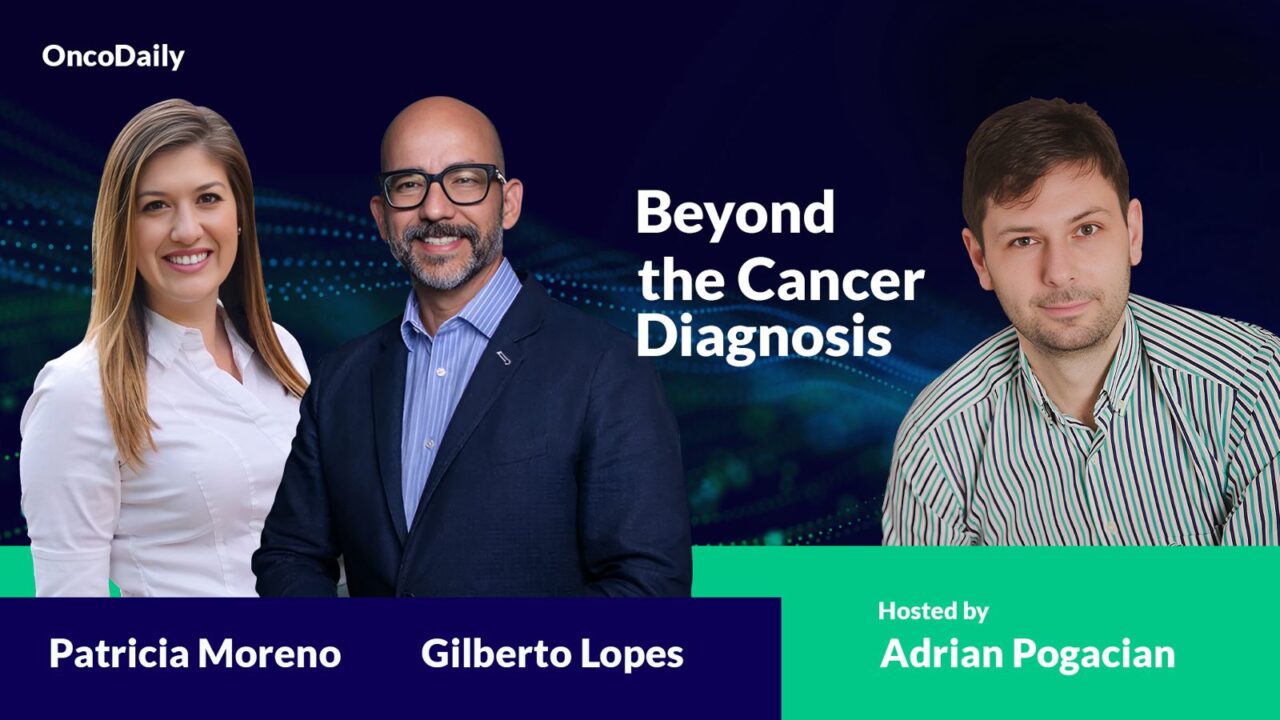
In this episode of ‘Beyond the Cancer Diagnosis‘ Adrian Pogacian discusses the challenges and the social impact of receiving cancer diagnosis centered around the Princess of Wales’ recent announcement with Dr Gilberto Lopes and Patricia Moreno from Sylvester Comprehensive Cancer Center, Miami.
Speakers
Patricia I. Moreno is a licensed clinical psychologist and an Assistant Professor in the Department of Public Health Sciences at the University of Miami Miller School of Medicine. Additionally, she holds the position of Lead for Evidence-Based Survivorship Supportive Care at the Sylvester Comprehensive Cancer Center.
Her focus is in discovering factors that can be addressed to enhance the quality of life and decrease cancer prevention and control disparities, particularly among Hispanic/Latino and diverse populations in the United States. Dr. Moreno heads the CARES Lab, dedicated to serving the cancer community through research, community engagement, and psychosocial support.
Dr. Moreno has been recognized, with numerous awards including the Early-Stage Investigator Award by the Academy of Behavioral Medicine Research (ABM), the Renewal Award by the National Institutes of Health (NIH) Loan Repayment Program, among others.
Gilberto de Lima Lopes Junior serves as the Medical Director for International Programs and Associate Director for Global Oncology at the Sylvester Comprehensive Cancer Center, alongside being the Chief of the Medical Oncology Division and a Professor of Clinical Medicine at the University of Miami Miller School of Medicine.
Additionally, he sits on the board of directors for the Union International for Cancer Control (UICC) and performs the role of Editor-in-Chief for the American Society of Clinical Oncology’s JCO Global Oncology. Previously, Dr. Lopes held positions at the Johns Hopkins University, including Assistant Professor of Oncology and Senior Consultant.
His research interests mainly goes around disparities, health economics, value, policy, and access to cancer drugs and care in low- and middle-income countries. Dr. Lopes has authored over 250 papers and has been involved as principal investigator, co-Principal Investigator, or steering committee member in over 200 studies and clinical trials.
Moderator
Adrian Pogacian,
Adrian Pogacian, MS Psychology, licensed clinical psychologist with executive education in Psycho-oncology, considerable time active in the field of Health Security, holding a degree in Global Health Diplomacy from Geneva Graduate Institute.
Currently, an advocate of Psycho-education in the field of oncology, researcher and associate lecturer with focus on Communication in Cancer Care, Coping with Cancer and Fear of Recurrence, working with young people and their caregivers on self-blame and disease acceptance.
Additionally, co-author of the first Romanian Pediatric Oncology and Hematology Guide Book, Founder of INCKA Psycho-oncology Center, ESO (European School of Oncology) Podcast contributor, Writer and Host Content in Psycho-oncology and Beyond The Cancer Diagnosis Interview Series at OncoDaily.com
Beyond The Cancer Diagnosis: Psycho-Oncological Aspects Of Kate Middleton’s Diagnosis
00:15 – Introduction
02:08 – Average age of cancer onset
2:47 – Sharing information about parents’ cancer diagnosis with children
8:07 – Talking with the patient about accepting the disease
10:43 – Preventive chemotherapy
12:37 – Is coping a fight between fear and hope?
15:46 – Coping strategies of the Princess of Wales
19:39 – How much time does the patient have?
21:46 – Anxiety, depression, and suicidal thoughts
25:23 – Level of education and acceptance of cancer diagnosis
About OncoDaily
OncoDaily was founded in 2023. It is a US-based oncology media platform, which features the latest news, insights, and patient stories from the world of oncology. Within a short period of time it became one of the leading oncology media platforms globally.
OncoDaily gathers content from various sources, including social media posts from renowned oncologists from all over the world, news from oncology societies and cancer centers, patient and survivor stories, and career-related information for professionals.
The mission of OncoDaily is to empower patients, survivors, and professionals with the knowledge and inspiration they need to fight cancer. The motto of OncoDaily is “Cancer doesn’t take a day off – neither do we”.
Follow the transcript below
AP: Hello again, Doctor Moreno. Hello again, Doctor Lopes. Thank you for being today with us. The subject is about the recent announcement of Catherine, Princess of Wales, known also as Kate Middleton, which came as a huge shock, but unfortunately, this announcement is part of a terrifying global trend. More and more young adults are diagnosed with cancer.
So I will begin with Doctor Lopes, asking him if he can tell us which is the primary cause of this issue of more and more young adults diagnosed with cancer.
GL: We don’t actually know. We have a number of different theories that are being tested and studied as we speak. Moving into cities without a doubt has led to this demographic transition that increases the number of cancers we see at all ages.
But over the last couple of decades, we are seeing younger patients developing colorectal cancers, breast cancers and others. We do imagine that air pollution has to do with patients developing lung cancer for instance, but we really don’t have a clear explanation for most patients.
There are specific cases where you have exposure to carcinogens, either because of occupational histories or because of environmental issues, such as in Antofagasta, Chile, for instance. But we really don’t have a good explanation for all of the most cases.
AP: And accordingly with this, can you tell us what is the average age of cancer nowadays?
GL: It continues to be a disease of older patients. So the vast majority of patients are in their sixth or seventh and even eighth decade of life when they develop cancer. But we are seeing more cancers that we used to see in older patients, in patients in their 30s and 40s and sometimes even in their 20s.
AP: I was asking you this, because in Romania, the average is between 35 and 40 years old. So, this was the reason. Now I’m passing to Doctor Moreno, talking about Catherine, Princess of Wales, who is both a mother and a daughter.
We agree in cancer that the emotional factor plays a powerful role, most often more powerful than the rational one. And should this information be shared with the children and why do some families, people avoid this sensible subject?
PM: Sure, as both of you were talking about, with this increasing incidence of cancer among people who are younger, younger adults who are having a diagnosis and young people either trying to start a family or who are parents of young children. And what we know is that cancer is painful and stressful for everyone. But we tend to see some of the highest levels of psychological distress among younger adults, particularly those between 18 and 39 years old.
The Princess of Wales is only in her early 40s, so she’s very young to be receiving a cancer diagnosis. And so the shock that she spoke about is not a surprise. And when you have young children, there becomes a decision about what to say to them and how much information to reveal. And that’s really a personal decision. It’s based on how old your children are. If they’re very, very young, there’s only so much information they can metabolize about the diagnosis or the treatment that the parent is receiving.
But we do know that most of the time it’s better to give children some level of information that’s developmentally appropriate. The not knowing or the uncertainty oftentimes is more difficult for children. And in particular, children tend to have a lot of magical thinking. And so they put together information that they have and so they can make conclusions about what the cancer means or how it happened. That’s really incorrect or can make them much more fearful.
Children are pretty concrete thinkers. They’re most interested in their lives and what will change and be different in their lives and what will stay the same. So there’s no need to go into kind of in-depth conversations about cancer biology or anything like that, but for them to have a basic level of understanding about what they’re seeing that’s different in their day-to-day schedules or in their day-to-day lives, or that they are able to visualize that’s different in their parent is the most important thing.
And kids are really resilient. I think that to your question about why do people avoid it? People avoid it because they’re scared. They’re scared that their children will become overwhelmed or that their children aren’t ready for that type of information. But most of the time, children who are confused or don’t have information, are left in the dark are actually the ones who struggle the most.
AP: Yeah, we all know that cancer means fear in the first place. That’s the first emotion. And according to this discussion about family, we all know that, family support, it’s half of recovery. So I will ask again, Doctor Moreno please, talk about the process of dyadic coping. If there is something like this, in this particular case.
PM: Yeah, yeah. The Princess of Wales talked about how important it has been for her husband to be by her side and what we know is that people who feel the support of their close loved ones, of their family, of their spouse, of their partner tend to do much, much better.
But it is a dyadic process because as, you know, Doctor Lopes and anyone who has treated people with cancer knows the pain of having your most loved, you know, spouse and partner affected by cancer is oftentimes as painful as for the person who has received the diagnosis. And so they’re both individually experiencing stress and emotional pain, and they’re both trying to support one another as well as figure out how to cope themselves.
And sometimes they don’t fully open up with one another because they’re trying to protect the other person from the stress that they’re experiencing, as they know that it affects their spouse or their partner. So it can be a little bit difficult.
And so oftentimes it’s really important for the couple or for the immediate family to have some additional support around them besides just the two of them or just, you know, the immediate family members because, everyone is affected in their own way, not just the patient who’s receiving treatment.
There’s a lot of hurt and, and coping that occurs by the spouses and the partners as well. but certainly having a loving family or a loving spouse by your side can make the experience much more tolerable and help someone get through the treatment and diagnosis.
AP: And now we know the psychological part. And now I’m, turning back to Doctor Lopes and ask him. How tough is for you, Doctor Lopes as an oncologist to discuss with your patients about the acceptance of this disease of cancer, because you are the first, who communicate the diagnosis and the first, that has to accept.
GL: Actually, we usually see patients at a moment when they have already heard that they have cancer and where unfortunately, even in the medical community, a lot of people take patients’ hopes away. And that is the worst that you can probably do, especially as today we do have a number of different treatment modalities that can help patients live longer and with much better quality of life, even if they have metastatic disease.
Not talking about the ability that we have today to find many, if not most, cancers at an early stage, at least for breast and colorectal. We certainly have that ability even for lung. Unfortunately, we don’t do as much of the screening CT scans we should be doing, but even for lung, we can actually find the disease early when we have a much better chance of cure. So cancer today is not a death sentence by any means.
We have a much better ability to not just prevent disease, such as by using hepatitis B and HPV vaccinations, for instance, but also with things such as tamoxifen or other modulators for patients that are at high risk of breast cancer, we can prevent colon cancer by finding polyps and removing them before they become cancer. So the possibilities today are not what the question actually started with.
Of course, when we do have patients with disease that is metastatic and might be beyond our ability to cure today, even those patients have hope in a number of different treatments. In lung cancer, we have a growing number of patients who are alive five and more years after diagnosis of advanced disease because their disease has responded to immunotherapies or targeted agents.
So it’s certainly not that idea, at least where treatments are available and where the health care systems actually are able to have patients access them. Of course, when we do talk globally, then it’s absolutely right. Most patients in low middle income countries in particular, do not have access to a lot of the technologies that I just mentioned, and especially not to many of our new treatments that are making such a difference to so many patients in the US.
AP: You talk about some of the procedures in oncology, and I noticed that, regarding this particular case, everyone on social media was talking about this preventive chemotherapy. Can you explain us a little bit because, I guess, there will be a tendency now for people not so informed to do it by themselves.
GL: Preventing cancer with chemotherapy. So unfortunately for that, except for the case that I just mentioned, when you have women that are at high risk of breast cancer and we can use tamoxifen and other modulators, we don’t have any diseases where chemotherapy prevents a new cancer. So we usually call preventative chemotherapy adjuvant chemotherapy.
And what that means is if you do have a disease that we can remove surgically, let’s say if you have an ovarian cancer or a breast cancer or lung cancer, depending on that tumor’s characteristics and the patient’s characteristics, we would be able to provide certain treatments that can try to help the disease from coming back. So try to prevent the disease from coming back.
Some of these treatments are chemotherapy. So medications are classically seen as chemotherapy agents. But we also have hormone treatments for breast cancer. We have immunotherapies. We have targeted agents for lung cancer and others. So there’s a huge number of potential treatments that we can use in what we call the adjuvant setting technically as medical oncologists.
And these are modalities of treatment that can try to help the disease from coming back or at least prolong the time that a patient is disease free.
AP: Okay. Thank you very much. Doctor Moreno, I will ask you, let’s say direct question is the following statement true or false codes? Coping. It’s a fight between fear and hope at the end.
PM: I would say false. As a psychologist, I think we try to move away from binary options, you know, one or the other. You can have hope and still be scared. I think anybody who receives a cancer diagnosis will have some level of fear. That’s normal. It’s expected. And we don’t want to pathologize that. We don’t want people to expect that they have to be sort of a happy soldier or a happy fighter all the time.
Of course, if someone gets to a level of psychological distress that is really impairing their ability to follow through with their care or is really affecting their lives, we’re going to treat that and we’re going to make sure that they have the right level of care in order to be as well as possible emotionally and physically.
But we don’t want to set the expectation that someone can’t be afraid, that they can’t have some level of frustration or anger, that this is happening, that it’s interrupting their life, that it’s affecting their ability to be with their family in the way that they would like, or to work in the way that they would like, especially for younger adults.
It really disrupts the course of their lives, and which is why it’s so distressing. So you know, hope is such a beautiful word and it means so many different things for different people.
Doctor Lopes talked about hope can mean one thing for a person with early stage cancer. Hope can mean something very different for another person, and you can have hope through the end of your life. You can hope for comfort. You can hope for time with your loved ones. That is important and allows you to make sense of the arc of your life.
I mean, hope can take many, many different shapes. but I think we just want to make sure that people understand that the expectation is not that they have to carry this experience in any one particular way. It’s okay to have the full continuum of emotions. And the fact is that most people will, and that’s normal.
And I think it’s very freeing for people to know that many other people in that situation would experience shock, fear, frustration, maybe even anger, sadness. You know, all of that is normal. And that’s why we work as a multidisciplinary team to make sure that we do really take care of people who need an extra layer of support for their emotional health.
But we don’t want to set the expectation that people can’t have hope and fear or hope in any other emotion that’s more complex or layered.
AP: So, coping is more about progress than victory.
PM: Yeah coping is about living as well as possible within the circumstances of your life you know, there are going to be challenging aspects to undergoing treatment.
But within, you know, those challenging experiences of, you know, surgery or chemotherapy or having to pause certain activities, are we able to give you the support that you need to be as well as possible physically and emotionally in that experience? And that can look so different for every person.
AP: And regarding this particular case, can you give us, for example, three coping strategies that the Princess of Wales can apply on the other coping?
PM: Yeah. I mean, like I said, it is individual, but she named two of the most important things. She has the support of her loved ones. And she also talked about being taken care of by a really great medical team. And we know that when people have a strong alliance with their oncologist and with their oncology care team, when they feel like they have good communication and that they’re on the same page, they trust them.
They’re making decisions together about what’s best for, you know, her and her care. Those are some of the two most protective factors. If you have a really good social support system around you, and you have a strong and trusting relationship with your care team, that sets you up for success every time, even in all of the other challenges.
And then beyond that, it becomes about, you know, every day just asking yourself, what are the small things I can do that bring me a little bit of joy, bring me a little bit of comfort, and that can be very different.
You know, for some people it’s going to be spending time outside or making time to connect with their art or whatever is, you know, already the values and the priorities that they have had before cancer, you know, people become full formed humans before cancer ever enters their lives.
And it’s just about trying to keep them connected to what makes them themselves through the cancer treatment as much as possible, even when there are other challenges that are coexisting.
AP: Okay, I’m, returning to Doctor Lopes and asking also, let’s say direct question, how important is time in the oncological process? Because I’m coming from Eastern Europe where cancer is still, let’s say, a non curable disease. And you talk in, in the West as a curable disease. So it’s kind of two different approaches. But in any of them, time, how important is for patient time?
AP: Doctor Lopes, the second last question will go to you. In oncology is the therapeutic approach in this last period more conservative or not. Because we do hear a lot about this particular subject.
GL: It depends what you are talking about. Time. time is what we try to gain. Try time is what we try to help patients have more of so that they can do what’s important to them, be it to reach a loved one’s wedding or a grandchildren being born. So in that sense, time is a philosophical concept. That is everything we are trying to gain for our patients and for ourselves in many ways as well.
But if the question is more direct about how time or how much time do you have to actually start the treatment? That varies a lot. That depends on the type of treatment, depends on the stage of the disease. Of course, we do want to have treatment as early as possible, but that doesn’t mean starting treatment today or tomorrow, or even this week or this month for certain diseases.
They are so indolent that starting treatment in six weeks, three months or six months might actually be enough. There are patients that have diseases that we would call cancer, but probably eventually will change the nomenclature in the future, like some prostate cancers, for instance, that are low grade, you could go for years without any treatment.
On the other hand, if you have somebody with a small cell lung cancer and you don’t treat that disease within a couple of weeks, patients are likely to get worse and even more aggressively. If you have someone with leukemia or an aggressive lymphoma such as Burkitt’s lymphoma, you do need to start treatment within a few days. Otherwise you do impact prognosis adversely. So it is a very broad concept, both philosophically and practically.
AP: I ask you this because, every oncological patient, when heard about this diagnosis said I don’t have time. So the oncological patients don’t have time, don’t have space. And this is the first question, how much time do I have? You know to live or if I came, on time or I postpone because usually, bad news, we intend to postpone them. Yeah.
GL: There’s one more important aspect that has to do with your question, which is, we really can’t precise for each individual, for each person we’re seeing in front of us as a medical oncologist, how long each of us has, even us without disease, because what we get are statistics. And the statistics that we get are, number one, usually old and outdated because they reflect what happened. The treatments that we were giving five years ago.
If we’re looking at five year survival and we also get aggregate numbers, so we get average numbers, we know that half of the patients are going to live less than that number that we get, and half of the patients are going to live more and longer. So we really can’t precise for each person. And I think that that’s an important message.
If we are in a system, in a health care system where we actually have new treatments coming along, those updates, those numbers that you get on the internet are usually outdated, and they are average, and an average is just the midpoint. that may not show, for instance, that 15 to 30% of patients with lung cancer today, even with metastatic disease, can actually get to live for five years or longer as compared to 3% or less a decade ago.
And as you mentioned, it’s extremely important the systems and the ability to get access to new treatments, because if you don’t get any treatments, cancer is still a very dismal disease in many, many ways.
AP: Thank you. I’m turning back now to Doctor Moreno. I asked him, Doctor Lopes, about time. Now I want to ask you about this. let’s say triad of which every, oncological patient have anxiety, depression and suicidal tentatives, regarding these issues So how important is psycho oncological education or psycho oncological awareness?
PM: Yeah, yeah, the stress of course, is so important. And it affects almost every person who receives a cancer diagnosis. I think it is important to know, though, that most people have some level of anxiety or fear, concern, some level of change in their mood that might be sadness or along the continuum of depressed mood, but most people don’t actually develop an anxiety disorder or a depressive disorder or a clinical depression.
That was something that we used to think or we used to assume that, oh, cancer is so stressful. It’s so difficult. Most people who get a diagnosis of cancer must go on to have a clinical level of anxiety and depression, and that’s not always true. Just because people are not at their typical baseline and you see more emotional richness, including anxiety and depressed mood in their experience as a response to the diagnosis and to the challenges of treatment.
Most people actually fare relatively well. It’s less than a third or less than a quarter of people who have clinical levels of anxiety and depression. And what we found is that actually, most people don’t have elevated suicidal ideation. When you look at the cancer community as a whole or people who have a diagnosis of cancer as a whole, you tend to see rates of suicidal ideation, as the sort of comparable levels as the general population. So you don’t always see an increased risk for that.
There are specific cancers, maybe that are higher risk if the treatments are really, really difficult to tolerate or if the impact physically of that treatment is really difficult to tolerate, then we might be looking for that. But the most important thing is most people do pretty well and we always, in our healthcare system make sure that we are screening for higher levels of psychological distress, so higher levels of anxiety or of depressed moods.
So when it hits that threshold that it’s clinically impacting them, it’s impacting their ability to, you know, go about their day to day lives to go through their treatment. It’s impairing them or it’s just so overwhelmingly distressful. Then we have the resources to make sure that we address that.
And part of that screening is to also make sure that if someone were struggling and to the point that they had suicidal ideation, that we would also identify that through our screening and make sure that subgroup of patients that do need an extra layer of support for their emotional health receives that, additional layer of support for their emotional health.
So I think it’s important, though, not to assume that every single person will have a clinical level of anxiety or depression, or will experience suicidal ideation as a result of their diagnosis and treatment. We have some pretty good epidemiological data at this point to know that the rates tend to be much lower than we initially assumed, given the challenges inherent.
AP: Okay, I see that we are approaching the final of the interview. I will ask one more question. Regarding the last one about anxiety, depression. How much do you think that the level of education interferes in accepting the oncological disease?
I mean, if I’m a PhD or, I don’t know, doing lifelong learning, maybe I can accept better than a person who didn’t have the chance to, make a formation, for example, or it executive education. Do you think that the level of education has an impact on acceptance of cancer?
PM: Yeah. I mean, I’m going to reframe the question a little bit. So I don’t think that people who have lower levels of education have an inherently harder time accepting their diagnosis of cancer or their experience what we know to be true in our country and in many places around the world, most places around the world, I would argue, is that people with lower socioeconomic resources, which tends to, coincide with lower levels of education, tend to receive lower quality care, and they have a harder time accessing care, period.
And they have a harder time accessing high quality care. And so we know that when they receive care, they may not be included in the decisions about what treatments to get, what will treatment look like, what’s important to them, and the communication between them and their care team oftentimes is different.
You know, they may be given less opportunities to ask questions. They may have less sort of education or information given to them. And this could be because of our own sort of institutional biases against people who have lower socioeconomic resources.
And so I think that anyone, given the appropriate level of support and care can move through this experience as well as possible. Of course there are challenges, but I don’t think that there’s anything inherent to, you know, anybody who might have a lower level of education, not being able to cope with the illness or not being able to accept the need for cancer treatment following a diagnosis.
It’s really about these systemic structural, institutional, barriers to high quality care. And high quality care goes hand in hand with making sure that patients have the level of support that they need in order to make sense of the diagnosis, to understand the information that’s being given to them, and to participate fully from an empowered place about what, you know is going to come now with treatment and moving forward through their care.
AP: Thank you. Thank you very much.