MASCC 2025 Highlights: Gut Microbiota as a Novel Target for Managing Chemotherapy-Induced Neurological Toxicities
At the MASCC 2025 Annual Meeting, Associate Professor Hannah Wardill, NHMRC Investigator and head of the Supportive Oncology Research Group, delivered a groundbreaking talk urging the oncology community to rethink the management of neurotoxic side effects of cancer therapies. Her presentation highlighted the limitations of current interventions for chemotherapy-induced peripheral neuropathy (CIPN) and cancer-related cognitive impairment (CRCI), emphasizing the gut-brain axis as a promising and underexplored therapeutic target.

Persistent Symptoms, Poor Solutions
Neurotoxicity—including peripheral neuropathy and cognitive impairment—is a common and debilitating consequence of modern cancer therapies. As Wardill noted, oxaliplatin, used in colorectal cancer, and proteasome inhibitors, used in multiple myeloma, are among the top offenders, with peripheral neuropathy affecting up to 60% of patients.
These symptoms are not transient: many patients experience pain, numbness, and cognitive deficits that persist for months or years, disrupting daily life, social participation, and employment.
Despite this burden, current clinical guidelines offer few effective options. ASCO and ESMO guidelines both acknowledge the lack of preventive agents and recognize duloxetine as the only pharmacological treatment with some evidence for CIPN—though even its benefit is limited.
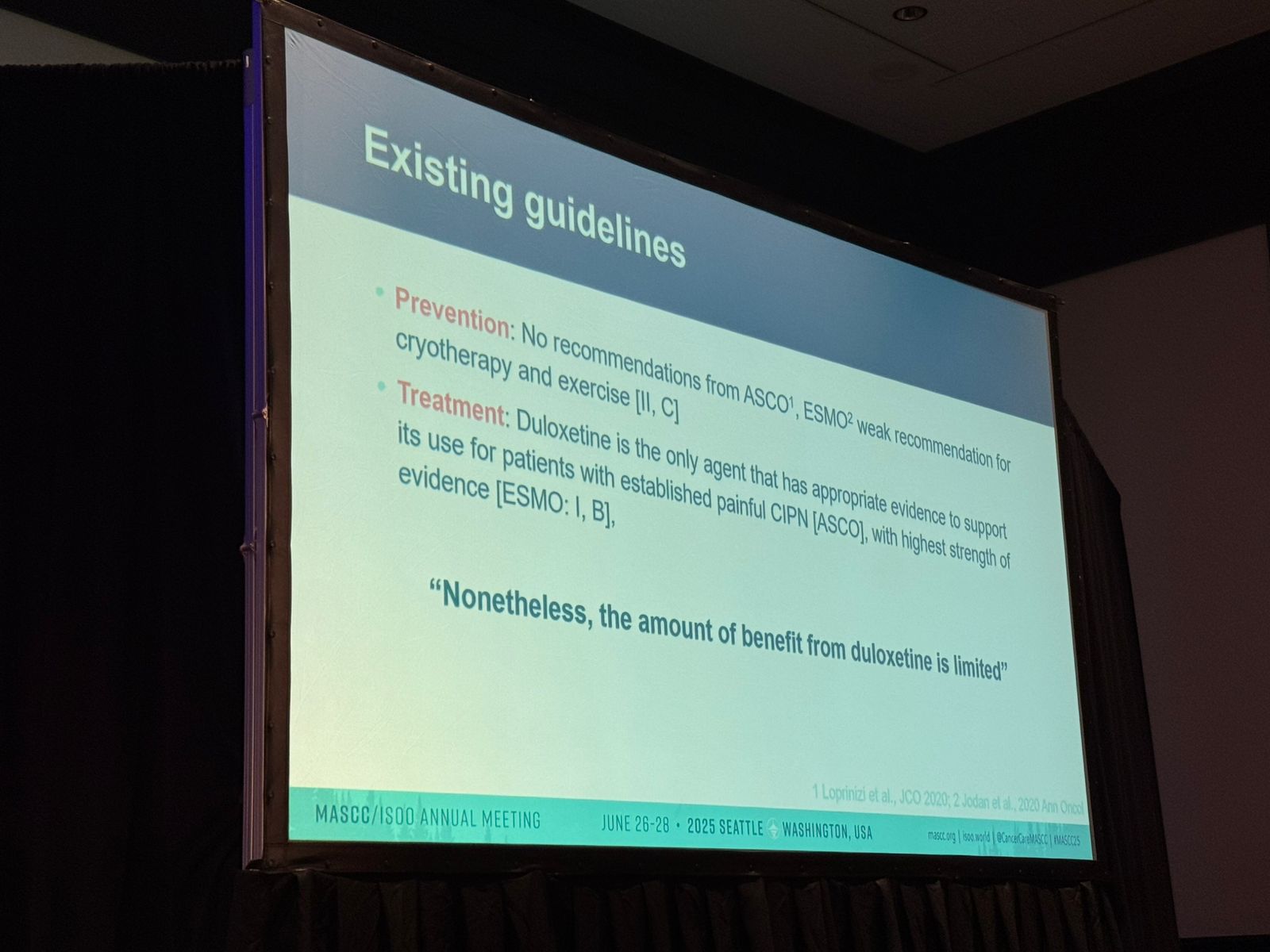
In practice, patients often resort to off-label or non-prescribed treatments. In a MASCC-led survey of 447 individuals with PN, only 8% were using duloxetine, while 33% used gabapentin (not guideline-recommended), and 49% turned to non-prescribed supplements or medications. Nearly a third expressed preference for a “pill” over lifestyle interventions—yet such options remain limited.
Cognitive impairment, especially prevalent in breast cancer and HSCT survivors, is even more poorly addressed. Guidelines are sparse, and the condition is often misattributed to stress or dismissed altogether.
A New Direction: The Gut-Brain Axis and Microbiota
Recognizing the failure of conventional neuroprotective strategies, Wardill presented a compelling case for targeting the gut microbiota, which plays a central role in gut-brain axis signaling and neuroinflammation.
The gut microbiota is now understood to exert systemic influence on the central and peripheral nervous systems via immune modulation, microbial metabolites, and barrier integrity. Cancer therapies disrupt this ecosystem, and growing evidence suggests that such disruption contributes directly to neurological side effects.
Key preclinical findings include:
- Rodent models treated with paclitaxel or oxaliplatin experience neuropathic pain, which can be attenuated by disrupting or modifying gut microbiota.
- Germ-free mice receiving microbiota transplants from chemotherapy-treated mice develop pain phenotypes, suggesting a causal microbial link.
- Temporary microbiota depletion protects against oxaliplatin-induced hyperalgesia, despite irreversible nerve damage.
These insights shift the paradigm: neurotoxicity may not only be nerve-intrinsic but also microbiota-modulated.
Human Studies and the Path Forward
Wardill’s group is actively advancing this field with two novel studies:
- A human-to-mouse fecal microbiota transfer study, assessing whether neuropathy symptoms can be transferred via microbiota.
- A clinical trial investigating encapsulated fecal microbiota transplantation (FMT) in auto-HSCT recipients—with peripheral neuropathy included as a secondary outcome.
- While still in early stages, these studies represent a radical rethinking of how we understand and potentially treat neurotoxic symptoms.
Mechanisms and Intervention Strategies
The pathways remain complex. Microbiota may affect:
- Neuroimmune responses
- Blood-brain barrier permeability
- Cytokine-driven inflammation
- Nociceptive signaling modulation
This opens the door to interventions such as:
- Direct microbial therapies (probiotics, FMT)
- Prebiotic fiber to fuel beneficial bacteria
- Postbiotics, i.e., microbial-derived metabolites with anti-inflammatory or neuroprotective properties
Conclusion: A Call to Action
Wardill closed with a powerful message: Conventional pharmacologic strategies have failed, and a microbiota-informed approach may offer a new frontier. She urged researchers and clinicians to include neurotoxicity-related endpoints in future trials of microbiome-targeted interventions and to recognize these symptoms as treatable and biologically rooted, not inevitable.
With deeper mechanistic insights and integrated clinical designs, the gut-brain axis may be key to restoring neurological function and quality of life in cancer survivors.
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
