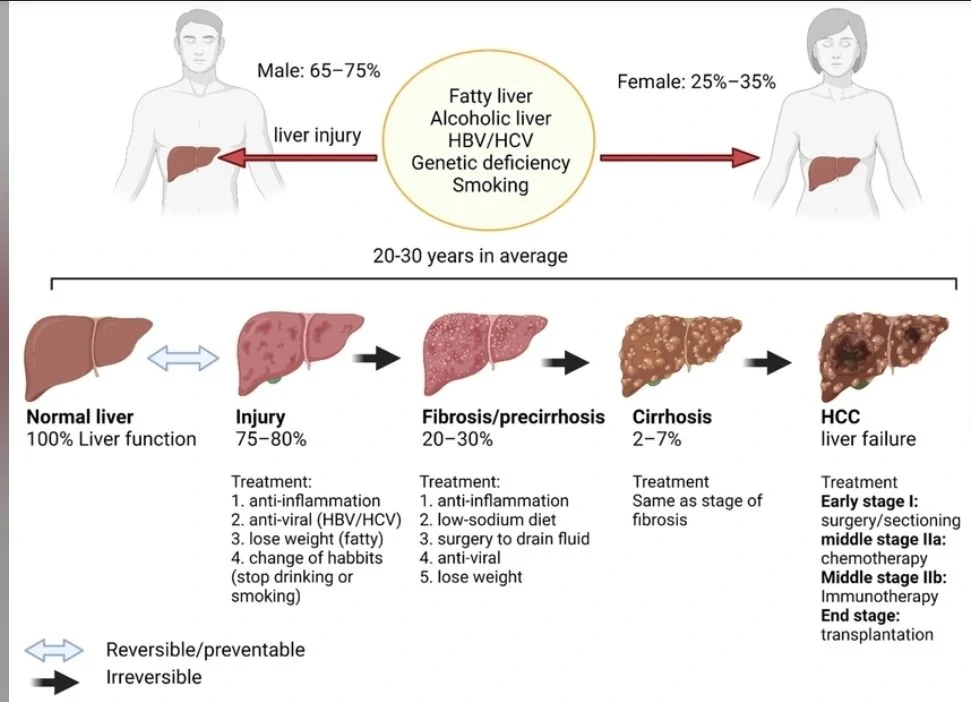
HCC rarely appears out of nowhere. It grows out of long-standing liver injury, fibrosis progressing to cirrhosis, often in patients we already know and follow. Viral hepatitis (B&C), NASH (now called MASH), alcohol-related liver disease (and metabolic dysfunction-associated fatty liver disease MAFLD).
These patients don’t enter the system late. The cancer does.
Fibrosis and cirrhosis aren’t just scars. They actively reshape the liver, altering signaling pathways, driving genomic instability, and creating an environment where malignant clones can emerge long before a tumor is visible on imaging.
This is why early detection matters so much in HCC.
We’ve relied heavily on ultrasound for surveillance, and while it has value, its limitations are well known in day-to-day practice. Image quality depends on the operator.
Sensitivity drops in obese patients and in nodular cirrhotic livers. And in many community and safety-net settings, access to consistent, high-quality ultrasound simply isn’t guaranteed.
The result is predictable: earlydisease is missed, and HCC is often diagnosed when cancertreatment options are already limited (especially second line).
Where do we go from here?
Liquid biopsy offers a way to align detection with the biology of this disease. Molecular changes, particularly methylation and fibrosis-associated signals, emerge well before a mass forms or sheds large amounts of tumorDNA (ctDNA). Detecting those signals means identifying risk and transformation earlier, not just confirming advancedcancer.
Science is moving in that direction. What lags is adoption.
If we’re serious about improving outcomes in HCC, especially in community and underserved populations, we need cancersurveillance tools that are less operator-dependent, more scalable, and better matched to how this cancer actually develops.
My years studying the inflammation-driven progression of gastric disease have shaped how I think about early diagnosis. HCC reinforces that lesson every day: waiting for a tumor to appear on imaging is often waiting too long.
How can you relate this to your experiences with cancer?”
More posts featuring Achyut Saroj.


