Manni Mohyuddin, Assistant Professor in the Division of Hematology/Bone Marrow Transplant at the University of Utah Huntsman Cancer Institute, recently shared a thread on X/Twitter:
”A very common consult that hematologists get is for MGUS in the setting of neuropathy. Are they associated? What diagnosis can explain the association? What workup needs to be ordered? In this thread, we do a deep dive on this important topic/outline management.
Firstly, we must recognize that neuropathy is actually very common (28% in those with diabetes, 11% in those without). And MGUS is very common too. So it is almost guaranteed that you will see patients with MGUS and neuropathy. But that doesn’t mean they are related.
And since common things are common, always evaluate and look for common explanations for neuropathy first. Diabetes, Vit B12 deficiency, alcohol etc. Even in someone with MGUS, those causes are far more likely to be the cause of neuropathy.
In order to ascertain whether they are related in the first place, we need a prospectively screened cohort, as retrospective studies may identify associations that are false (people with more healthcare encounters/illnesses are more likely to be diagnosed with neuropathy/MGUS).
The amazing Iceland screens, treats or prevents multiple myeloma (StopMM) is doing that- and I anxiously await their results. Meanwhile, a study of 15,351 pts with MGUS and over 58,000 controls uncovered an association between MGUS and neuropathy. Link to publication.
This same stellar group has already disproved any association between MGUS and osteoporosis (please don’t order labs looking for myeloma for every osteoporosis patient).
So now, having proven that there probably is a legit association between MGUS and neuropathy, but that both are very common- how do we approach these situations? The first thing to know is that the probability of them being related is VERY low.
The first thing to look at is the type of heavy chain involved. Is it IgM or not? IgM plasma cell disorders have a legit association with neuropathy. It is unclear whether non-IgM MGUS (unless it is Amyloidosis or POEMS) truly has any causation with neuropathy.
There are some well-known entities where IgM MGUS can cause neuropathy. Classically, it causes distal, acquired, demyelinating, symmetric neuropathy with M protein (DADS-M), a variant of CIDP. Usually affects older men, mostly sensory. Anti-MAG antibodies in 50% of patients.
EMG can help tremendously in the work-up (obviously a hematologist needs to work with a neurologist for this). What do we see in EMG for IgM-associated neuropathies? Demyelination, slower motor velocities, terminal nerve involvement.
Other than anti-MAG antibodies, any other testing that can be abnormal? Patients with IgM-associated MGUS who do not have Anti-MAG antibody may have anti-ganglioside or anti-asialo-GM1 antibodies- so worth checking them too. Again, these antibodies don’t prove causality but useful.
Very rarely- IgM-associated MGUS can present with some syndromes. An example below: CANOMAD (chronic ataxic neuropathy, ophthalmoplegia, immunoglobulin M [IgM] paraprotein, cold agglutinins, and disialosyl antibodies).
And sometimes an IgM plasma cell dyscrasia is actually Waldenstroms Macroglobulinemia. And that can cause neuropathy too. So be sure to evaluate for that as a diagnostic entity. Remember IgM MGUS is more likely will become Waldenstrom rather than IgM Myeloma (which is very rare).
Treatment for IgM-associated MGUS usually entails a trial of IVIG, and if no response- a trial of rituximab- and if no response, further plasma cell-directed therapies as appropriate. This is obviously not based on high-quality data, but small series and opinions/viewpoints.
Now what if you see findings of CIDP in the setting of a non-IgM MGUS (IgG or IgA)? The reality is that treatments that work for CIDP (IVIG, plasma exchange etc) work similarly well for those patients, and you would treat just as you would treat any other patient with CIDP.
There was actually a NEJM randomized study on this topic all the way back in 1991. For patients with polyneuropathy and MGUS, actual plasma exchange compared to sham exchange seemed to benefit IgG and IgA much more than IgM!
Regardless, plasma exchange is an effective treatment modality for CIDP overall- so in my opinion, whether or not IgG or IgA MGUS is present doesn’t change management, so for all practical purposes- I think of these as coincidental (unless Amyloid or POEMS).
So we have learnt now, that IgM MGUS is definitely related with neuropathy. And that for IgG or IgA MGUS, there is no clear link- unless there is amyloidosis or POEMS. So, you must think of amyloidosis or POEMS for such patients you see in clinic. How do you do that?
AL Amyloidosis is usually a lambda variant. It is extremely rare (although not impossible) to have isolated nerve amyloidosis, so a careful clinical exam is necessary to look for other organ involvement. I look at urinary proteinuria and serum ntPROBNP to evaluate kidneys/heart.
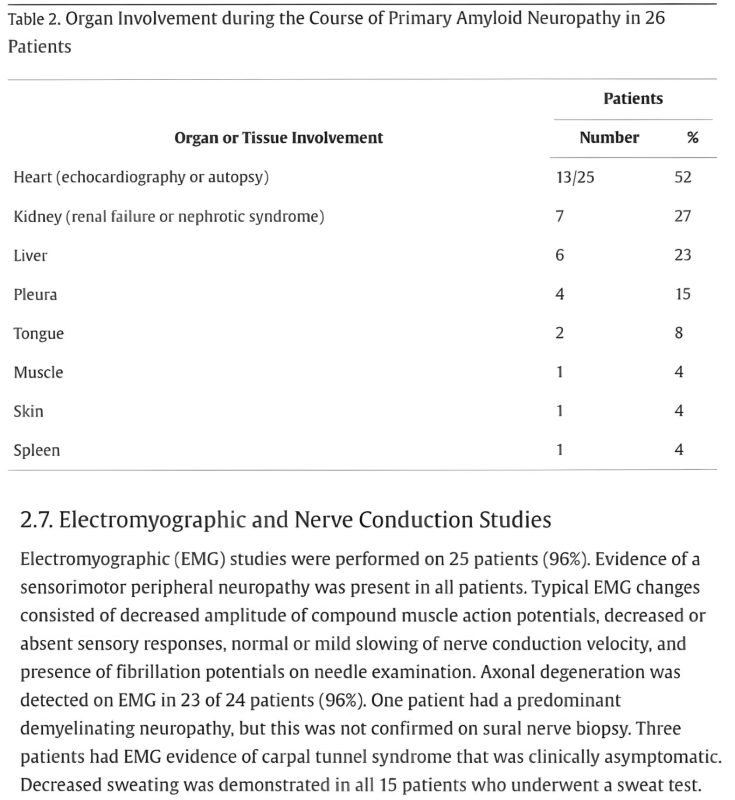
In this report from the Mayo Clinic of 1,282 patients with AL amyloid, 26 had neuropathy as dominant feature, and the majority of those 26 ALSO had other organs involved. EMG findings in the image below- always shows abnormalities.
So if you see a patient with IgG or IgA MGUS who has neuropathy, and no other clinical findings of amyloidosis on exam/initial work-up, it is extremely unlikely that isolated nerve amyloidosis is the cause of neuropathy. Now what about POEMS syndrome?
POEMS (polyneuropathy, organomegaly, endocrinopathy, monoclonal protein, skin changes) is also rare. Almost always lambda light chain. You may not have all the features, but polyneuropathy is universal. A serum VEGF level is useful for diagnosis.
POEMS causes “osteosclerotic” rather than lytic lesions. You can occasionally have it even in absence of a detectable bone marrow clone. If localized, can treat with radiation, but if systemic with plasma cell clone, treat with myeloma therapy (obviously avoid neurotoxic drugs).
In summary: Is there POEMS or amyloidosis? Is it IgM- if yes, consider IgM-related neuropathies, and Waldenstroms as a cause.
If IgG/IgA, very unlikely to be related unless POEMS/amyloidosis. For more reading, this review by Vincent Rajkumar is excellent. END.”
Source: Manni Mohyuddin/Twitter
