Shahrin Ahmed, Medical Specialist at the Canadian Cancer Society, shared on X:
“Pancreatic cancer awareness – MED12 is identified as being instrumental in basal-like pancreatic cancer.
MED12 is a significant regulator of the basal cell state in this disease, as revealed by this approach.
Basal-like PDAC cells’ growth is more susceptible to loss of MED12 than those without basal characteristics, according to this study.
The biochemical interaction that maintains basal identity in human cancer, which can be targeted for tumor lineage-directed therapeutics, has been revealed through our genetic screens.
The pancreatic cells are the starting point for pancreatic cancer. Malignant tumors are a group of cancer cells that can invade and destroy nearby tissue. It is capable of spreading (metastasizing) to other parts of the body.
The duct that connects the pancreas and the digestive system. Ductal adenocarcinoma of the pancreas is the name given to this type of cancer. Ductal adenocarcinomas account for about 95% of all pancreatic cancers.
Pancreatic cancer remains a significant health challenge worldwide due to its aggressiveness and lethality. Among all cancer types, it is the third-highest contributor to cancer-related mortality.
The tumor microenvironment (TME) and cancer cells have a complex relationship that leads to tumor growth and treatment resistance.
Cancer-associated fibroblasts (CAFs) control the processes of tumor growth, immune evasion, therapy resistance, and ECM remodeling in the TME. As a result, boosting the efficacy of pancreatic cancer therapy can be achieved through targeted modulation of CAFs.
In the United States, pancreatic cancer accounts for approximately 3.3% of all cancers. Cancer is the 10th most common cause of death among men and people who were born male, while it is the 8th most common cause of death among women and people who were born female.
There are an increasing number of cases of pancreatic cancer. By 2030, it is projected that pancreatic cancer will become the second leading cause of cancer death in the United States, according to trends.
In the United States, the percentage of people who survive five years after being diagnosed with pancreatic cancer is 11%. This signifies that 11 out of 100 individuals remain in good health five years after their diagnosis.
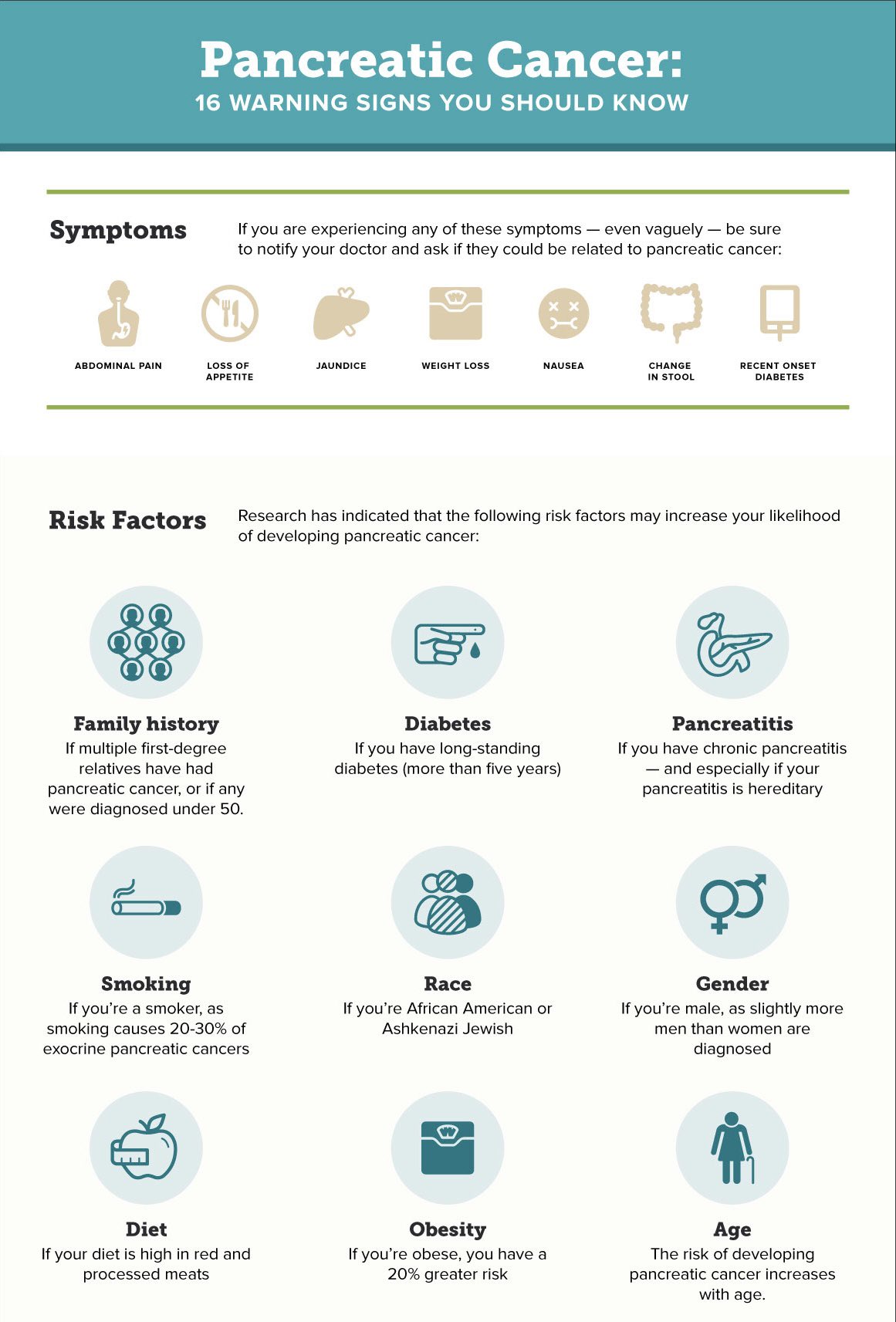
Routine screening for pancreatic cancer is not typically done by healthcare providers.
In individuals who have a genetic predisposition that increases their chances of developing pancreatic cancer, providers recommend regular monitoring through imaging tests and endoscopic ultrasounds.
It’s essential to go through the screening process. Mutations in genes BRCA1 and BRCA2 can occur in individuals who have pancreatic cancer Mutations in BRCA1 and BRCA2 are not only associated with breast cancer, but also with prostate, ovarian, and pancreatic cancer.
If you’re related to someone who has pancreatic cancer as either a parent, child, or sibling, you may want to consider genetic testing. If you have a BRCA1 or BRCA2 gene mutation, your results can provide information about it.
It’s important to remember that having the mutation does not necessarily mean you will develop cancer. Having knowledge of your risk is crucial.”
Source: Shahrin Ahmed/X