
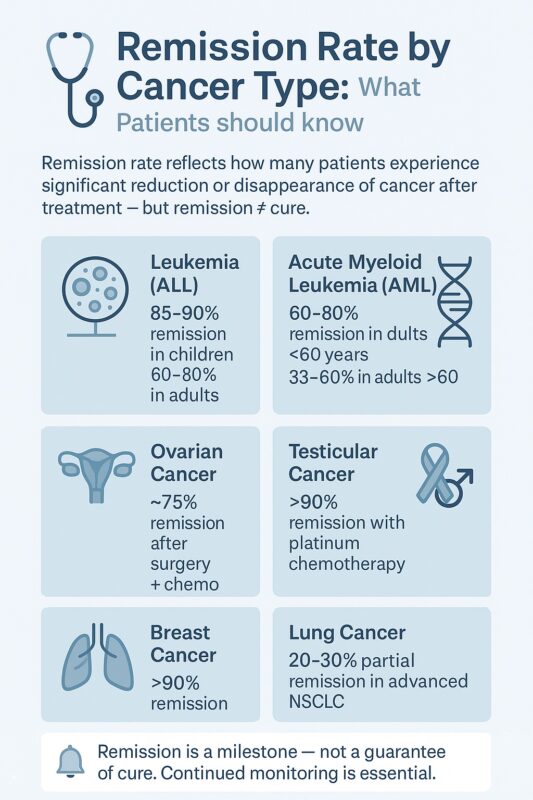
Understanding Remission Rate in Cancer: Key Insights for Patients
When a patient begins cancer treatment, a word that often emerges early in conversations is “remission.” While it is commonly associated with recovery or even cure, the concept of remission — and, by extension, remission rate in cancer — is more complex. A clear understanding of what remission means, how it differs from cure, what remission rates reflect, and why it matters can empower patients to navigate their cancer journey more confidently and realistically.
What Does Remission Mean?
In oncology, remission refers to a decrease or disappearance of signs and symptoms of cancer following treatment (National Cancer Institute [NCI], n.d.). Remission can be complete or partial:
- Complete remission (CR) is defined as the absence of detectable disease based on imaging, clinical examination, and laboratory testing (NCI, n.d.).
- Partial remission (PR) describes a significant reduction in tumor size or cancer burden, typically by at least 30%, but with residual disease remaining (American Cancer Society [ACS], n.d.).
Importantly, remission does not always mean the cancer has been eradicated. Even during a complete remission, microscopic cancer cells can remain undetected in the body (RBOI, 2018). As a result, remission is considered a critical milestone but not necessarily the final step in cancer care.
How Does Remission Rate Differ from Cure Rate?
The remission rate is a key measure used in clinical trials. It describes the proportion of patients whose disease responds to treatment — either with a significant reduction (partial remission) or complete disappearance (complete remission) of measurable cancer (ACS, n.d.).
Read About Clinical Trials in Cancer Care on Oncodaily
In contrast, the cure rate refers to the proportion of patients who remain disease-free for an extended period, often five years or more, with no evidence of recurrence (BSW Health, n.d.). While remission rate reflects the short-term success of therapy in reducing cancer burden, cure rate addresses long-term outcomes.
For example, in pediatric acute lymphoblastic leukemia (ALL), up to 95% of children can achieve complete remission within weeks of starting therapy, but the five-year cure rate is about 80–90%. For acute myeloid leukemia (AML), remission rates are reported at approximately 60–80%, yet the five-year survival rate — a proxy for cure rate — is lower, ranging around 24%.
This distinction is critical for patients to understand because a high remission rate may not always translate into a high cure rate.
Why Does Remission Rate Matter?
For patients and families, remission rate offers a snapshot of how well a particular therapy works to shrink tumors or eliminate visible disease (ACS, n.d.). It helps patients evaluate different treatment options and set realistic expectations. However, remission rate is population-based; it indicates how many people achieved remission in a clinical trial or observational study but does not predict an individual patient’s outcome (RBOI, 2018).
Knowing this distinction can help prevent misunderstandings that could lead to over-optimism or unwarranted pessimism. Informed patients are better positioned to discuss next steps, including maintenance therapy and follow-up plans, with their care team.
What Factors Influence Remission Rates?
Remission rate in cancer vary widely across treatment regimens, and patient characteristics.
Cancer Type and Stage
Some cancers are inherently more responsive to treatment. Blood cancers such as ALL and Hodgkin lymphoma have high remission rates with modern therapy — often exceeding 80–90% — while pancreatic cancer and metastatic lung cancer tend to have much lower remission rates (Reuters, 2024).
Disease stage is another critical determinant. Early-stage cancers generally achieve higher remission rates than advanced-stage or metastatic disease, because they are localized and easier to eradicate with surgery or systemic therapy (ACS, n.d.).
Treatment Regimen
Therapies themselves play a major role. For instance, platinum-based chemotherapy leads to remission rates exceeding 90% in testicular cancer (BSW Health, n.d.). By contrast, response rates in metastatic melanoma, even with modern immunotherapy, remain modest, though improving over time (Reuters, 2024).
Recently, innovative therapies such as CAR-T cell therapy have led to long-lasting remissions in relapsed or refractory hematologic malignancies (The Guardian, 2025). In one reported case, a patient treated with CAR-T therapy remained in remission for over 18 years and went on to have two children (The Guardian, 2025).
Patient-Specific Factors
Remission likelihood also depends on patient characteristics. Younger patients tend to achieve higher remission rates than older patients with the same disease. In AML, for example, remission rates among adults under 60 can approach 60–80%, compared to 33–60% in patients over 60.
Additionally, genetic and molecular features of tumors can influence response. Certain chromosomal abnormalities in leukemia, for instance, are associated with more favorable responses to induction therapy.
Read About Breast Canceer Success Rate on OncoDaily
How Is Remission Monitored?
Achieving remission is only part of the journey. Once remission is reached, close surveillance is critical to detect relapse early and intervene promptly (ACS, n.d.). Typical follow-up includes:
- Regular physical exams and symptom checks.
- Imaging tests (e.g., CT, MRI, PET scans) to monitor internal disease status.
- Laboratory testing, including tumor markers and, in hematologic cancers, minimal residual disease (MRD) detection.
Follow-up schedules depend on cancer type and risk profile but often involve visits every three to six months initially, extending to annual visits after five years for many cancers (ACS, n.d.).
Relapse, Maintenance Therapy, and Survivorship
Relapse remains a significant concern even after prolonged remission. For example, certain breast cancers can recur decades after initial treatment (Cancer Therapy Advisor, n.d.). In some cancers such as ALL, maintenance therapy — additional treatment given even after remission is achieved — reduces relapse risk and prolongs disease control.
Survivorship also involves managing late effects of cancer therapy, from cardiovascular risks to secondary cancers. Many survivors need ongoing care not only to monitor for recurrence but also to maintain quality of life and address long-term treatment complications.
Progress in Cancer Outcomes
The progress in cancer treatment is reflected in national trends: U.S. cancer death rates have dropped by one-third since 1991, reflecting improved therapies and early detection. Childhood cancer survival rates, in particular, have dramatically improved, with five-year survival now exceeding 80% for many cancers.
This progress, however, should not obscure the ongoing need for individualized, vigilant care. Understanding what remission and remission rates represent is part of the modern patient’s toolkit for informed participation in their care.
Summary
In summary, remission rate describes the proportion of patients whose cancer shrinks or disappears after treatment, but it does not equate to cure rate, which reflects long-term survival without recurrence (ACS, n.d.). Patients in remission require ongoing monitoring, and their outcomes depend on cancer type, stage, treatment, and individual characteristics.
While remission is a significant milestone and often a source of hope, it is not the endpoint for many patients. With the emergence of innovative therapies such as immunotherapy, targeted agents, and CAR-T cell treatments, remission rates and the durability of remission are improving, but vigilance remains key.
Understanding these terms allows patients and families to have informed discussions with their oncology teams, set appropriate expectations, and remain engaged in their care journey.
You Can Watch More on OncoDaily Youtube TV
Written by Armen Gevorgyan, MD
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
