Lung cancer and immunotherapy
Lung cancer is the leading cause of cancer-related deaths worldwide, with an estimated 1.8 million deaths in 2020 according to the World Health Organization. Immunotherapy is a revolutionary approach that harnesses the body’s immune system to fight cancer cells. In lung cancer, immunotherapy works by enabling the immune system to recognize and attack cancer cells more effectively, helping to control the growth and spread of the disease.
Lung cancer immunotherapy involves using drugs that target specific proteins on immune cells or cancer cells, unleashing the immune system’s ability to detect and destroy cancer cells. This approach has shown promising results in both non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC), offering new hope for patients.
The symptoms of lung cancer are presented in this video produced by Cancer Research UK.
Types of immunotherapy for lung cancer
There are several types of immunotherapy used to treat lung cancer, some of which are approved and available for use, while others are still being trialled.
- Immune checkpoint inhibitors: These drugs target specific proteins on immune cells or cancer cells known as “checkpoints” or brakes, preventing the immune system from mounting an effective anti-tumor response. By blocking these checkpoint proteins, the drugs release the brakes and allow the immune system’s T cells to recognize and attack the cancer cells more efficiently. The most commonly targeted checkpoint proteins are PD-1 (programmed cell death protein 1) on T cells and PD-L1 (programmed death ligand 1) on cancer cells. Checkpoint inhibitors work by disrupting the interaction between PD-1 and PD-L1, reactivating the T cells and enabling them to target and kill the cancer cells. Examples include pembrolizumab, nivolumab, atezolizumab, and durvalumab.
- Cancer vaccines: These are designed to stimulate the immune system to recognize and attack specific cancer cells by introducing tumor-associated antigens or proteins. The vaccines aim to prime the immune system to recognize these antigens as foreign and mount an immune response against the cancer cells expressing them. Different types of cancer vaccines are being explored, including peptide vaccines, dendritic cell vaccines, and viral vector vaccines. Examples include tecemotide and GVAX which are being tested in clinical trials with various success rates.
- Adoptive cell transfer: This approach involves removing immune cells (such as T cells) from the patient, modifying them in the laboratory to enhance their ability to recognize and attack cancer cells, and reintroducing them back into the patient’s body. The modified T cells are often engineered to express specific receptors (e.g., chimeric antigen receptors or CARs) that target tumor-associated antigens. CAR-T cell therapy against lung cancer is still in clinical trials.
More information about completed and ongoing clinical trials for lung cancer can be found here – clinicaltrials.gov
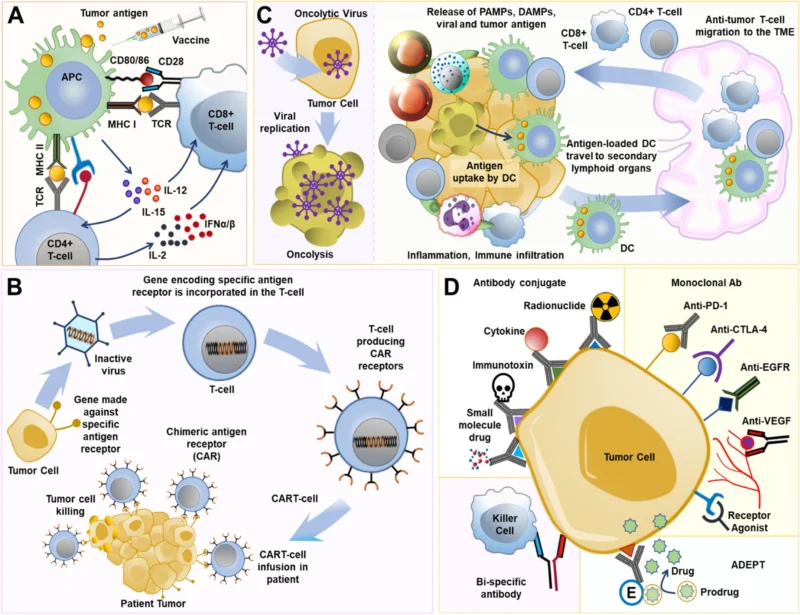
Different aspects of lung cancer immunotherapy: A: Using a tumor-specific vaccine to fight cancer. B: Collecting T cells from either the donor or the patient, genetically modifying them to introduce Chimeric Antigen Receptor (CAR) receptors, and then mass-producing these cells in the lab. Once infused back into the patient, these CAR T-cells target and attack the tumor. C: Employing oncolytic viruses to induce the destruction of cancer cells. D: Utilizing monoclonal antibodies (mAbs) to target specific sections of cancer cells, potentially offering an effective treatment for lung cancer. Image source: Lahiri et al.
Drugs approved for lung cancer immunotherapy
Several immunotherapy drugs have been approved by the U.S. Food and Drug Administration (FDA) for the treatment of lung cancer.
- Immunotherapy for NSCLC:
-
- Pembrolizumab (Keytruda): A PD-1 immune checkpoint inhibitor approved in 2015 for first-line treatment of metastatic NSCLC with high PD-L1 expression, and as a second-line treatment for advanced NSCLC after chemotherapy.
- Nivolumab (Opdivo): A PD-1 immune checkpoint inhibitor approved in 2015 for second-line treatment of advanced NSCLC after chemotherapy, and in combination with ipilimumab (Yervoy) for first-line treatment of metastatic NSCLC.
- Atezolizumab (Tecentriq): A PD-L1 immune checkpoint inhibitor approved in 2016 for first-line treatment of metastatic NSCLC with high PD-L1 expression
- Durvalumab (Imfinzi): A PD-L1 immune checkpoint inhibitor approved in 2018 for unresectable stage III NSCLC after chemoradiation therapy.
- Ipilimumab (Yervoy): A CTLA-4 immune checkpoint inhibitor approved in 2018 in combination with nivolumab for first-line treatment of metastatic NSCLC.
- Immunotherapy for SCLC:
-
- Nivolumab (Opdivo): Approved in 2018 in combination with chemotherapy for the treatment of advanced SCLC.
- Atezolizumab (Tecentriq): Approved in 2019 in combination with chemotherapy for the treatment of advanced SCLC.
These immune checkpoint inhibitors work by disrupting the PD-1/PD-L1 and CTLA-4 pathways that cancer cells use to evade the body’s immune system. By blocking these proteins, the drugs allow the T cells to recognize and kill the cancer cells more effectively, leading to improved survival outcomes in many patients.
This short video provides insight into a study revealing that neoadjuvant Durvalumab alongside chemotherapy in resectable NSCLC patients resulted in improved outcomes and safety compared to chemotherapy alone. Video source: NEJM.org
Immunotherapy side effects
Immunotherapy works by stimulating the body’s immune system to recognize and attack cancer cells more effectively. However, this heightened immune response can also lead to adverse effects, as the activated immune cells may inadvertently target healthy tissues and organs. The side effects of immunotherapy can vary in severity and can affect different parts of the body.
Some common side effects of immunotherapy drugs include fatigue, nausea, itching, skin rash, and more. These side effects are generally less toxic than traditional chemotherapy. However, because immunotherapy drugs work by stimulating the immune system, it is possible to develop serious immune-related adverse events (irAEs) from an over-stimulated immune system, which can affect how various organs function. These irAEs can affect various organs and systems in the body, and their severity can range from mild to life-threatening.
Some examples of immune-related adverse events and their associated symptoms include:
- Pulmonary (lung) toxicity: Pneumonitis (inflammation of the lungs), shortness of breath, cough, chest pain
- Gastrointestinal toxicity: Colitis (inflammation of the colon), diarrhea, abdominal pain, nausea, vomiting
- Hepatic (liver) toxicity: Hepatitis (liver inflammation), elevated liver enzymes, jaundice
- Endocrine toxicity: Thyroiditis (thyroid gland inflammation), hypophysitis (pituitary gland inflammation), adrenal insufficiency, diabetes
- Dermatologic (skin) toxicity: Severe rash, pruritus (itching), vitiligo (patchy loss of skin pigmentation)
- Musculoskeletal toxicity: Arthralgia (joint pain), myalgia (muscle pain), polymyalgia rheumatica
- Neurological toxicity: Headache, dizziness, confusion, peripheral neuropathy
- Renal (kidney) toxicity: Nephritis (kidney inflammation), increased creatinine levels
- Cardiovascular toxicity: Myocarditis (inflammation of the heart muscle), pericarditis (inflammation of the sac surrounding the heart)
The prevalence of these side effects can vary and depend on the specific immunotherapy drug used.
Early recognition and prompt management of adverse events are crucial to prevent potentially life-threatening complications. This may include withholding or discontinuing immunotherapy, administering corticosteroids or other immunosuppressive agents, and providing supportive care as needed.
Life expectancy after immunotherapy
The life expectancy after immunotherapy for lung cancer can vary depending on several factors, including the stage of the cancer, the type of immunotherapy used, and the individual patient’s response to treatment. However, several studies have shown promising results in terms of improved survival rates. Below are some up-to-date data about this.
Non-small cell lung cancer:
- In the KEYNOTE-024 trial, patients with advanced NSCLC who received pembrolizumab (an anti-PD-1 immunotherapy) had increased overall survival compared to those who received chemotherapy alone.
- The CheckMate-017 and CheckMate-057 trials evaluated nivolumab (another anti-PD-1 immunotherapy) in advanced NSCLC. The overall survival was higher compared to docetaxel chemotherapy.
Small cell lung cancer:
- In the CASPIAN trial, patients with extensive-stage SCLC who received durvalumab (an anti-PD-L1 immunotherapy) in combination with chemotherapy showed overall improved survival compared to those who received chemotherapy alone.
- The IMpower133 trial evaluated atezolizumab (anti-PD-L1 immunotherapy) in combination with chemotherapy for extensive-stage SCLC. This regimen also showed improved survival compared to chemotherapy alone.
More information about completed and ongoing clinical trials for lung cancer can be found here clinicaltrials.gov
It’s important to note that these are median survival times, and individual patient outcomes can vary significantly based on factors such as the stage of the disease, the specific immunotherapy regimen used, and the patient’s overall health status.
While these data demonstrate a significant improvement in life expectancy with immunotherapy, ongoing research and clinical trials are continuously exploring ways to further enhance the efficacy of these treatments and improve long-term survival outcomes for lung cancer patients.
FAQs
Who qualifies for immunotherapy?
Immunotherapy is typically recommended for patients with advanced or metastatic lung cancer, particularly NSCLC. Patients with certain biomarkers, such as high levels of PD-L1 expression, may be more likely to respond to immunotherapy. However, eligibility criteria can vary depending on the specific immunotherapy drug and the patient’s overall health condition.
What is the success rate of immunotherapy for lung cancer?
The success rate of immunotherapy for lung cancer can vary depending on the type of immunotherapy used, the stage of the cancer, and individual patient factors.
How long does immunotherapy work for lung cancer?
The duration of immunotherapy’s effectiveness can vary significantly among patients. Some patients may experience long-term remission, while others may experience disease progression after an initial response. Factors such as the type of immunotherapy, the stage of the cancer, and the patient’s overall health can influence the duration of response. Ongoing monitoring and follow-up are essential to determine the appropriate course of treatment.
Sources
- Lung cancer immunotherapy: progress, pitfalls, and promises – Molecular Cancer
- Perioperative Pembrolizumab for Early-Stage non-small cell lung cancer- NEJM
- Immunotherapy in NSCLC: Past, present, and future directions – Frontiers in Oncology
- Lung Cancer Immunotherapy – American Lung Association
- Immunotherapy and its side effects – Cancer Research UK
- Duration of Immunotherapy in Non-Small Cell Lung Cancer Survivors: A Lifelong Commitment? – Cancers
- Nivolumab versus Docetaxel in Advanced Nonsquamous non-small cell lung cancer – NEJM
- Lung Cancer Immunotherapy: Beyond Common Immune Checkpoints Inhibitors – Cancers
- Immunotherapy in lung cancer – Translational Lung Cancer Research
- Current state of immunotherapy for non-small cell lung cancer – Translational Lung Cancer Research
- Lung cancer immunotherapy – Clinicaltrials.gov