Pancreatic Cancer: Symptoms, Causes, Types, Diagnosis & Treatment
Pancreatic cancer is a malignant disease that originates in the tissues of the pancreas, an organ critical for digestion and blood sugar regulation. It is one of the deadliest forms of cancer, often diagnosed at an advanced stage, which contributes to its poor prognosis. Understanding pancreatic cancer is essential due to its high mortality rate and the difficulty of early detection. This article will explore its symptoms, causes, types, diagnosis, and treatment options, drawing on data from recent studies to provide an overview of current advances in managing this disease.
What Are the Symptoms of Pancreatic Cancer?
Common symptoms of pancreatic cancer include jaundice, abdominal pain, unexplained weight loss, and digestive issues. Jaundice, seen in about 70% of cases, results from a blocked bile duct. Abdominal pain, often radiating to the back, is another frequent symptom. Patients also experience weight loss and digestive problems like nausea or poor appetite. For instance, many patients report unexplained fatigue and weight loss, which are common early signs. Studies show that 60-80% of patients present with these symptoms, underscoring their prevalence in pancreatic cancer.
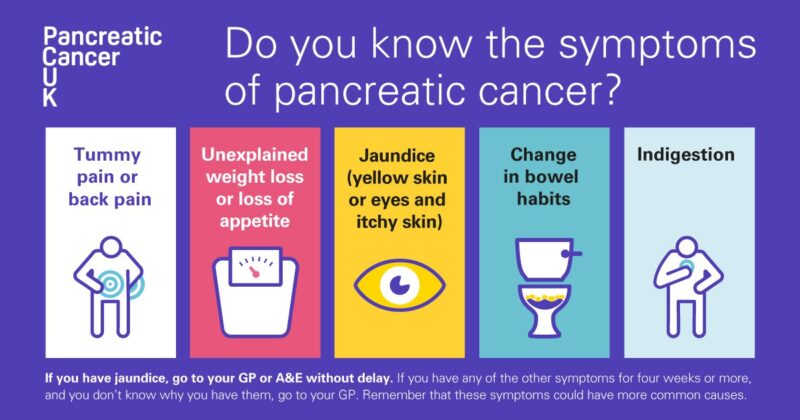
What Are the Early Signs of Pancreatic Cancer?
Initial symptoms of pancreatic cancer are often subtle and can be easily overlooked. These may include mild digestive discomfort, such as bloating, nausea, or changes in stool, as well as back pain that can seem unrelated. Patients may also experience vague abdominal discomfort or a sense of fullness. Because these symptoms are common to less serious conditions, they often delay diagnosis. Early detection is crucial, as pancreatic cancer is more treatable in its early stages. Recognizing these early warning signs, even if they seem minor, is key to improving survival outcomes.
What Are the Causes and Risk Factors for Pancreatic Cancer?
The risk factors for pancreatic cancer are influenced by both genetic predisposition and environmental factors. Research from Siegel et al., 2023, highlights that family history and inherited mutations, such as BRCA1/BRCA2, are significant genetic contributors to the disease. Lifestyle factors also play a pivotal role; smoking, according to a 2021 study by Ilic and Ilic, doubles to triples the risk of pancreatic cancer, accounting for approximately 20-30% of cases. Additionally, chronic pancreatitis, obesity, type 2 diabetes, and poor dietary habits, particularly a high-fat diet, are strongly associated with increased risk.
Genetic Factors and Family History
Genetic factors significantly influence pancreatic cancer risk, with mutations in genes like BRCA1, BRCA2, and PALB2 being among the most recognized contributors. A study by Hu et al., 2020, found that individuals with BRCA2 mutations had a 3 to 10-fold increased risk of developing pancreatic cancer compared to those without the mutation. Additionally, hereditary pancreatitis, linked to PRSS1 gene mutations, also elevates risk.
Family history plays a critical role in risk assessment. Research by Klein et al., 2021, revealed that individuals with two or more first-degree relatives diagnosed with pancreatic cancer had a 6.4-fold increased risk. Furthermore, mutations like PALB2 or STK11 (associated with Peutz-Jeghers syndrome) add to the risk. Genetic counseling and testing for high-risk families can guide personalized prevention and screening strategies, improving early detection and potentially improving outcomes.
Lifestyle and Environmental Risk Factors
Lifestyle factors such as smoking, alcohol consumption, and diet play a significant role in the development of pancreatic cancer. Smoking has long been recognized as a major risk factor, with studies showing that smokers are two to three times more likely to develop pancreatic cancer compared to non-smokers. Heavy alcohol consumption can lead to chronic pancreatitis, which in turn increases the risk of pancreatic cancer by 1.5 to 2 times. Diets high in processed meats, saturated fats, and low in fruits and vegetables also contribute to an elevated risk of developing this disease. Obesity, particularly abdominal obesity, has been linked to a higher incidence of pancreatic cancer.
Environmental factors are also critical contributors. Long-term exposure to certain chemicals, such as pesticides and petroleum products, has been associated with an increased risk of pancreatic cancer. Workers in industries with frequent chemical exposure may face a higher likelihood of developing the disease, emphasizing the importance of protective measures and minimizing exposure to harmful substances. These lifestyle and environmental factors highlight the need for preventive strategies, including smoking cessation, moderation in alcohol consumption, and adopting a healthier diet to reduce the overall risk of pancreatic cancer.
What Are the Types of Pancreatic Cancer?
Pancreatic cancer is classified into two main types: Exocrine Pancreatic Cancer and Pancreatic Neuroendocrine Tumors (PNETs). Exocrine pancreatic cancer, which includes pancreatic adenocarcinoma, is the most common type, accounting for over 90% of cases. It typically presents with symptoms like jaundice, weight loss, and abdominal pain. Treatment often involves surgery, chemotherapy, and radiation.
Pancreatic Neuroendocrine Tumors (PNETs) are less common, making up about 5-10% of pancreatic cancers. These tumors arise from hormone-producing cells and can present with hormonal symptoms, such as diarrhea or blood sugar issues. Treatment options for PNETs include surgery, targeted therapies, and hormone therapy.
Exocrine Pancreatic Cancer
Exocrine pancreatic cancer is the most prevalent type of pancreatic cancer, typically arising from the exocrine glands, with pancreatic ductal adenocarcinoma being the most common subtype. Symptoms often include jaundice, abdominal or back pain, unexplained weight loss, and digestive issues such as loss of appetite and fatty stools. Genetic mutations (such as KRAS, BRCA2, and TP53), lifestyle factors like smoking and obesity, and a family history of pancreatic or related cancers are recognized risk factors.
Treatment for exocrine pancreatic cancer varies based on the stage at diagnosis. Options include surgery (e.g., Whipple procedure), chemotherapy (such as Gemcitabine or FOLFIRINOX), and radiation therapy. While early-stage cases with localized tumors have a better prognosis, often benefiting from surgery and adjuvant therapy, survival rates remain low for most patients due to late-stage diagnosis. According to the 2024 NCCN guidelines, the 5-year survival rate for pancreatic cancer is less than 10%, with localized cases having a survival rate of up to 30%. Advanced-stage patients typically experience a median survival of less than a year, although regimens like FOLFIRINOX can extend survival by several months.
Pancreatic Neuroendocrine Tumors (PNETs)
Pancreatic neuroendocrine tumors (PNETs) are a rarer subtype of pancreatic cancer, accounting for approximately 5-10% of all pancreatic tumors. PNETs are divided into functioning and non-functioning types. Functioning PNETs produce hormones like insulin or gastrin, leading to symptoms associated with hormone overproduction, such as hypoglycemia or ulcers. Non-functioning PNETs, which do not produce active hormones, are often diagnosed at more advanced stages due to their vague symptoms like abdominal pain or unexplained weight loss.
Treatment options for PNETs depend on the stage and type of the tumor. Localized disease is typically treated with surgical resection, while advanced cases may require chemotherapy, targeted therapies (e.g., everolimus, sunitinib), or somatostatin analogs to manage hormone production in functioning tumors. According to the 2024 NCCN guidelines, 5-year survival rates for localized PNETs are significantly better compared to metastatic cases, with survival rates ranging from 50% to 60% for localized tumors, but dropping to approximately 20% for metastatic disease .
How Is Pancreatic Cancer Diagnosed?
Diagnostic procedures for pancreatic cancer typically include imaging tests such as CT scans, MRI, and PET scans to visualize the tumor and assess its spread. These imaging methods are crucial for determining the stage of the cancer and planning treatment options. Additionally, a biopsy is often performed to confirm the diagnosis by extracting a small sample of the tumor for examination. Tumor marker tests, such as measuring CA 19-9 levels, can also aid in diagnosis, although they are more useful for monitoring treatment response than for early detection. Accurate diagnosis is vital for effective treatment planning, with imaging and biopsy accuracy rates generally exceeding 90% in detecting pancreatic cancer.
Imaging and Lab Tests for Pancreatic Cancer
Diagnostic tools for pancreatic cancer include a range of imaging and laboratory tests aimed at detecting and staging the disease early and accurately. CT scans are widely used for identifying the tumor location and assessing its operability, with an accuracy rate of 85-90%. MRI offers more detailed imaging of soft tissues, often employed when CT results are unclear. Additionally, PET scans help detect metastatic disease by identifying areas of increased glucose metabolism, particularly in combination with CT scans.
For laboratory tests, CA 19-9, a tumor marker, plays an essential role in both diagnosis and monitoring treatment. Elevated CA 19-9 levels are detected in 70-90% of patients with pancreatic cancer, particularly in advanced cases. However, false positives can occur in non-cancerous conditions like cholangitis or pancreatitis. Therefore, its effectiveness is enhanced when combined with imaging results. Biopsy methods, particularly endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA), achieve high diagnostic accuracy, especially when integrated with imaging findings, offering accuracy rates close to 90-95% for detecting pancreatic cancer.
These combined diagnostic approaches ensure comprehensive detection and staging, crucial for guiding effective treatment strategies
What Are the Treatment Options for Pancreatic Cancer?
Pancreatic cancer treatment options vary depending on the stage and individual patient factors, with a combination of surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy often utilized. Surgery is the primary curative option for early-stage, resectable tumors, while chemotherapy (e.g., FOLFIRINOX or gemcitabine) is commonly used in both early and advanced stages to slow disease progression. Radiation therapy may be applied to shrink tumors or relieve symptoms, often in conjunction with other therapies. Newer approaches like targeted therapies (e.g., PARP inhibitors for BRCA-mutated tumors) and immunotherapy are increasingly used, particularly for advanced or genetically driven cases. Palliative care focuses on improving quality of life by managing pain and other symptoms throughout the treatment journey.
Surgery for Pancreatic Cancer
The Whipple procedure, distal pancreatectomy, and total pancreatectomy are the primary surgical options for pancreatic cancer. Each of these surgeries is chosen based on the tumor’s location and extent. The Whipple procedure, or pancreaticoduodenectomy, is most often used for tumors in the head of the pancreas. It involves the removal of the head of the pancreas, part of the stomach, duodenum, and other surrounding structures. According to the 2024 NCCN guidelines, an R0 resection, meaning no cancer cells are left at the margins, is crucial for long-term survival .
A distal pancreatectomy is typically used for cancers in the body or tail of the pancreas. It may involve the removal of the spleen. This surgery is more challenging due to the advanced stage at which cancers in this location are often diagnosed. Laparoscopic distal pancreatectomy is increasingly common, reducing hospital stay and recovery time while maintaining similar oncologic outcomes .
Total pancreatectomy, where the entire pancreas and surrounding organs are removed, is rare and reserved for cases with diffuse involvement. Postoperative recovery from these surgeries can be extensive, often requiring enzyme replacement and management of diabetes. The survival rates and outcomes vary, but achieving a complete resection is associated with the best prognosis .
Chemotherapy for Pancreatic Cancer
Chemotherapy regimens such as FOLFIRINOX and gemcitabine are among the primary treatments for advanced pancreatic cancer.
FOLFIRINOX, a combination of 5-fluorouracil (5-FU), leucovorin, irinotecan, and oxaliplatin, is recommended as first-line therapy for patients with good performance status (PS), typically ECOG 0–1. According to the 2024 NCCN Guidelines, FOLFIRINOX has demonstrated superior outcomes in both overall survival (OS) and progression-free survival (PFS) when compared to gemcitabine monotherapy. In a clinical trial, FOLFIRINOX achieved a median OS of 11.1 months and a PFS of 6.4 months, significantly outperforming gemcitabine’s 6.8 months OS and 3.3 months PFS. However, FOLFIRINOX can lead to higher rates of severe side effects, such as neutropenia (45.7%), diarrhea (12.7%), and sensory neuropathy (9%), necessitating careful patient selection based on their ability to tolerate these toxicities .
Gemcitabine is another key chemotherapy option, often combined with other agents like nab-paclitaxel to improve efficacy. Gemcitabine-based regimens are frequently used in patients with intermediate PS or in cases where FOLFIRINOX is not suitable due to toxicity concerns. Although gemcitabine monotherapy has a lower efficacy compared to FOLFIRINOX, with a median OS of 6.8 months, it remains a critical option for patients who cannot tolerate more aggressive treatments. Combinations such as gemcitabine with albumin-bound paclitaxel have shown improved outcomes, with OS reaching 8.5 to 12 months in certain trials, albeit with increased toxicity .
You can Read More on Immunotherapy for Pancreatic Cancer: Article by OncoDaily

Radiation Therapy for Pancreatic Cancer
Radiation therapy plays a key role in treating pancreatic cancer, often used alongside surgery or chemotherapy to target remaining cancer cells, reduce tumor size, or manage symptoms in inoperable cases. External beam radiation therapy (EBRT) is the most common form, delivering high-energy rays directly to the tumor. Radiation is typically employed in patients with localized, non-metastatic pancreatic cancer, especially in those where surgery may not be possible or to downsize tumors before surgery.
According to the 2024 NCCN Guidelines, radiation therapy can be used preoperatively (neoadjuvant) to shrink tumors, making them more resectable, or postoperatively (adjuvant) to target residual cancer cells. Studies, such as one published in the Journal of Clinical Oncology (JCO), show that combining radiation therapy with chemotherapy can improve local control of the disease, especially when used with FOLFIRINOX in borderline resectable pancreatic cancer.
While radiation therapy is effective in controlling local tumor growth, it is not without side effects. Common side effects include fatigue, nausea, and skin irritation at the treatment site, as well as more serious complications like gastrointestinal toxicity or bowel perforation in rare cases. Patients have reported varying degrees of these effects, with most finding them manageable under medical supervision.
Success rates vary depending on the tumor stage and treatment combination. Data from studies cited in the NCCN Guidelines indicate that, in combination with chemotherapy, radiation therapy can improve survival rates in selected patients with locally advanced pancreatic cancer. However, it is often more effective for palliative care in inoperable cases, helping to alleviate pain and improve quality of life.
What Are the Stages of Pancreatic Cancer?
Pancreatic cancer is classified into different stages based on tumor size, location, and the extent to which it has spread, which significantly affects treatment options and prognosis.
- Stage I: The cancer is confined to the pancreas and is often considered resectable (able to be surgically removed). Surgery, such as the Whipple procedure, is the primary treatment, followed by adjuvant chemotherapy. According to the 2024 NCCN Guidelines, patients with Stage I pancreatic cancer have a 5-year survival rate of about 34-37% when treated surgically, though prognosis improves with early detection.
- Stage II: Cancer has spread to nearby tissues and possibly lymph nodes but is still localized enough for surgery in some cases. Chemotherapy or radiation therapy may be given before or after surgery. Survival rates decrease slightly, with a 5-year survival rate ranging from 20-30%, as reported in the Journal of Clinical Oncology.
- Stage III: At this stage, the cancer has grown into nearby blood vessels or other structures, making it usually unresectable. Treatment typically involves chemotherapy, such as FOLFIRINOX or gemcitabine, combined with radiation therapy to control the disease. Per the 2024 NCCN Guidelines, the 5-year survival rate for Stage III pancreatic cancer is less than 10%, with most patients experiencing disease progression despite treatment.
- Stage IV: This is the most advanced stage, where cancer has spread to distant organs, such as the liver or lungs. Treatment is focused on managing symptoms and prolonging life through chemotherapy and, in some cases, targeted therapy or palliative care. Survival rates are poor, with less than 3% of patients surviving five years post-diagnosis, as detailed in studies referenced by the NCCN Guidelines.
Pancreatic cancer’s progression is typically rapid, and survival statistics highlight the importance of early detection and aggressive treatment in improving outcomes. However, even with early diagnosis, the aggressive nature of pancreatic cancer makes long-term survival a challenge for many patients.
After Treatment: What to Expect
The post-treatment phase for pancreatic cancer patients involves regular monitoring for recurrence through imaging and tumor marker tests like CA 19-9. Persistent side effects from treatments, such as fatigue, digestive issues, or neuropathy, are common. Patients who have undergone surgery, especially those with partial pancreas or intestine removal, often require enzyme supplements and a specialized diet to manage digestion.
Lifestyle adjustments include a balanced diet, regular exercise, and stress management, with changes such as smaller, more frequent meals and enzyme supplements to support digestion. Long-term follow-up is crucial for monitoring recurrence, while a strong support network and professional guidance are key for improving recovery and quality of life.
How Long Does It Take to Notice and Cure Pancreatic Cancer?
The timeline from noticing symptoms to diagnosis and treatment for pancreatic cancer can vary significantly, often depending on the stage at which the disease is detected. Pancreatic cancer is notorious for presenting vague symptoms that can be mistaken for other gastrointestinal issues, such as jaundice, abdominal pain, weight loss, or digestive problems. Due to these non-specific early symptoms, diagnosis often occurs at a more advanced stage, making early detection challenging.
On average, once more definitive symptoms arise, patients may undergo initial imaging studies like CT scans or MRI, which are instrumental in determining the presence of a tumor. The diagnostic process, including further tests like biopsies or tumor marker evaluations (e.g., CA 19-9 levels), can take a few weeks, with treatment typically commencing shortly after diagnosis. According to the NCCN 2024 guidelines, for resectable cases, surgery is prioritized, while chemotherapy or radiotherapy may follow, depending on the tumor’s characteristics .
This timeline is crucial as early-stage interventions can significantly improve survival rates, though most cases are diagnosed at advanced stages where options become limited.
You can Watch Latest Updates About Pancreatic Cancer Research, shared at ASCO: ASCO highlight series by OncoDaily
Living with Pancreatic Cancer
Managing daily life with pancreatic cancer requires a balance of emotional, physical, and practical strategies. Coping strategies such as mindfulness and relaxation techniques can help reduce stress. Building a strong support system, including family, friends, and healthcare providers, is crucial. Many patients benefit from talking openly about their feelings and joining support groups.
Lifestyle changes such as adjusting to a nutrient-rich diet, eating smaller frequent meals, and staying physically active with light exercises can improve energy and well-being. For example, one patient found that taking short daily walks and focusing on a balanced diet helped her manage treatment side effects and maintain a positive outlook. Engaging with healthcare providers to address symptoms early and getting help with daily tasks can make managing life with pancreatic cancer more manageable.
Can Pancreatic Cancer Be Prevented?
Preventive measures for pancreatic cancer focus on minimizing risk factors and promoting early detection. Regular screenings, particularly for individuals with a family history of pancreatic cancer or genetic predispositions (e.g., BRCA mutations), can help in early detection. Experts recommend screening through endoscopic ultrasound (EUS) or MRI for high-risk individuals.
Lifestyle changes, such as quitting smoking, reducing alcohol consumption, maintaining a healthy weight, and managing chronic conditions like diabetes, significantly lower the risk. A diet rich in fruits, vegetables, and whole grains, while limiting processed foods and red meats, is recommended. Research shows that individuals who follow a healthy diet and lifestyle have up to a 30% reduced risk of developing pancreatic cancer.
Expert advice suggests that while there is no guaranteed prevention, these measures can reduce risk and improve overall health, offering a better chance for early detection and more effective treatment outcomes.
Regular Screenings for Pancreatic Cancer
Regular screenings for pancreatic cancer are crucial for early detection, especially for individuals at high risk, such as those with a family history of the disease or genetic mutations like BRCA or PALB2. Early detection significantly improves survival rates, as pancreatic cancer is often diagnosed at an advanced stage when symptoms appear late.
According to the NCCN Guidelines, patients diagnosed at an early stage have a 5-year survival rate of about 37%, compared to 3% for those diagnosed at a more advanced stage. Screening methods, such as endoscopic ultrasound (EUS) and MRI, are commonly recommended for high-risk groups and can detect early, localized tumors, offering the best chance for successful treatment, including surgical resection. Early intervention through screening can be life-saving, emphasizing its critical role in improving patient outcomes.
Lifestyle and Dietary Changes
Lifestyle and dietary changes can significantly reduce the risk of pancreatic cancer. Quitting smoking is one of the most impactful steps, as research shows that smoking is a major risk factor, accounting for about 20-30% of pancreatic cancer cases. Studies indicate that stopping smoking can reduce risk by up to 50% after a decade of cessation.
Maintaining a healthy weight and staying physically active also contribute to lowering pancreatic cancer risk. Obesity has been linked to an increased likelihood of developing pancreatic cancer, and studies suggest that regular exercise and weight management can reduce this risk.
Dietary changes include eating more fruits, vegetables, and whole grains, while reducing consumption of red and processed meats, which have been associated with a higher risk of pancreatic cancer. Research published in the Journal of the National Cancer Institute found that diets high in fruits, vegetables, and fiber reduced cancer risk by up to 30%.
Incorporating these lifestyle changes can significantly decrease the likelihood of developing pancreatic cancer, improving overall health and potentially preventing the disease.
FAQ
What is the success rate of pancreatic cancer treatments?
The success rate depends on the stage of the cancer at diagnosis. Early-stage pancreatic cancer has a 5-year survival rate of around 20%, while for advanced-stage cancer, this rate drops to below 10%. Success rates improve with early detection and advanced treatments like FOLFIRINOX and targeted therapies.
Are there any novel treatments for pancreatic cancer?
Yes, novel agents such as PARP inhibitors, immunotherapy, and targeted therapies are being explored in clinical trials. These treatments aim to target specific genetic mutations or enhance the body’s immune response to pancreatic cancer.
What are the common side effects of chemotherapy for pancreatic cancer?
Common side effects include nausea, fatigue, hair loss, and increased risk of infection. FOLFIRINOX, for example, is more aggressive and may lead to severe side effects like neuropathy and diarrhea, while gemcitabine tends to be less toxic.
How effective is surgery in treating pancreatic cancer?
Surgery, such as the Whipple procedure, can be highly effective for early-stage pancreatic cancer. It offers the potential for a cure when the cancer is localized, but surgery is only an option for about 20% of patients due to late-stage diagnosis.
What role does radiation therapy play in treating pancreatic cancer?
Radiation therapy is often used in combination with surgery or chemotherapy to shrink tumors or manage symptoms. It can help reduce pain and improve survival rates, especially when paired with other treatments.
How do clinical trials contribute to pancreatic cancer treatment advancements?
Clinical trials are essential for testing new treatments, including novel agents like PARP inhibitors or immunotherapies. These trials provide valuable insights into the efficacy and safety of new therapies and offer patients access to cutting-edge treatments.
Are there genetic factors that increase the risk of pancreatic cancer?
Yes, genetic mutations in BRCA1, BRCA2, and PALB2 can increase the risk of developing pancreatic cancer. Individuals with a family history of these mutations may benefit from genetic counseling and early screening.
Can lifestyle changes reduce the risk of pancreatic cancer?
Yes, lifestyle changes like quitting smoking, reducing alcohol consumption, maintaining a healthy weight, and eating a balanced diet rich in fruits and vegetables can help lower the risk of pancreatic cancer.
What is the importance of early detection in pancreatic cancer?
Early detection is crucial, as pancreatic cancer is often diagnosed at an advanced stage. Regular screenings for high-risk individuals and paying attention to symptoms like jaundice or unexplained weight loss can improve survival rates.
What are the long-term side effects of pancreatic cancer treatments?
Long-term side effects vary by treatment but can include chronic fatigue, digestive issues, and neuropathy. Patients often require ongoing care and support to manage these effects and maintain quality of life after treatment.
Written by Toma Oganezova, MD
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
