What is follicular lymphoma?
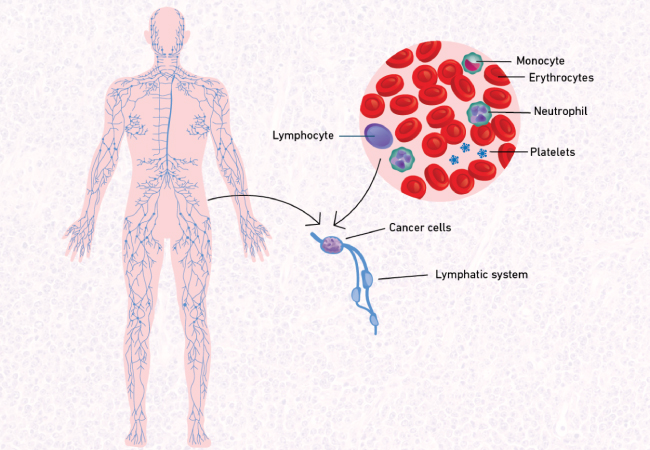
Follicular lymphoma (FL) is a type of blood cancer that originates from B-lymphocytes, a type of white blood cell. It is classified as a non-Hodgkin lymphoma (NHL) and is characterized by the formation of abnormal lymphoid follicles within the lymph nodes.
Source of image lymphomachallenge.ethz.ch
Causes and Risk Factors
Genetic Factors
- Chromosomal Translocations
- Mutations in Specific Genes
Environmental Factors
- Chemical Exposure: Exposure to certain chemicals, such as pesticides, herbicides, and industrial solvents, has been associated with an increased risk of developing FL. However, more research is needed to establish definitive links.
- Radiation Exposure: Individuals exposed to high levels of radiation, either occupational or due to nuclear accidents have an increased risk of developing FL
- Lifestyle Factors: Aspects of a Western lifestyle, including a sedentary lifestyle, obesity, and diets high in meat and milk, have been associated with an increased risk of FL. Conversely, diets rich in fruits, vegetables, polyunsaturated fatty acids, and vitamin D may reduce the risk.
Immunological Factors
- Immune Suppression: Conditions that weaken the immune system, such as HIV infection, congenital immunodeficiencies, or the use of immunosuppressive drugs (e.g., post-organ transplant medications), increase the risk of developing FL.
- Autoimmune Diseases: Autoimmune conditions like rheumatoid arthritis, Sjogren’s syndrome, systemic lupus erythematosus, and celiac disease are associated with a higher risk of FL.
Infections
- Viral Infections: Certain viral infections, including Epstein-Barr virus (EBV), human T-cell lymphotropic virus (HTLV) type I, and human herpesvirus 8 (HHV-8), have been implicated in the development of FL, although these viruses are more commonly associated with other types of lymphomas.
- Bacterial Infections: Infections with certain bacteria, such as Helicobacter pylori, have been linked to an increased risk of NHL, though the evidence for FL specifically is less clear.
Demographic Factors
- Age: The risk of developing follicular lymphoma increases with age, with the median age at diagnosis being 60-65 years.
- Gender: FL is slightly more common in women than in men.
- Ethnicity and Geography: The incidence of follicular lymphoma is higher in Caucasians compared to African Americans and Asians. It is also more common in developed countries like the United States and Western Europe.
Family History
Having a first-degree relative with NHL increases the risk of developing follicular lymphoma, suggesting a potential genetic predisposition.
Other Factors
- Medical History: A history of certain medical conditions, such as heart disease and previous cancer treatments, may be associated with an increased risk of FL.
- Occupational Exposures: Certain occupations, such as spray painters, have been linked to a higher risk of FL due to exposure to potentially harmful chemicals.
In summary, the development of follicular lymphoma is influenced by a combination of genetic, environmental, immunological, and demographic factors. Understanding these risk factors can help identify individuals at higher risk and potentially guide preventive strategies and early interventions.
Symptoms
Common Symptoms
Painless Swelling of Lymph Nodes: The most common symptom is the presence of one or more painless swellings in the lymph nodes, which can occur in the neck, armpit, or groin. These swellings are due to enlarged lymph nodes caused by the accumulation of lymphoma cells.
General Symptoms (B Symptoms)
B Symptoms: These include a group of systemic symptoms that are less common in follicular lymphoma compared to high-grade lymphomas but can still occur:
- Unexplained Weight Loss: Significant weight loss without any obvious reason.
- Fevers: Persistent or intermittent fevers with a temperature above 38ºC.
- Drenching Night Sweats: Severe night sweats that can soak through clothing and bedding.
Other Symptoms
- Fatigue: Overwhelming tiredness that does not improve with rest.
- Frequent Infections: Increased susceptibility to infections or difficulty recovering from infections due to compromised immune function.
- Shortness of Breath: This can occur if the lymphoma affects the chest area or if there is significant anemia.
- Loss of Appetite: Reduced desire to eat, which can contribute to weight loss.
- Generalized Aches and Pains: Unexplained aches and pains throughout the body.
Extranodal Symptoms
Follicular lymphoma can also present outside the lymph nodes, known as extranodal lymphoma, leading to additional symptoms depending on the affected area:
Bone Marrow Involvement: Around half of the patients have lymphoma cells in their bone marrow at diagnosis, which can cause:
- Anemia: Low red blood cell count, leading to tiredness and shortness of breath.
- Thrombocytopenia: Low platelet count, increasing the risk of bruising and bleeding.
- Neutropenia: Low neutrophil count, making the patient more prone to infections.
Emotional and Psychological Impact
Anxiety and Emotional Distress: The chronic nature of the disease and the uncertainty regarding its progression can lead to significant emotional and psychological stress.
In summary, while many people with follicular lymphoma may not exhibit symptoms initially, the disease can present with a range of symptoms that affect both physical and emotional well-being. The most common initial sign is painless swelling of the lymph nodes, but systemic symptoms like weight loss, fever, night sweats, and fatigue can also occur, especially as the disease progresses.
Diagnosis
The diagnosis of follicular lymphoma (FL) involves a combination of clinical evaluation, imaging studies, and laboratory tests. Here is a detailed overview of the diagnostic process based on the provided sources:
Clinical Evaluation
- Physical Examination: The initial step often involves a thorough physical examination to check for swollen lymph nodes, spleen, or liver. The doctor will palpate areas such as the neck, armpits, and groin to detect any enlarged lymph nodes.
Imaging Studies
- CT Scans and PET Scans: Imaging studies like computed tomography (CT) scans and positron emission tomography (PET) scans are used to visualize the extent of the disease. These scans help in staging the lymphoma by showing how far it has spread to lymph nodes or other organs.
- Bone Marrow Biopsy: A bone marrow biopsy may be performed to check if the lymphoma has spread to the bone marrow. This involves taking a sample of bone marrow, usually from the hip bone, to look for lymphoma cells.
Laboratory Tests
Blood Tests: While blood tests cannot diagnose follicular lymphoma, they provide important information about the patient’s overall health and how the disease is affecting the body.
Common blood tests include:
- Complete Blood Count (CBC): Measures the levels of red blood cells, white blood cells, and platelets. Abnormal counts can indicate bone marrow involvement.
- Liver and Kidney Function Tests: Assess how well the liver and kidneys are functioning, which is important for planning treatment.
- Lactate Dehydrogenase (LDH): Elevated levels of LDH can indicate more aggressive disease.
- Beta-2 Microglobulin (B2M): High levels of B2M can suggest a more aggressive form of FL.
Biopsy
- Lymph Node Biopsy: The definitive diagnosis of follicular lymphoma is made through a biopsy of an enlarged lymph node. There are different types of biopsies:
- Excisional Biopsy: Removal of an entire lymph node, which is the preferred method for diagnosing FL as it provides a larger tissue sample for analysis.
- Core Needle Biopsy: Removal of a small cylinder of tissue using a wide needle. This is less invasive but may not always provide enough tissue for a definitive diagnosis.
- Fine Needle Aspiration (FNA): Involves using a thin needle to remove a small sample of cells. This method is generally not recommended for diagnosing FL due to insufficient tissue for analysis.
Histopathological Examination
- Microscopic Examination: A pathologist examines the biopsy sample under a microscope to identify the characteristic features of follicular lymphoma, such as the presence of abnormal B-cells forming follicular patterns.
- Immunohistochemistry: This involves staining the biopsy tissue with antibodies to detect specific proteins that are characteristic of FL.
Genetic and Molecular Tests
- Fluorescence In Situ Hybridization (FISH): This test detects specific genetic abnormalities, such as the t(14;18) translocation, which is common in FL.
- Polymerase Chain Reaction (PCR): Used to detect genetic mutations and translocations at a molecular level, providing additional information about the lymphoma.
Staging
- Staging: After diagnosis, the disease is staged to determine its extent. The Ann Arbor staging system is commonly used, and it ranges from Stage I (localized) to Stage IV (widespread).
In summary, the diagnosis of follicular lymphoma involves a combination of physical examination, imaging studies, blood tests, and most importantly, a biopsy of an affected lymph node. The biopsy sample is then analyzed using various techniques to confirm the presence of follicular lymphoma and to determine its specific characteristics and stage.
Treatment
Watchful Waiting
Active Surveillance: For patients with no or very few symptoms, physicians may recommend a “watch and wait” approach. This involves regular checkups and monitoring through laboratory and imaging tests. Treatment is initiated if symptoms develop or if there are signs of disease progression.
Chemotherapy
Combination Chemotherapy: Common regimens include:
- R-CHOP: Rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone.
- R-CVP: Rituximab, cyclophosphamide, vincristine, and prednisone.
- R-Bendamustine: Rituximab and bendamustine.
- Other Combinations: Chlorambucil with rituximab, and lenalidomide with rituximab (R2).
Immunotherapy
- Monoclonal Antibodies: Rituximab and obinutuzumab are commonly used. These antibodies target the CD20 protein on B-cells, marking them for destruction by the immune system.
- CAR T-Cell Therapy: This involves modifying a patient’s T-cells to better target and destroy cancer cells. Approved CAR T-cell therapies include tisagenlecleucel (Kymriah) and axicabtagene ciloleucel (Yescarta).
- Bi-specific Antibodies: These antibodies bring T-cells and B-cells together to enhance targeting of cancer cells. Examples include mosunetuzumab-axgb (Lunsumio).
Radiation Therapy
- Localized Radiation: Effective for early-stage follicular lymphoma confined to one area. Radiation can provide long-lasting remission in some patients.
Maintenance Therapy
- Rituximab Maintenance: After initial treatment, rituximab can be given every two months for up to two years to prolong remission.
Emerging and Experimental Treatments
- Tazemetostat: An EZH2 inhibitor used for treating follicular lymphoma, often in combination with other drugs to enhance efficacy.
- Lenalidomide: An immune modulator used in combination with rituximab for relapsed or refractory FL.
- Checkpoint Inhibitors: These drugs help the immune system recognize and attack cancer cells, though they are still largely experimental for FL.
Stem Cell Transplantation
- Autologous and Allogeneic Transplants: Used for relapsed or refractory follicular lymphoma, especially in younger patients. This involves high-dose chemotherapy followed by the infusion of healthy stem cells to restore bone marrow function.
Radioimmunotherapy
- Yttrium-90 Ibritumomab Tiuxetan (Zevalin): Combines a radioactive particle with an antibody to target and destroy cancer cells.
In summary, the treatment of follicular lymphoma involves a range of options tailored to the stage of the disease, the presence of symptoms, and the patient’s overall health. The goal is to manage the disease effectively while minimizing side effects and maintaining quality of life.
More information about completed and ongoing clinical trials can be found here clinicaltrials.gov
Prognosis and Survivorship
Follicular lymphoma (FL) is a slow-growing type of non-Hodgkin lymphoma that, while generally considered incurable, has a relatively favorable prognosis. Many patients live for many years, often managing the disease as a chronic condition with periods of remission and relapse. The introduction of treatments like rituximab has significantly improved survival rates, with many patients experiencing long-term remissions. Regular monitoring and personalized treatment plans are essential, and advancements in therapy continue to improve outcomes, offering hope for even better management of the disease in the future.
Watch Juliana’s fight story from Lymphoma Research Foundation
During Treatment
Common side effects include:
During treatment for follicular lymphoma, common side effects can vary depending on the type of therapy used. Here are some of the common side effects associated with different treatments:
Chemotherapy
- Fatigue: Extreme tiredness that does not improve with rest.
- Nausea and Vomiting: Feeling sick and vomiting are common.
- Hair Loss (Alopecia): Temporary loss of hair.
- Infections: Increased risk due to low white blood cell counts.
- Bruising and Bleeding: Due to low platelet counts.
- Mouth Sores: Painful sores in the mouth.
- Constipation or Diarrhea: Changes in bowel habits.
- Loss of Appetite: Reduced desire to eat.
- Peripheral Neuropathy: Nerve damage causing tingling, numbness, and pain in the hands and feet.
Radiation Therapy
- Skin Changes: Redness, blistering, and peeling in the treated area.
- Fatigue: General tiredness.
- Nausea and Diarrhea: Especially if the abdomen is treated.
- Mouth Sores and Trouble Swallowing: If the head and neck are treated.
Immunotherapy (e.g., Rituximab)
- Infusion Reactions: Fever, chills, rash, and shortness of breath during or after infusion.
- Infections: Due to decreased white blood cell counts.
- Fatigue: Common with immunotherapy.
CAR T-Cell Therapy
- Cytokine Release Syndrome (CRS): Fever, chills, fatigue, nausea, and muscle aches due to a massive release of cytokines.
- Neurotoxicity: Headache, confusion, dizziness, and seizures.
- Tumor Lysis Syndrome (TLS): Rapid breakdown of cancer cells causing kidney and heart problems.
General Side Effects
- Fever: Often a sign of infection.
- Weight Changes: Loss or gain of weight.
- Shortness of Breath: Due to low red blood cell counts or lung involvement.
It is important for patients to communicate with their healthcare team about any side effects they experience, as there are often ways to manage and mitigate these effects to improve quality of life during treatment.
After Treatment
Follow-up Care
After completing treatment for follicular lymphoma (FL), follow-up care is crucial to monitor your health, manage any side effects, and check for signs of recurrence. Here are some key aspects of follow-up care based on the provided sources:
- Regular Check-Ups: You will have regular appointments with your healthcare team, which may include your oncologist, cancer nurse, or GP. These check-ups are typically more frequent in the first few years after treatment (every 3-4 months) and may become less frequent over time (every 6-12 months).
- Monitoring for Recurrence: Your doctor will watch for signs of cancer recurrence or a second cancer. This involves physical exams, blood tests, and imaging tests like CT scans or PET scans, depending on your specific situation.
- Managing Side Effects: Follow-up care includes managing long-term and late side effects of treatment, such as fatigue, cardiovascular issues, and secondary cancers. Your healthcare team will help you address these issues and improve your overall quality of life.
- Survivorship Care Plan: You should receive a survivorship care plan, which is a detailed summary of your treatment and follow-up care recommendations. This plan helps guide your ongoing care and ensures that all healthcare providers involved in your care are informed.
- Self-Management and Support: You may have follow-up care over the phone or via telehealth, especially if you live in a rural area. This type of care, known as supported self-management, allows you to be more in control of your health while still having access to your healthcare team for support and advice.
- Emotional and Psychological Support: Follow-up care also addresses emotional and psychological needs. You may be referred to a psychologist or counselor for support with anxiety, depression, or fear of recurrence. Support groups and survivorship resources are also available to help you cope with the emotional aspects of living with and beyond cancer.
- Healthy Living Tips: Your healthcare team will provide advice on maintaining a healthy lifestyle, including diet, exercise, and avoiding risk factors that could affect your health. This can help improve your overall well-being and reduce the risk of recurrence.
In summary, follow-up care after treatment for follicular lymphoma is essential for monitoring your health, managing side effects, and providing emotional and psychological support. Regular check-ups, a detailed survivorship care plan, and access to support services are key components of effective follow-up care.
Resources
- American Cancer Society – Cancer.org
- National Cancer Institute – Cancer.gov
- American Society of Clinical Oncology (ASCO) – Cancer.net
- Լymphoma Research Foundation – lymphoma.org
- Blood Cancer UK – bloodcancer.org
- Follicular lymphoma in the modern era: survival, treatment outcomes, and identification of high-risk subgroups – Blood Cancer Journal
- Follicular Lymphoma Foundation – theflf.org
- Leukemia and Lymphoma Society – lls.org
- Cancer Research Institute – cancerresearch.org
- Follicular lymphoma – treatment and prognostic factors – PubMed
- Oncodaily.com