Remote Therapeutic Monitoring (RTM) is helping address one of the most challenging parts of cancer care—the time patients spend at home between clinic visits. For many people undergoing treatment, the hardest moments do not happen in the exam room. They happen quietly at home. Fatigue gradually worsens. Nausea becomes harder to control. Appetite fades. Pain increases. Dehydration develops. Early signs of infection appear. When these changes go unnoticed, they can escalate into emergency department visits, hospitalizations, or interruptions in cancer treatment.
Despite major advances in cancer therapies, the period between visits remains one of the most vulnerable times in oncology care. Patients are often left to decide when a symptom is serious enough to report, while clinics rely on phone calls that may come too late—or may not happen at all. This gap is not due to lack of effort from patients or clinicians. It reflects the limitations of traditional oncology workflows.
Remote Therapeutic Monitoring offers a practical way to close this gap. Through structured, daily symptom tracking, RTM allows care teams to detect changes earlier, intervene sooner, and support patients more consistently during treatment. One company focused on making this approach work in everyday oncology practice is Relay RTM.
Why Between-Visit Symptoms Matter
Cancer treatments place continuous stress on the body. Many side effects do not appear suddenly but worsen over time. Fatigue may start as mild tiredness before becoming disabling. Nausea may progress from occasional discomfort to persistent vomiting. Even moderate diarrhea can quickly lead to dehydration, kidney injury, or hospitalization, particularly in older adults.
Many patients hesitate to reach out. Some worry about bothering their care team. Others assume side effects are unavoidable or “normal.” As a result, clinically meaningful symptoms often remain invisible until they reach a crisis point.
Earlier awareness allows earlier action—and that can change outcomes.
The Limits of Traditional Oncology Workflows
Most oncology clinics are built around scheduled visits, not continuous symptom visibility. When patients do call between visits, interactions are often urgent, unstructured, and disruptive to clinic flow. Nursing teams are pulled into reactive triage, important details may be missed, and documentation can be fragmented. This unpredictability contributes to staff burnout and uneven patient experiences.
Historically, proactive symptom management has also been financially unsupported, making it difficult for clinics to scale consistent between-visit care. RTM changes this dynamic by providing a structured, reimbursable framework for symptom monitoring.
What Remote Therapeutic Monitoring Means for Patients
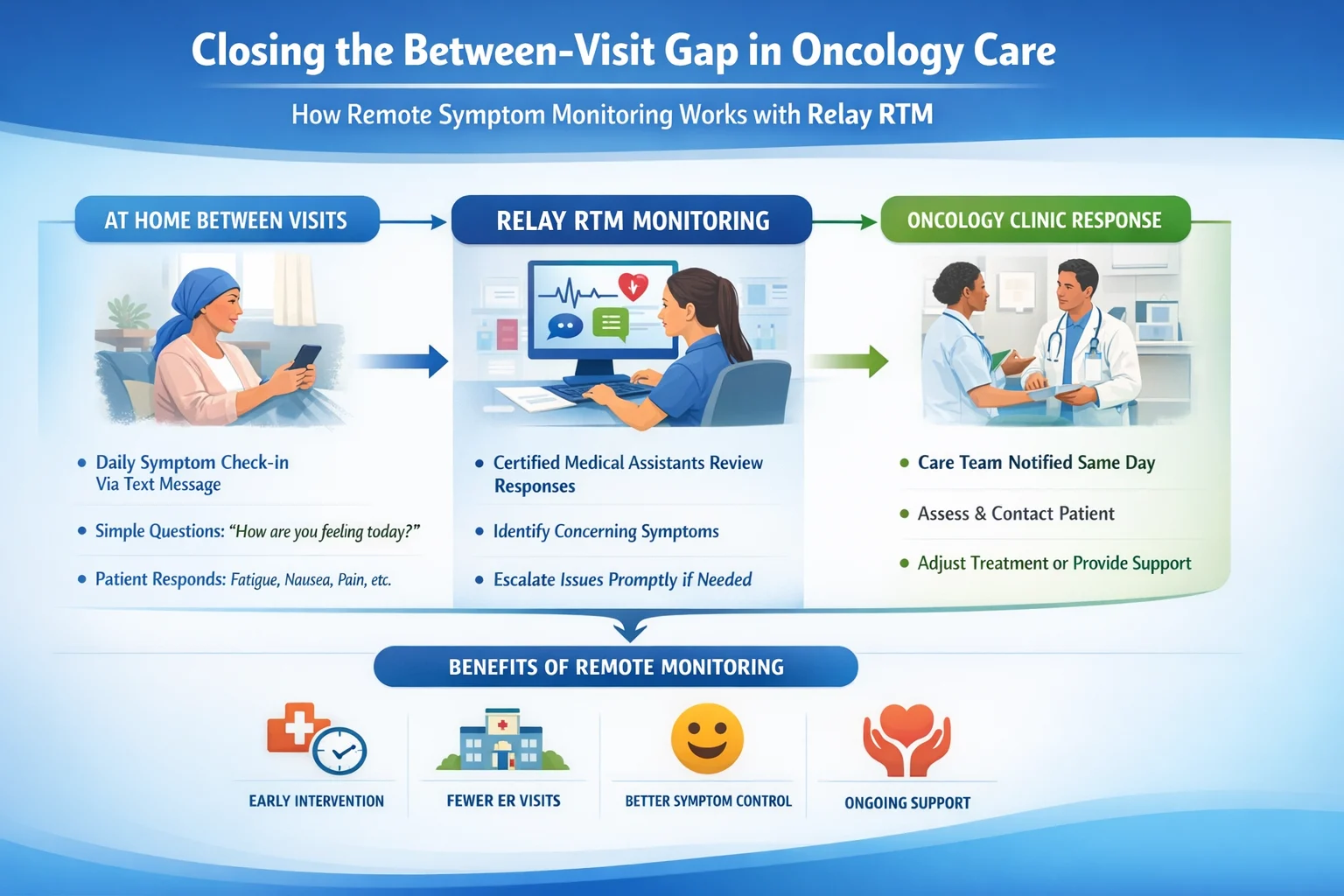
Remote Therapeutic Monitoring allows care teams to track patient symptoms regularly while patients remain at home. Instead of relying on sporadic phone calls, RTM creates a consistent daily check-in.
Relay RTM is designed to be simple. Patients receive brief symptom questions via text message. There is no app to download, no portal to navigate, and no technical setup. This simplicity is critical for patients undergoing treatment, older adults, and those with limited digital experience. Patients respond to short questions covering symptoms such as fatigue, nausea, pain, hydration, appetite, and other treatment-related concerns.
How Relay RTM Works in Daily Oncology Practice
A common concern with remote monitoring is that it may create more work for clinics. Relay RTM was designed to avoid this. Patient responses are reviewed daily by U.S.-based Certified Medical Assistants trained to recognize meaningful symptom trends. Rather than triggering alerts for every minor change, the focus is on identifying patterns that suggest clinical risk.
When concerning trends emerge, they are escalated to the oncology clinic for same-day review. These commonly include:
- Worsening fatigue affecting daily function
- Dehydration risk or reduced oral intake
- Escalating gastrointestinal symptoms
- Early signs of infection
- Increasing or poorly controlled pain
Relay does not make clinical decisions. The oncology care team retains full control over evaluation and treatment. Relay functions as an early-warning layer, ensuring timely and organized communication. Documentation is prepared in a format aligned with RTM billing requirements, reducing administrative burden for clinic staff.
Why Earlier Symptom Detection Improves Outcomes
Catching symptoms early allows problems to be managed before they escalate. Dehydration can often be treated with timely outpatient fluids instead of hospitalization. Infections can be addressed before becoming severe. Pain and nausea can be adjusted before they disrupt daily life or treatment adherence.
Early intervention also helps patients stay on therapy. Many dose reductions or treatment interruptions occur not because treatment fails, but because side effects become unmanageable. Proactive symptom management preserves treatment continuity and quality of life. Clinics using Relay RTM report improved visibility into patient status between visits and fewer urgent disruptions to clinic operations.
Financial Sustainability Without Added Burden
For years, symptom management outside clinic visits has been clinically necessary but financially unsupported. RTM reimbursement changes that reality.
Practices using Relay RTM typically generate around $150 per patient per month under existing RTM billing codes. This allows symptom monitoring to be supported as part of routine care rather than absorbed as unpaid work. Importantly, reimbursement supports care delivery—it does not replace clinical judgment or patient-centered decision-making.
Real-World Engagement and Performance
Relay RTM is already in routine clinical use. Across participating clinics:
- Patient response rates average 81%
- 96% of patients meet RTM billable thresholds
- About three clinically meaningful symptom escalations per patient per month are identified and reviewed
These escalations frequently lead to outpatient interventions that prevent symptom progression and reduce emergency department visits. Clinics also report more predictable triage workflows and improved staff efficiency.

What This Means for Patients
Between visits, many patients feel uncertain and alone. They may wonder whether symptoms matter or whether it is worth calling the clinic. Relay RTM provides reassurance that symptoms are being monitored regularly. Patients know that changes are reviewed and shared with their care team when needed. This reduces anxiety and helps patients feel supported throughout treatment, not just during appointments.
As one patient shared:
“It really takes a load off my shoulders knowing someone is checking in regularly.”
A Shift Toward Proactive, Patient-Centered Oncology Care
Modern oncology care is no longer focused solely on treating tumors. It also aims to preserve quality of life, prevent avoidable complications, and support patients throughout the treatment journey. Between-visit symptom monitoring is central to this shift. When symptoms are identified early, outcomes improve, clinic workflows stabilize, and patients feel more supported.
Relay RTM demonstrates that proactive symptom monitoring can be implemented at scale without increasing clinical burden. By combining simple patient communication, daily clinical review, and aligned reimbursement, it transforms symptom management from a reactive process into a sustainable model of care.
Looking Ahead
The future of oncology care will not be defined only by new drugs. It will also be shaped by better communication, earlier intervention, and continuous support.
Remote Therapeutic Monitoring is rapidly becoming foundational to modern oncology practice. Relay RTM shows how structured, human-reviewed monitoring can close the between-visit gap—improving care during the moments when patients need it most.