Andy Minn, Professor at University of Pennsylvania School of Medicine, shared a post on X:
“Summary of our paper on combining JAK inhibitors with anti-PD1 for lung cancer (NSCLC). Part of a bench-to-bedside journey to understand opposing roles of Interferon (IFN) in IO. Wonderful team with John Wherry, Divij Mathew, Caitlin Foley, Melina Marmarelis, Joshua Bauml et al!
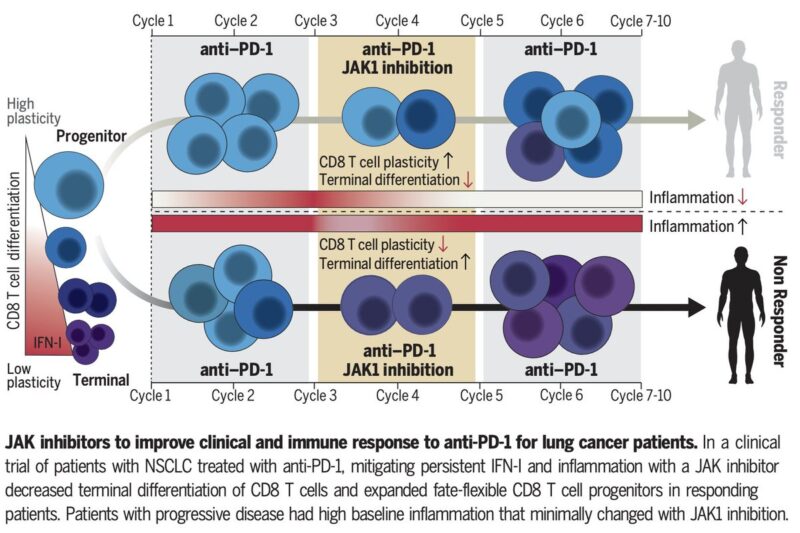
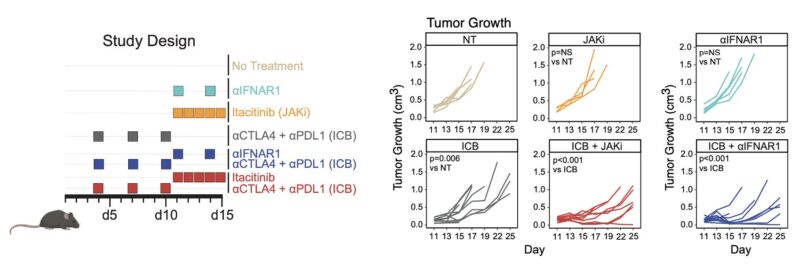
In mice, chronic IFN paradoxically leads to immune checkpoint blockade (ICB) resistance. Blocking IFN in cancer or immune cells improves immune function, promoting CD8 T cells to take on non-exhausted fates. Similarly, a JAK inhibitor (JAKi) prevents chronic IFN and improves ICB.
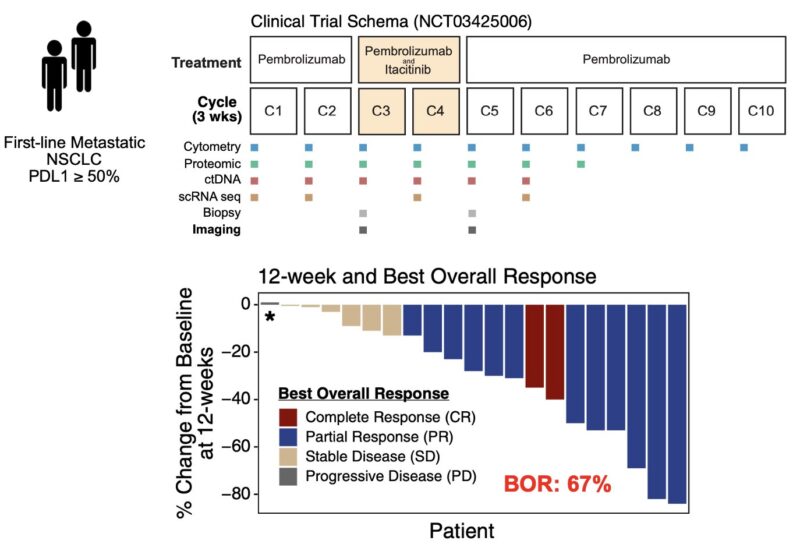
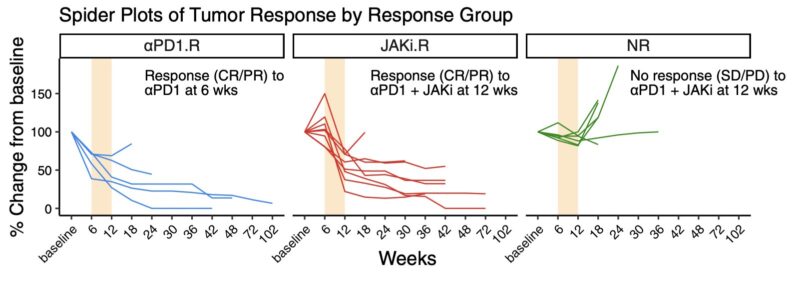
We adapted this JAKi strategy in a phase 2 trial for first-line stage IV NSCLC with PDL1 >= 50%. Patients received anti-PD1 (pembro) for cycles 1-2, then JAKi was added for cy3-4, then back on aPD1 alone. Best overall response rate was 67%, which is high. Durability was notable too.
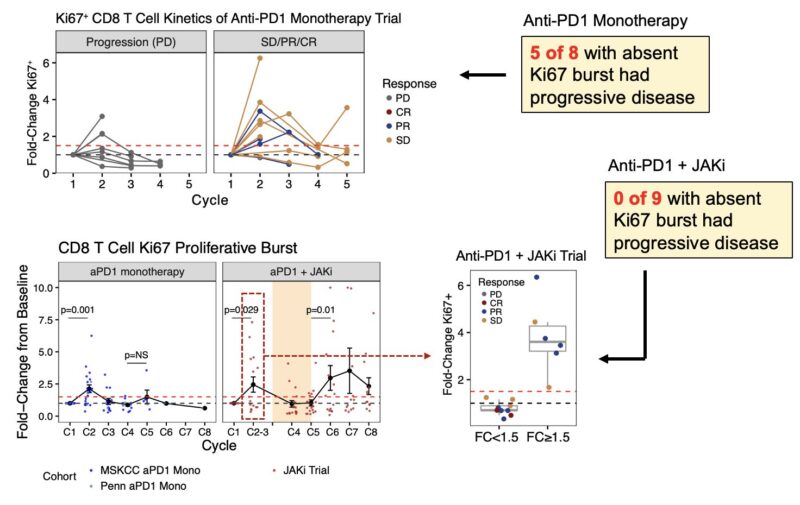
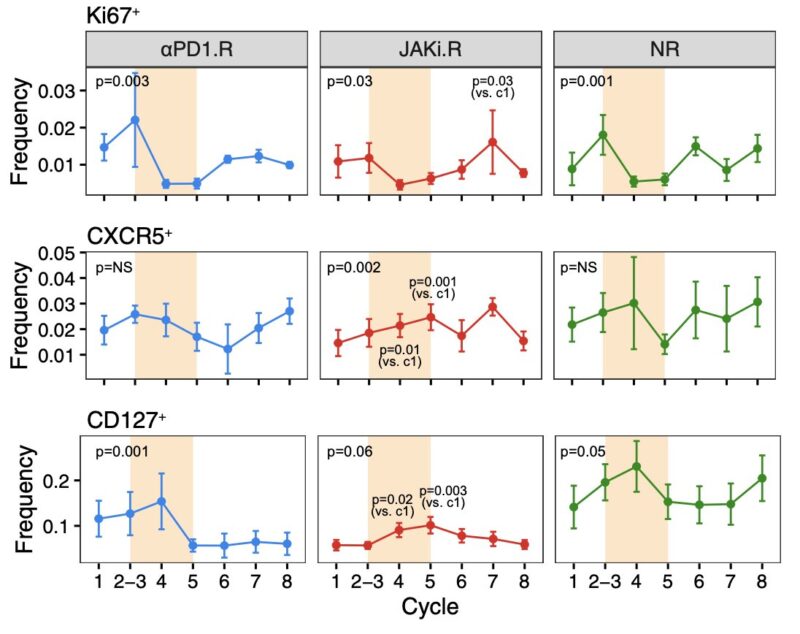
Typically a single CD8 T cell Ki67 proliferation burst occurs shortly after aPD1. Its absence predicts progression, which we confirmed in an aPD1 only cohort. With aPD1+JAKi, patients without this aPD1 proliferation burst still responded and a post-JAKi proliferation burst occurred. What was JAKi doing?
Besides T cell responses, tumor response patterns were insightful too. Some patients responded during cy1-2 of aPD1 before addition of JAKi (aPD1.R), some only after JAKi was added (JAKi.R) during cy3-4 (colored beige in plots), and others failed to respond even after JAKi (NR).
Notably, JAKi.R patients were the ones who, on average, did not have an early CD8 T cell proliferation burst after aPD1. So what did JAKi do to potentially salvage clinical response and immune function? Initial analysis pointed towards CD8 T cells expressing PD1, CD127, and/or CXCR5.
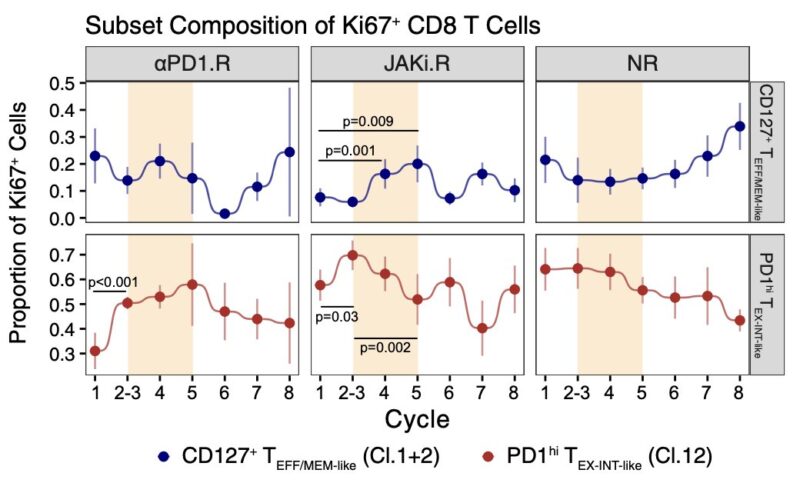
Rather than just proliferation status, we focused on the composition of proliferating CD8 T cells. We found that in JAKi.R patients, addition of JAKi led to a unique compositional change – an increased proportion of CD127 effector/memory T cells and decreased PD1 exhausted cells (Tex).
This improved composition of proliferating CD8 T cells in JAKi.R patients was coupled to an increase in CD8 T cells with CXCR5, a marker for precursor/progenitor cells, suggesting adding JAKi might’ve yielded a more balanced differentiation of CXCR5 precursors into Tex and non-Tex fates.
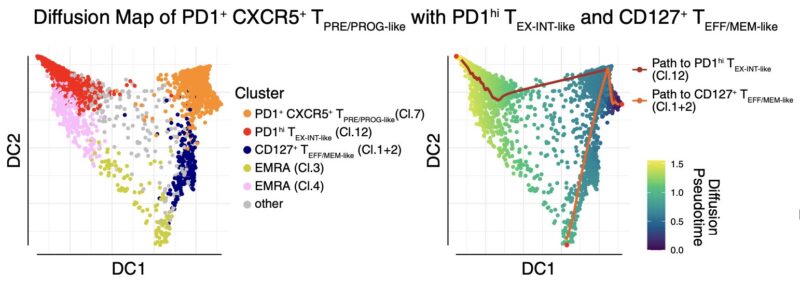
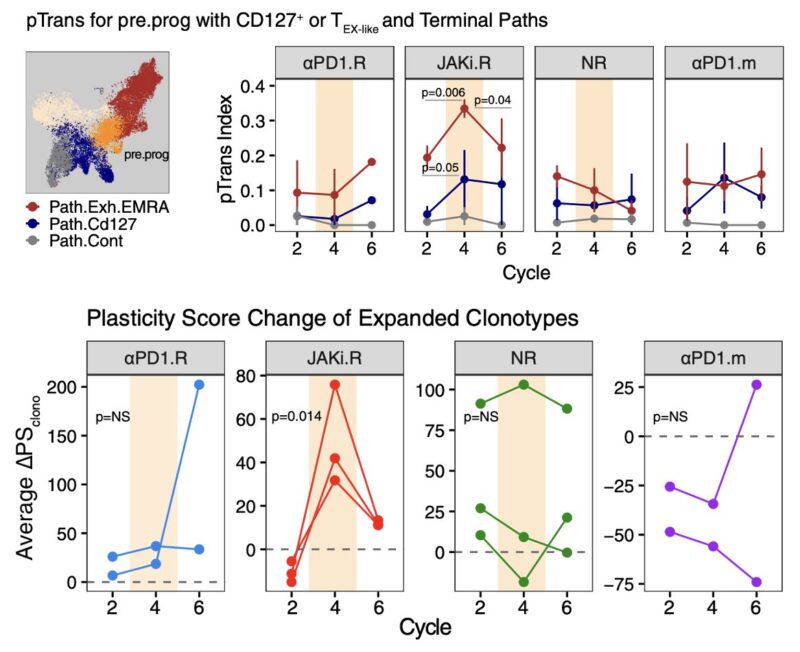
Indeed, CD8 clonotypes enriched in precursor/progenitors showed more differentiation toward Tex and CD127 non-Tex fates during JAKi and specifically in JAKi.R patients. This led to greater CD8 T cell “plasticity” or “fate flexibility”, which might’ve promoted durable response.
Finally, we wondered why NR patients did not benefit from JAKi. These patients had the highest baseline inflammation. Many cytokines including suppressive ones that decreased on JAKi in responders stayed high in NR patients. Thus, NR patients had high baseline inflammation refractory to JAKi.
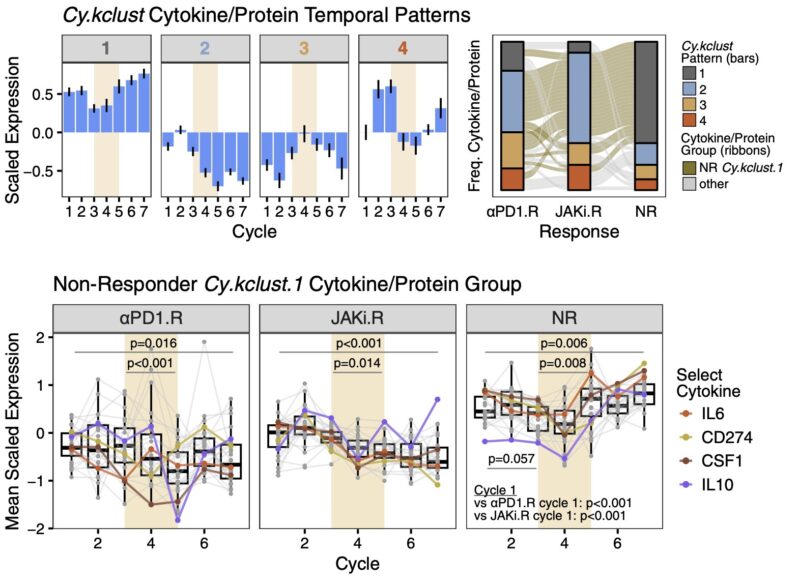
Type I IFN (IFN-I) was among these persistently high and JAKi-refractory cytokine pathways in NR patients. In CD8 T cells, this persistent IFN-I signaling was linked to progressive Tex clonal expansion and therapy failure, consistent with known roles for IFN-I in driving Tex.
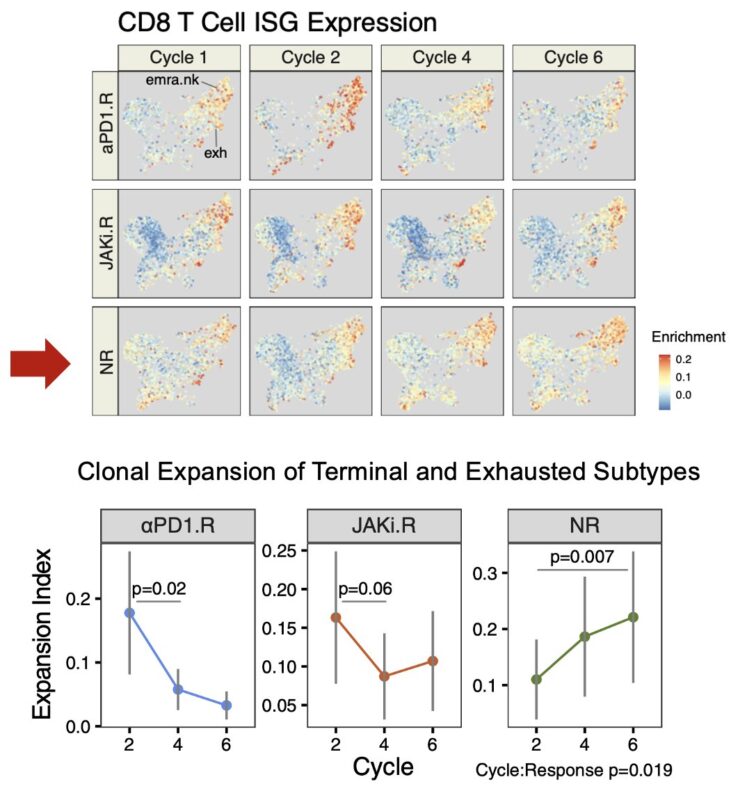
In summary, adding JAKi to aPD1 in NSCLC may help to rebalance CD8 T cell differentiation dynamics by pivoting differentiation away from Tex. This was associated with high response rates. Refractoriness to JAKi was linked to progressive Tex and therapy failure.
Remarkably, the potential benefit of combining JAK inhibitors to anti-PD1 may span different cancer types, clinical settings, and immune cell types. See Teijaro Lab’s paper too! Hope this was helpful!”
Source: Andy Minn/X
