Vascular Endothelial Growth Factor inhibitors (VEGFi), family comprises several secreted glycoproteins, widely used to treat advanced cancers and ocular diseases, may cause significant adverse effects.
This article explores the ocular side effects of anti-VEGF therapy, including intraocular inflammation, increased intraocular pressure (IOP), and endophthalmitis. We will also discuss the risk factors, mechanisms, and clinical implications of these adverse events, providing insights into their management and strategies to minimize complications.
The Painter’s Eye, 1941(El ojo del pintor, 1941) – art print Salvador Dali
How Does Anti-VEGF Therapy Work?
VEGF inhibitors are used in cancer therapy to block angiogenesis, the process by which tumors develop new blood vessels to sustain growth and metastasis. These agents include monoclonal antibodies, such as bevacizumab and ramucirumab, as well as tyrosine kinase inhibitors like sunitinib and sorafenib. Often combined with chemotherapy or radiation, VEGF inhibitors enhance antitumor effects by improving drug delivery and reducing tumor vascularization.
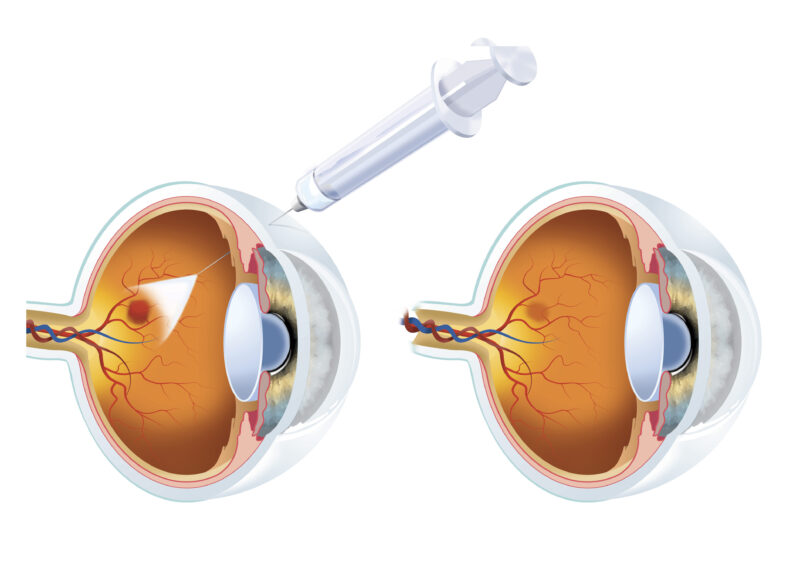
Ocular toxicity from VEGF inhibitors is a concern due to both local and systemic effects. Locally, intravitreal injections can lead to complications like endophthalmitis, increased intraocular pressure, retinal detachment, and ocular surface disease. Systemically, VEGF inhibitors can cause nephrotoxicity, thrombotic microangiopathy, and worsening hypertension or proteinuria, as they may reduce systemic VEGF levels, affecting kidney function and vascular health. These systemic effects highlight the importance of monitoring patients for potential systemic complications when using VEGF inhibitors, even when administered locally for ocular conditions.

A 16-year-old female with tuberous sclerosis complex presented with an aggressive, rapidly growing retinal astrocytic hamartoma despite 6 intravitreal anti-VEGF treatments administered monthly (A). Sirolimus (2 mg/day) was initiated. At 20 months follow-up, near complete regression of the tumor was observed (B). The initial exudation present on optical coherence tomography (C, top panel) completely resolved with mTOR therapy (C, lower panel). The patient’s visual acuity improved from 20/30 at baseline to 20/20 with treatment. Image courtesy Mary E. Aronow, MD.
How VEGF Supports Normal Vascular Function and Retinal Health?
Vascular Endothelial Growth Factor (VEGF) is essential for maintaining vascular function through multiple mechanisms. It plays a key role in angiogenesis and vasculogenesis, stimulating endothelial cell proliferation and migration to support new blood vessel formation during embryonic development and tissue repair. Additionally, VEGF enhances vascular permeability, allowing nutrients and oxygen to reach tissues, particularly in response to hypoxia, by inducing a fenestrated phenotype in endothelial cells.
Beyond vessel formation, VEGF promotes endothelial cell survival through anti-apoptotic signaling pathways, ensuring vascular integrity and preventing vessel regression. In specific tissues like the eye, VEGF supports retinal blood vessel stability, helping to maintain vision. However, dysregulated VEGF levels can contribute to ocular diseases such as age-related macular degeneration and diabetic retinopathy.
VEGF and Its Role in Angiogenesis
VEGF is a key regulator of angiogenesis, the formation of new blood vessels. It primarily signals through two endothelial receptors, VEGFR-1 and VEGFR-2, triggering pathways that support endothelial cell survival, proliferation, migration, and vascular permeability.
While VEGF is essential for physiological processes like embryonic development and wound healing, it also plays a central role in disease, particularly cancer. Tumors exploit VEGF to drive excessive angiogenesis, ensuring a sufficient blood supply for growth and metastasis. VEGF interacts with VEGFR-3 to promote lymphangiogenesis, further aiding tumor spread.
What Are the Dual Roles of VEGF Inhibitors in Cancer and Eye Care?
VEGF inhibitors are essential in both oncology and ophthalmology, where they target pathological angiogenesis to control disease progression. In oncology, these agents disrupt the blood supply that sustains tumor growth and metastasis. Bevacizumab (First approved by FDA on Feb 26, 2004), a humanized monoclonal antibody, binds VEGF to prevent receptor activation and is FDA-approved for cancers like metastatic colorectal and non-small cell lung cancer, often used with chemotherapy.
Aflibercept (first approved by FDA on Nov 18, 2011) , a fusion protein acting as a decoy receptor, neutralizes VEGF activity and is used in metastatic colorectal cancer. While primarily used in ophthalmology, ranibizumab (first approved by FDA on June 30, 2006) also has potential oncology applications due to its VEGF-inhibiting properties.
In ophthalmology, VEGF inhibitors are vital for treating conditions such as age-related macular degeneration (AMD) and diabetic retinopathy, both driven by excessive angiogenesis. Anti-VEGF therapies like ranibizumab and aflibercept reduce abnormal retinal blood vessel growth, helping to preserve vision and prevent disease progression. By targeting VEGF, these inhibitors play a crucial role in managing both cancer and vision-threatening disorders.
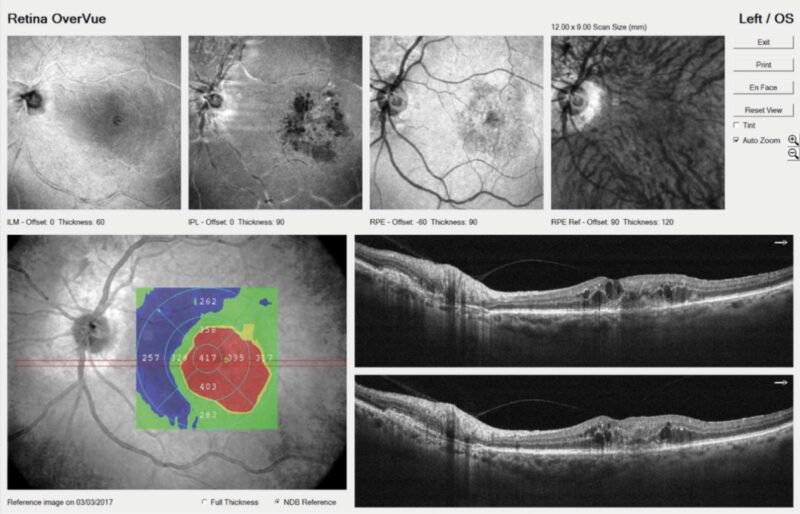
OCT imaging shows the left eye of an 81-year-old CNVM patient with intraretinal fluid. He’ll be treated with intravitreal anti-VEGF injections.
Ocular Side Effects of Anti-VEGF Therapy
While VEGF inhibitors effectively block pathological angiogenesis in oncology and ophthalmology, they can also lead to various ocular adverse effects.
Conjunctival hemorrhage, vitreous floaters, rhegmatogenous retinal detachments, and retinal hemorrhage are primarily attributed to mechanical trauma during injection.
Intraocular Pressure (IOP)
Intraocular pressure (IOP) is the fluid pressure within the eye, critical for maintaining its shape and proper function. It is regulated by the production and drainage of aqueous humor, a clear fluid produced by the ciliary body behind the iris. A normal IOP range is typically between 10–21 mmHg. Elevated IOP can lead to ocular hypertension, which, if left untreated, may result in glaucoma. Glaucoma is a group of eye diseases that damage the optic nerve, potentially causing irreversible vision loss. On the other hand, low IOP, though rare, can cause problems like retinal detachment or optic nerve damage. Proper regulation of IOP is essential for the health of the eye.
Anti-VEGF agents are typically administered in volumes of 0.05–0.1 mL, causing a transient rise in intraocular pressure (IOP) to 30–50 mm Hg due to the sudden increase in volume. This acute elevation normalizes within an hour. However, repeated intravitreal injections have been associated with persistent ocular hypertension (IOP >25 mm Hg post-injection), often requiring long-term IOP-lowering therapy. Proposed mechanisms include microparticle obstruction of the trabecular meshwork and direct VEGF inhibitor-induced effects on trabecular meshwork cells. Kampougeris G, Glaucoma Pract. 2013
Brolucizumab-Associated Retinal Vasculitis (BARV)
Brolucizumab (Beovu) was approved by the US FDA in October 2019 for treating neovascular age-related macular degeneration (n-AMD). It is the smallest type of antibody, called a single-chain antibody fragment (scFv), and is the first of its kind approved in medicine. Brolucizumab works by blocking VEGF-A, a protein that causes abnormal blood vessel growth in the eye, helping to reduce fluid leakage and stabilize vision in patients with n-AMD. Its smaller size may allow for fewer injections compared to other treatments.
Brolucizumab is primarily used to treat neovascular (wet) age-related macular degeneration (AMD) and diabetic macular edema (DME). It was approved in 2019 for AMD, helping to reduce abnormal blood vessel growth and fluid leakage under the retina, thus stabilizing vision. In 2022, it was approved for DME to treat visual impairment caused by fluid accumulation in the retina due to diabetes.
Brolucizumab is under preclinical development for potential use in treating Kaposi sarcoma and glioblastoma, expanding its therapeutic potential. Eason AB, Cancer Res. 2018
The most likely explanations involve severe vascular perfusion reduction, particularly in eyes with already compromised retinal blood flow, or local production of anti-brolucizumab antibodies. Vasculitis can affect arteries, veins, and capillaries, leading to arterial narrowing, occlusion, and perivascular sheathing. Retinal ischemia may present with whitening, cotton wool spots, intraretinal hemorrhage, and pericentral acute middle maculopathy. Cox J.T., J. Clin. Med. 2021
Infectious Endophthalmitis
Infectious endophthalmitis is a serious, potentially vision-threatening infection that affects the interior of the eye, typically involving the vitreous body and anterior segments. As one of the ocular side effects of anti-VEGF therapy, this condition can occur following intravitreal injections, often due to the introduction of bacteria, fungi, or other pathogens into the eye. The resulting intense inflammation can progress rapidly, leading to severe pain, blurred vision, and, if left untreated, permanent vision loss or blindness.
The primary cause of infectious endophthalmitis is the introduction of bacteria or fungi into the eye during the intravitreal injection procedure. Despite the use of strict aseptic techniques, contamination can still occur at various stages. This includes contamination from the needle or syringe, which may come into contact with non-sterile surfaces. The skin around the injection site, despite being disinfected, can also serve as a source of pathogens if proper cleaning procedures are not followed or if there is a break in sterile technique.
The most common presenting symptom of endophthalmitis is reduced visual acuity, followed by pain, photophobia, redness, floaters, eyelid swelling, and discharge. Key clinical signs include vitritis, hypopyon, conjunctival hyperemia, corneal edema, and elevated intraocular pressure. Several factors contribute to the risk of endophthalmitis, including patient-specific, medication-specific, and delivery-specific factors. Notably, some patients have been found to develop anti-idiotype antibodies against anti-VEGF agents, which may play a role in immune-related ocular inflammation. Sanjeewa et al., 2008
Dry Eye Syndrome
Dry eye syndrome is a chronic inflammatory condition of the ocular surface, characterized by symptoms such as burning, itching, a gritty sensation, excessive tearing, conjunctival redness, foreign body sensation, and blurred vision. These symptoms are linked to clinical markers, including tear hyperosmolarity, elevated inflammatory mediators, and abnormal tear production. Calonge et al., 2010
Patients undergoing prolonged anti-VEGF treatment commonly experience dry eye symptoms, often due to repeated exposure to preservatives in antibiotic eye drops, which can exacerbate ocular discomfort. Ayaki et al., 2012 Since tear hyperosmolarity plays a central role in the pathophysiology of dry eye syndrome, it serves as a valuable marker for diagnosis, monitoring, and management of chronic ocular conditions. Versura et al., 2010
Early intervention should focus on assessing and addressing tear hyperosmolarity to prevent disease progression and improve patient outcomes.
You Can Also Read Antibody-Drug Conjugates and Their Ocular Effects in Cancer Treatment by OncoDaily.
Risk Factors For Ocular Side Effects of Anti-VEGF Therapy
Patients with pre-existing ocular conditions, such as glaucoma or diabetic retinopathy, are more susceptible to complications like increased intraocular pressure (IOP) and hemorrhage. Older individuals or those with compromised vascular health may also experience higher rates of side effects due to decreased resilience of ocular tissues. High cumulative doses of systemic VEGF inhibitors are associated with a greater likelihood of ocular side effects. The concurrent use of other antiangiogenic therapies further elevates the risk, as overlapping mechanisms and increased systemic burden can exacerbate side effects.
What Diagnostic Tools Help Detect Ocular Side Effects of Anti-VEGF Therapy?
Diagnosing ocular adverse events (AEs) induced by anti-VEGF therapy requires a comprehensive approach to differentiate treatment-related complications from other ocular conditions.The first step is obtaining a detailed patient history, focusing on post-injection symptoms such as pain, vision changes, redness, or photophobia. It is also crucial to assess risk factors, including prior ocular conditions, systemic comorbidities (e.g., diabetes, hypertension), and history of multiple injections.
A thorough ophthalmic examination follows, including visual acuity tests to assess vision loss, slit-lamp examination to detect anterior segment inflammation or corneal edema, and fundoscopic evaluation to identify retinal hemorrhages, macular edema, or signs of endophthalmitis. Intraocular pressure (IOP) measurement is also essential to rule out secondary glaucoma.
Imaging techniques, such as optical coherence tomography (OCT), help visualize retinal changes like fluid accumulation, structural disruptions, or signs of inflammation. Fluorescein angiography (FA) can further aid in identifying vascular abnormalities and ruling out alternative causes of vision changes.
A critical aspect of diagnosis is the differential diagnosis, ensuring that symptoms are not due to other conditions such as uveitis, retinal vein occlusion, or diabetic macular edema relapse. Given the potential overlap in symptoms, distinguishing sterile inflammation from infectious complications is essential, often requiring anterior chamber or vitreous fluid analysis in severe cases.
Finally, reporting systems such as the FDA Adverse Event Reporting System (FAERS) play a key role in tracking and analyzing reported side effects, improving early recognition and management of complications associated with anti-VEGF therapy.
Prevention and Management of Ocular Toxicity from VEGF Inhibitors
A comprehensive approach is essential for preventing and managing ocular toxicity associated with VEGF inhibitors. Prevention strategies include conducting a thorough baseline ophthalmologic assessment to identify pre-existing conditions that may increase the risk of toxicity. Regular monitoring through fundoscopy and intraocular pressure (IOP) assessments helps detect complications early. Management strategies focus on symptomatic relief with artificial tears and ocular lubricants to address dry eye symptoms commonly seen with anti-VEGF therapy. In cases of severe toxicity, dose modifications or treatment breaks may be necessary to minimize further risk.
Optimizing Anti-VEGF Therapy: Ophthalmologist-Oncologist Collaboration
Collaboration between ophthalmologists and oncologists is crucial for the prevention and management of anti-VEGF-induced ocular adverse events. This multidisciplinary approach ensures that both the systemic treatment plan and ocular health are closely monitored and managed. Ophthalmologists can conduct baseline eye examinations, monitor for early signs of ocular toxicity (e.g., increased intraocular pressure, retinal hemorrhage), and provide timely interventions such as adjusting treatment or recommending ocular therapies.
Oncologists, on the other hand, can assess the impact of VEGF inhibitors on the patient’s overall health and coordinate with ophthalmologists to adjust dosages or consider treatment breaks if ocular adverse events arise. Regular communication between the two specialists helps to optimize treatment outcomes, minimize ocular complications, and ensure the patient’s quality of life is maintained throughout the course of therapy.
Written by Margarita Pozlikyan MD
FAQ
What conditions are treated with VEGF inhibitors?
VEGF inhibitors are used to treat various cancers (e.g., colorectal, lung, and renal cell carcinoma) and eye diseases like age-related macular degeneration (AMD) and diabetic retinopathy by targeting abnormal blood vessel growth.
What are the common side effects of VEGF inhibitors?
Common side effects include hypertension, proteinuria, delayed wound healing, bleeding, and fatigue. Severe complications like nephropathy and cardiovascular issues may also occur.
How do VEGF inhibitors work?
VEGF inhibitors block the activity of vascular endothelial growth factor, preventing the formation of new blood vessels that tumors or diseased tissues rely on for growth and survival
What are the common ocular side effects of anti-VEGF injections?
Common ocular side effects include subconjunctival hemorrhage, vitreous hemorrhage, increased intraocular pressure, inflammation (uveitis), and eye pain. Subconjunctival hemorrhage is reported in nearly 10% of injections, while vitreous hemorrhage is also a frequent occurrence.
How serious are the ocular side effects of anti-VEGF therapy?
While most ocular side effects are mild and temporary, serious complications can occur, such as endophthalmitis (a severe eye infection) and rhegmatogenous retinal detachment, although these are rare. The overall risk of severe complications is low but should be monitored closely.
What symptoms indicate a serious ocular complication after an injection?
Symptoms that may indicate serious complications include sudden vision loss, severe eye pain, increased redness in the eye, or signs of infection such as discharge. Patients experiencing these symptoms should seek immediate medical attention.
How can patients minimize the risk of ocular side effects from anti-VEGF therapy?
Patients can minimize risks by ensuring proper injection technique, adhering to follow-up appointments for monitoring intraocular pressure, and reporting any unusual symptoms promptly. Regular monitoring and communication with healthcare providers are essential for managing potential side effects effectively.
What are the common ocular side effects of Aflibercept?
Common side effects include blood in the white part of the eye (conjunctival hemorrhage), eye pain, blurred vision, increased pressure in the eye, and vitreous detachment (separation of the gel-like substance in the eye).
What are the most common side effects associated with Ranibizumab?
Commonly reported side effects include conjunctival hemorrhage, eye pain, vitreous floaters, and increased intraocular pressure.
What ocular side effects are linked to Bevacizumab?
Similar to other anti-VEGF agents, Bevacizumab may cause eye redness, eye pain, and increased intraocular pressure.