Through the lens of Stephanie Gayhart – an Oral Squamous Cell Carcinoma Survivor
Stephanie Gayhart, a nurse leader and survivorship expert, shared about her battle with Oral Squamous Cell Carcinoma on her LinkedIn. Her journey through cancer inspired many and prompted us at OncoDaily to join in spreading awareness about this disease.
As we observe Head and Neck Cancer Awareness Month, we aim to share Stephanie’s story and educate our readers about this often misunderstood illness.
Join us as we delve into her experiences and strive to understand and support for those affected by cancer:
Viewer discretion is advised. This content may contain sensitive media.
Day 1 of Head and Neck Cancer Awareness Month
The Stef in the photo here had stage 3 oral tongue cancer, HPV negative, no known risk factors.
The Stef in this photo was a seasoned critical care nurse and had no idea someone her age and health status could have a rapidly growing tumor show up on her tongue.
The Stef in this photo had been told by multiple providers that the tumor couldn’t be cancer because she was too young at 37 years old.
She would soon find out she was not alone…

Photo taken from Stephanie Gayhart/LinkedIn
Day 2 of Head & Neck Cancer Awareness month and Adolescent & Young Adult (AYA) Cancer Awareness week
At 37 years old I was diagnosed with squamous cell carcinoma of the oral tongue. I had to figure out how to tell my then 6-year-old son that his mom may never talk again, would have to spend extra time at his daddy’s house, and that I was going to come home after surgery looking much different. Almost every day in the 20 days between diagnosis and surgery, we read a story called “Cancer Hates Kisses” by Jessica Reid Sliwerski.
I broke out of the hospital a week after my surgery, on his first day of First Grade. He was terrified to be near me. My face was swollen, I had bandages everywhere, and a tube coming out of my nose. I sounded really weird when I tried to talk and had to hold my hand over the hole in my neck to speak. Knowing he liked monsters, I told him I was like the one from Frankenstein now because the doctors had taken parts of my body and moved them around to create a new me. He thought that was cool. I also told him the doctors thought all of the cancer was gone so his kisses had helped get rid of it!
Cancer sucks at any age, but trying to be a single mom to a young child while going through it was just a special kind of hell. Everything I experienced is why I advocate for AYA cancer awareness and cancer research and survivorship. I’ve lived it, I’ve healed myself so much (which is a never-ending work in progress), and now I am dedicating the rest of my life making sure others have an empathetic listener, a partner in survivorship, and know they’re not alone.
I was disheartened last week to hear a prominent figure in epidemiology and cancer state that the reason they don’t advocate to reduce screening ages or consider cancer diagnoses in younger people is because the incidence is so low and “1 out of 250 of my patients would actually have cancer, the rest just wanted some emotional support for something.” While I agree that we can’t go scanning every single person who walks through the door with a vague complaint of pain, there is NO REASON why people like me with visible, symptomatic, rapidly growing tumors should be ignored over and over again until the cancer has spread.
So now, I guess I’ll just have to be louder.

Photo taken from Stephanie Gayhart/LinkedIn
Day 3 of Head & Neck Cancer Awareness Month and AYA Cancer Awareness Week
This photo is my tumor after biopsy (the black mark is from silver nitrate). It went from being just a slightly sore lump under my chin to noticing a lump on my tongue to extreme mouth, neck, and ear pain in just a few weeks. By surgery, 3 weeks after biopsy, it had metastasized to an ipsilateral lymph node in my neck.
Oral Squamous Cell Carcinoma is known for rapid growth and metastasis and early identification is therefore key to overall mortality and morbidity.
Despite going to multiple providers with a very visible and palpable mass, increasing pain, and difficulty with eating and speaking, it took me over a month to get a CT scan and finally see a specialist who would biopsy it.
I realize not everything is worse case scenario, and in fact a young, healthy, female is highly unlikely to show up with a disease like tongue cancer. However, is the cost savings of continually denying one CT scan or one biopsy really worth the long-term costs associated with life-altering surgery and radiation treatments?

Photo taken from Stephanie Gayhart/LinkedIn
Day 4 of Head & Neck Cancer Awareness Month and AYA Cancer Awareness Week
I’ve learned two big lessons since my diagnosis:
1. The only thing I can control, with LOTS of practice, is how I respond to things
2. Duality — I can be terrified and grateful, sad and hopeful, etc.
The first photo here was taken maybe an hour before my hemiglossectomy & neck dissection. The second photo is the next day, after being under anesthesia for roughly 24 hours and finally in my room — trying to smile. I don’t want to sugarcoat my experience; I was absolutely terrified and in a ton of pain in both photos.
When I was diagnosed, I thought a lot about my death — not in a morbid way, but in deciding how I wanted to be remembered. My legacy. I realized very quickly there were two options: people remember me as “poor Stef, she was so miserable at the end” OR “Wow, she really was so bright and hopeful even when she was dying.” I sure as hell didn’t want anyone to ever utter the words “Poor Stef” so I opted for the second. I also realized I didn’t have to die to begin leaving a legacy of hope, love, and kindness. I didn’t have to minimize the fact that this was an absolutely horrific experience AND one that spurred tremendous personal growth and self-love. Cancer wasn’t a gift, but my growth in spite of it was.

Photo taken from Stephanie Gayhart/LinkedIn
Day 5 of Head & Neck Cancer Awareness Month and AYA Cancer Awareness Week
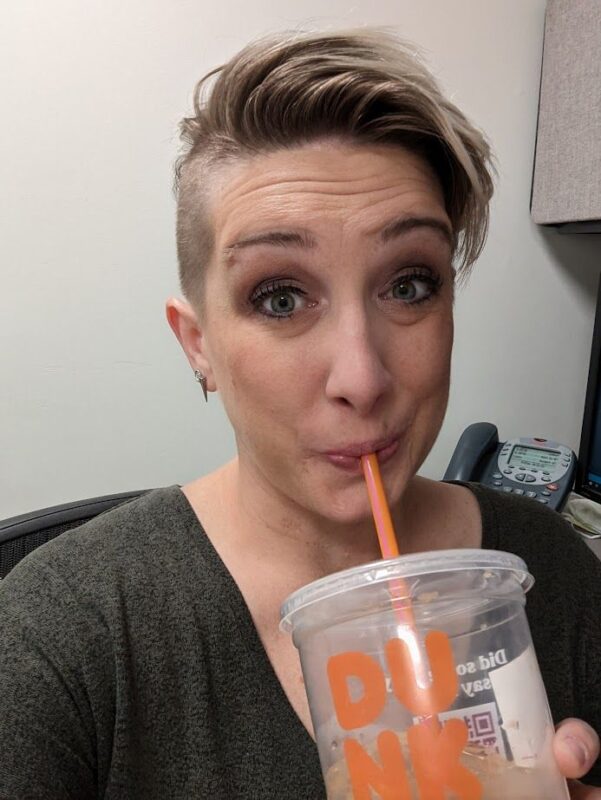
Four days after I left the hospital, 11 days post-op, I begged my partner at the time to take me to the mall. I wanted to have any stimulation I could that wasn’t related to feeding tubes and dressing changes and planning for my second surgery and radiation. I couldn’t use a straw yet but I was happy to take a few bites of a smoothie with a spoon.
It felt SO GOOD to do something “normal”. To not think about cancer for just a little while. I specifically wore my head & neck cancer shirt to try to “explain” without needing to actually say a word because I knew people would wonder. . .and honestly, I wanted them to know. I wanted the whole world to know young people get head & neck cancer!! See. . . we aren’t dramatic, we aren’t faking it, we aren’t overreacting!!
So often, AYAs are dismissed and their tumors continue to grow and spread. For people with aggressive cancers like oral squamous cell carcinoma, this can be deadly at worst, and severely debilitating at best. And for ALL young adults, this dismissal leads to a decrease in trust in the healthcare system and less likelihood of getting concerns addressed in the future.
Is that really the message we want to send?

Photo taken from Stephanie Gayhart/LinkedIn
Day 6 of Head & Neck Cancer Awareness Month and AYA Cancer Awareness Week
According to the NIH SEER database, between 2000-2020 the incidence of tongue cancer has risen in the US AYA population (age 15-39) with an APC of 1.1% for males and 1.3% for females. If we go back to 1975 — the APC is 1.3% for males and 1.9% for females.
Additionally, the 5-year relative survival rate (data calculated between 2013-2019) in the same age group drops drastically from 88.7% in those diagnosed in the early, localized stage of disease to 56.8% in those diagnosed with regional metastasis. Roughly 50% of AYAs tongue cancers are diagnosed in an early stage.
I know we make up a very small amount (<0.1%) of the total US population, but we matter. We are some of your future decision makers, creators, healers, and gamechangers.
How do we prove our lives are worth saving? How do we prove our quality of life is important? How do we calculate the invisible — the human potential lost?
Day 8 of Head & Neck Cancer Awareness Month
My second surgery was short and not at all sweet, but at least I got to go home afterward (and my cat was a great guardian, as seen in the photo).
Have you ever been nasally intubated while awake? 0/10 do not recommend. Because my tongue flap was still healing and my tracheostomy stoma had fully healed by this point, that was our only option. They gave me a lovely cocktail and I remember being very woozy, but also sitting up and screaming as the tube went in and the residents and nurses holding me down telling me “its almost in, we’re almost there.”
Fast forward a few months. My good friend was in the local critical care unit (where I worked), on a ventilator. I went into the room and he needed to be suctioned in-line at one point. I stayed, and started to get tunnel vision and very dizzy. I ran out to sit down at a desk and immediately started sobbing. I had NO IDEA I would react that way to suctioning, but it made sense. Aside from the nasal intubation “fun”, when I was in the hospital after my first surgery my tracheostomy had plugged and necessitated a rapid response and a bedside full trach tube change the next day.
Did you know many cancer survivors suffer from post-traumatic stress (PTS) that may or may not lead to PTSD? Prevalence of actual PTSD is estimated between 3-4% in early-staged, newly diagnosed patients up to 35% in patients who have finished treatment. PTS, which can be more easily treated, is prevalent in anywhere from 20-80% of patients depending on stage at diagnosis.
These are things I don’t talk about often, because I don’t like to focus on the negative, but they had a massive impact on me psychologically, and it needs to be discussed. I am fortunate that I have experienced a lot of post-traumatic growth, but there are so many others who deal in silence with PTS and potentially PTSD that deserve better care.
I’ve said it before and I’ll continue saying it: cancer survivorship isn’t just about the absence or stabilization of disease.

Photo taken from Stephanie Gayhart/LinkedIn
Day 9 of Head & Neck Cancer Awareness Month
I had gotten into the habit of doing Color Runs with my friends a few years before my diagnosis, and was very bummed that the 2019 Baltimore run was going to occur between my surgeries and start of radiation. I asked my surgeons if I could participate anyway, and they said as long as I didn’t overexert myself (lets be honest, I never actually “run”), it was a go!
We named the team “Sun’s Out, Tongues Out” and had a blast. I had finally started to be able to eat real food very slowly, and I felt good. Tired, obviously, but the time with my friends and being out around joyful people made me forget for a little while what I was up against.
I’m a firm believer that positive psychology (NOT toxic positivity) and a great support system have played a massive role in how well I’ve healed. I was fortunate that I had the support system already in place, but the positive outlook took A LOT of work. And not just on my part, but also the people around me. It required a balance between the opposite ends of seeing everything as horrible because we didn’t want to be vulnerable to joy, and seeing everything through rose-colored glasses because we wanted to hide from what we needed to face.
The real healing power, for anyone, comes when we can recognize that this one thing that feels all-encompassing sucks, but it’s really only one part of a vast, ever-changing life we’re living.
That isn’t toxic positivity, that’s the tragic beauty of human life.

Photo taken from Stephanie Gayhart/LinkedIn
Day 10 of Head & Neck Cancer Awareness Month
What you don’t see in the photo: I cried on the way to the party because I was hungry, tired, and in so much pain I could barely drink water. The treatment effects were beginning to accumulate and I was miserable.
People with cancer (and sick people in general) don’t always look or act a certain way, and we have NO IDEA what’s going on under someone else’s mask.

Day 12 of Head & Neck Cancer Awareness Month
Radiation to any part of the body is brutal. It causes long-term effects we aren’t even aware of yet (another reason we should have more AYAs involved in longitudinal studies) and well, the short-term effects speak for themselves.
I enhanced this photo to really show the areas that were targeted and make the photo correspond more accurately to how it felt. By this point, I was taking Oxycodone around the clock along with ibuprofen, plus wearing a Fentanyl patch. The burn on my neck/face was mild compared to inside my mouth. My native tongue was smooth and covered in ulcers. I literally begged for a PEG tube. I would have let them put it in at the office, sitting in the chair at that point. I lost 20 lbs in 6 weeks. I was refused the feeding tube.
For the final weeks of my treatments I wanted to give up. Do you have any idea how hard it is to force yourself to endure a treatment that you know is going to make you feel so much worse?
Toward the end of treatment and then for a week or two after, I needed IV fluids often because my blood pressure stayed stubbornly low. Getting a new IV every few days when I was that dehydrated was an adventure in itself. And, despite my best efforts (including medical friends “borrowing” IV equipment and fluids and administering them at my house on weekends), I finally wound up in the ED with acute liver injury r/t starvation. Because radiation effects are cumulative, and it keeps working for weeks after the final treatment, the side effects also keep getting worse before they level off and begin to subside.
Cancer treatments aren’t only toxic to the part of the body they’re targeting. Supportive, holistic care is VITAL to keeping patients alive and well.

Day 15 of Head & Neck Cancer Awareness Month
November 19th, 2019 I had my final radiation treatment. My mom, my best friend, and my boyfriend at the time came with me to celebrate and document the moment. I thought I’d be happier — I was relieved, don’t get me wrong! But suddenly I had no plan on what to do next. Where do I go from here? I still had frequent check-ins with my radiation oncology team and surgeon (who I still see yearly), but suddenly I felt very alone and unsure of my next steps. And I felt guilty for not feeling joyous! I think both myself and my friends/family/colleagues expected me to still be me, to go through a few weeks of healing and be right back to normal, but I also think part of me also knew that wasn’t going to happen and I had no idea how to face that.
Here’s the thing — when you have a disease like cancer where everything happens rapidly from the time of diagnosis through treatment, you don’t have any time to respond appropriately. You just go along with it and your only goal is to stay alive as long as possible (especially if you have a young kid at home). Then it all stops abruptly if you’re lucky enough to make it to the end of acute treatment, but your mind is still back in the room where you had your diagnosis. It takes time for the person inside to grasp everything they’ve been through, process it, reconcile with it, accept the new version, and move forward on a new path.
This is why I focus so much of my advocacy on survivorship; no one should go through the transition from acute treatment to the next phase, whatever that may be, and feel completely lost and alone. We MUST do a better job catching our survivors in this critical time period and giving them a safe space to land and figure everything out.

Photo taken from Stephanie Gayhart/LinkedIn
Day 17 of Head & Neck Cancer Awareness Month
Every single person in this photo from April 2022 is a tongue cancer survivor, specifically OSCC.
Almost every single person in this phone was diagnosed before the age of 40.
Some of us were diagnosed early, most late stage. Some have had recurrences. All of us know others who have passed away from the same disease. None of us had known risk factors.
My story is far from unique. I wish it wasn’t. Through the internet I’ve met hundreds of other head & neck cancer survivors, hundreds of other AYA survivors, and gotten many random messages asking for support during treatment and afterward. So have all of the people in this photo.
The emotional labor is high, but we respond out of love, because we were once there. But it begs the question: why do people have to reach out to strangers on the internet to feel supported?
Barbara Fountain recognized this and started Young Tongues — a global peer-to-peer support group and now recognized charity in the UK. She and I were diagnosed within the same year, on different continents, and found one another on Instagram. We both had a bunch of connections to other young tongue cancer survivors around the world, and lo, the group was born. Barbara has worked tirelessly to drive this mission and I’m so proud of call her my friend.
Cancer care goes so far beyond cancer centers. Survivorship, from diagnosis forward, takes place at home, at work, in the middle of the night when you can’t sleep worried about an upcoming scan, when you’re worried about how to talk to your kids about your diagnosis, when you don’t know how to navigate the side effects you’re having or just need someone in your corner who gets it and will support you no matter what.
I’m not sure if the healthcare systems will ever get survivorship right, but I have all the faith in the world in groups like this where survivors take the reigns and say “this isn’t working, its time to change the narrative.”

Day 18 of Head & Neck Cancer Awareness Month
I want to focus the rest of the month on side effects and long-term survivorship issues because these are the things that will continue to effect not only survivors, but the healthcare system as a whole. When we disregard the long-term effects of disease treatment, we create a bigger disease burden. I’m not sure why this is such a difficult concept for many, but it seems quite obvious to me. Anyway, I digress. . .
First up: one of the most annoying long-term physical side effects I deal with is dry mouth.
Fun fact: you have different types of saliva! Your parotid glands produce the thin, slippery saliva that’s sort of always there and helps clean your mouth. After radiation through those glands, they don’t function quite as well.
Your other salivary glands produce the thicker saliva used to break down food in the mouth. I had one of those removed during surgery (submental). Saliva helps give food its taste. Try eating with a really dry mouth sometime and you’ll feel that its painful and doesn’t taste as good. Also, trying to swallow without any moisture is an adventure I don’t recommend trying.
I used to love spicy food, now black pepper can be too spicy.
Too much salt or acid knocks out the other taste receptors sometimes for a day or more. I’ve had moments where I couldn’t taste sweet at all.
Speaking of sweet, fruit no longer tastes sweet to me. Actual fruit has become the LaCroix of fruit, if that. I REALLY miss fruit.
On the flip side, I cannot tolerate sugary drinks anymore; soda is disgusting and leaves a weird film in my mouth and makes it feel gritty. Carbonated drinks help me swallow better, so I now drink unsweetened flavored seltzer. Or coffee. Coffee has never failed me THANK GOD.
I try to be mindful every time I leave the house to bring water with me. Dry mouth can also make it almost impossible to talk, so if I’m doing any speaking I have to have water so I can enunciate coherently. I also carry “mouth lube” (my term for saliva substitutes) and mints (which can help increase saliva production, but burn like hell).
Remember how I said the thin saliva cleans your mouth? Thanks to the decrease of that saliva, I’m also at high risk for dental cavities. I am now almost religious about brushing my teeth and still get them.
This is just a tiny snapshot of ONE of the permanent side effects from head & neck cancer treatment that I deal with daily, and I kept it fairly light. Keep that in mind as we go through the rest of the month and think about the survivors you know. I guarantee they are fighting similar silent battles.
Day 20 of Head & Neck Cancer Awareness Month
Lymphedema.
I had no idea head & neck lymphedema was a thing until I had cancer. Roughly 6-12 months after finishing radiation treatment, I started to notice a different feeling on the left side of my face. I also noticed more swelling around the incision in my neck and a tightness.
I am fortunate to live in an area where ReVital Cancer Rehabilitation has an OT specializing in this type of lymphedema and was able to try out and teach me lots of techniques like manual lymphatic drainage, K-taping, garments, and getting a pump from Tactile Medical. (Special shout out to the best PT I know, Heather Roseman, PT, DPT, CDNT for the referral to ReVital and for always treating the WHOLE patient).
Fun fact: head & neck lymphedema usually shows up on the inside first — manifesting as difficulty swallowing or feeling like something is in your throat, difficulty breathing, pain, heaviness, & tightness — without visible changes on the outside.
Lymphedema can be incredibly detrimental to quality of life AND functioning, so its very important to discover and treat early before it gets out of hand. Aside from the obvious physical effects, it can cause psychosocial distress from physical appearance changes, difficulty swallowing (making eating in public more difficult), and distressing flashbacks to feelings we had during diagnosis and treatment.
Unfortunately, head & neck lymphedema garments are incredibly uncomfortable for me (I hate anything around my neck now, including shirts) so I never wore mine. I try to keep up with manual drainage when I wash and moisturize my face and I use my machine when I feel the lymphedema flaring — but not as often as I should. As for the K-tape . . .
I don’t want to walk around town looking like the latest victim of Freddy Kruger so I haven’t done more with that. I do love this Flexitouch machine, though. It doubles as a 32-minute relaxation session because I’m forced to be immobile and just let it do its thing. The trick is getting myself to sit still for 32 minutes (or even the shorter session which I think is about 16 minutes).
I’m not sure if there’s a verified scientific reason for it or not, but my lymphedema seems to flare when we have big storm fronts moving through the area. I’d love to see more research on this very debilitating side effect in all forms, not just head & neck, to find ways to manage and potentially cure it.

Day 23 of Head & Neck Cancer Awareness Month
Today I want to address the very large elephant in the room that people somehow continuously ignore: Sex.
*gasp* *clutches pearls* (here’s where you can stop reading if you want to pretend no one has sex or that heterosexual missionary cis-male to cis-female sex is the only sex people have and its only for procreation.)
Sexual health is an incredibly important part of human lives, and not just for procreation. Sexual health relates to intimacy, relationships, pleasure, self-esteem, etc. It is part of holistic health, and it involves our whole body, mind, and spirit; its not relegated only to the sexual organs. Collectively, we have SO MUCH shame around this topic that its rarely brought up and when it is, providers tend to shy away from talking about it.
I was smack in the middle of truly finally exploring my sexuality (and gender) when I was diagnosed with cancer. I was depressed about losing my tongue and what that meant for intimacy and sex with my current partner.
I was also very worried that the exploration of my sexuality would come to a screeching halt after surgery and radiation, but it felt like that wasn’t important in the face of potentially dying or not being able to eat — so I never brought it up. Interesting how we dismiss our own quality of life concerns sometimes, especially when there’s shame attached.
Since completing treatment, I’ve met many other survivors who have similar tales of concerns related to intimacy and sex. I recently had a young woman reach out to me on social media to discuss things like kissing after tongue cancer and how she could remain intimate with her partner.
She confessed she came from a background where these sorts of things weren’t discussed, but she wanted answers and support, and I gave her the tips and tricks I use now along with resources.
I know there are many specialists in this area now popping up, and that makes me incredibly happy. I hope providers take the initiative to refer to them and ensure their patients are getting truly holistic supportive care.
I also hope, for my queer community, that these specialists take our stories and struggles into account as well when providing education and support. We have a LONG way to go in destigmatizing sexual health (especially queer sexual health) but we can start by just addressing the elephant in the room consistently — humans have sex, all sorts of sex, and its not shameful to want to keep sex and intimacy practices going after cancer.

Day 24 of Head & Neck Cancer Awareness Month
It’s always felt sort of serendipitous to me that the exact area used to create a tongue flap was right where I had a tattoo of an ankh and the words “one life” on my left arm, so now that message is where the bulk of my cancer used to be.
The words are part of a song (One Life, One Chance by H2O) that got me through many rough years of depression and anxiety in my late teens/early 20s, and my right arm has the other half of the phrase: “One chance” around a scarab.
I’ve always been a lover of metaphor and was incredibly fascinated by ancient Egyptian religion and mythology at the time and those symbols spoke to me as reminders that I was in control of my life & my prosperity — not in a physical sense necessarily, but in a “dogged determination and resilience to prove that I won’t back down regardless of what life throws at me” kind of way.
Maybe that’s why I’m still here, still fighting, still refusing to give up every time I’m knocked down. Still going even when I’m exhausted, feeling like I’m screaming to be heard without a sound, feeling like a tiny cog in a massive machine that cares nothing about how well I function because it thinks I’m easily replaced. I’m incredibly stubborn.
I’ve always learned differently, questioned the status quo, always searched for meaning and found it in places others wouldn’t look, and I’ve always chosen the overgrown, dark, scary path versus the well-lit, safe, paved one.
My parents would constantly ask me why I always had to choose the hard way of doing things. . . but maybe that stubborn determination to learn and do things my way is the exact same trait that has allowed me to become so resilient.

Photo taken from Stephanie Gayhart/LinkedIn
Source: Stephanie Gayhart/LinkedIn
At OncoDaily, we believe in the power of personal stories to inspire, educate, and unite. Sharing the experiences of cancer survivors like Stephanie Gayhart allows us to shed light on the realities of living with and overcoming cancer. Every story shared on OncoDaily contributes to our mission of raising awareness, promoting advocacy, and ultimately, improving the lives of those affected by cancer.
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023

Three weeks after surgeries were completed, in the beginning of October 2019, I started 6 weeks (30 treatment days) of radiation therapy.
Prior to beginning treatment, we made the lovely mask seen on me in the photo below. It was so tight to my face that I couldn’t open my eyes without my eyelashes hitting it. The only hole was for the bite block I had to keep in place to hold my tongue down.
Every day, Monday through Friday, for 30 days, I drove an hour to my treatment center, changed into a gown, and laid in the exact same position on the table. Every day the giant foam popsicle went into my mouth (which could barely open wide enough), the mask went on and locked me tightly to the table, the staff left and worked behind the safety of giant cement walls, and laser beams rotated around my skull and neck for a few minutes while I tried not to move or choke on my own spit.
That was the easy part.
See, the interesting thing about radiation is the treatment itself is painless. In fact, I felt nothing physical at all each time I laid on that table. The side effects are insidious and cumulative.
By the end of treatment, I legitimately felt like we had sucked away years of my life. . .so naturally I did what any millennial would do and made a meme about it referencing one of the greatest films of all time (this is not up for debate).
I’m not sure I would have survived this treatment without my ridiculous sense of humor.
Photo taken from Stephanie Gayhart/LinkedIn