Ben Sasse, the former U.S. Senator from Nebraska (2015-2023) and short-term president of the University of Florida (2023-2024), revealed his stage 4 pancreatic cancer diagnosis on December 23, 2025, via a deeply personal X post. At 53 years old, Sasse delivered a raw, unfiltered message blending stark acceptance of his prognosis with unwavering faith, family devotion, and resolve to fight—capturing national attention amid his recent family health trials.

Photo by Gage Skidmore via Wikimedia
In his viral X post, Sasse wrote: “Last week I was diagnosed with metastasized, stage-four pancreatic cancer, and am gonna die.” He framed it bluntly as a “death sentence,” acknowledging the disease’s notoriety for late detection and dismal outcomes, yet pivoted to gratitude:
“I’ve got less time than I’d prefer… but God has been good.”
Sasse emphasized his roles as husband and father, noting pain for his wife Melissa (recently battling epilepsy, prompting his UF exit) and three children. He vowed, “We’re gonna fight,” while pointing to eternal hope in Christ, stating his faith provides “real hope beyond the grave.” The post’s authenticity eschewing political spin sparked prayers, shares, and media coverage from ABC News to Fox.
Sasse’s Background: From Policy Leader to Personal Crisis
Born on February 22, 1972, in Plainview, Nebraska, Ben Sasse grew up in a rural, working-class family, instilling his lifelong emphasis on self-reliance, community, and traditional values. He excelled academically, earning a bachelor’s degree in American history from Harvard University (1994), followed by an MA and PhD from Yale University (2004), where his dissertation explored populism and political rhetoric.
Early in his career, Sasse honed analytical skills at the Boston Consulting Group (1994-1995) and McKinsey & Company (1995-2005), advising Fortune 500 firms on strategy. He then entered public service during the George W. Bush administration, serving as Assistant Secretary for Planning and Evaluation at the U.S. Department of Health and Human Services (2007-2009), overseeing policy on healthcare, welfare reform, and data-driven initiatives amid the financial crisis.
As president of Midland University in Fremont, Nebraska (2010-2014), Sasse orchestrated a dramatic turnaround: enrollment surged 69%, finances stabilized from deficits to surpluses, and innovative programs like competency-based education positioned it as a national model for small liberal arts colleges.
Ben Sasse’s Senate Career and Conservative Intellectualism
Elected to the U.S. Senate in 2014 as Nebraska’s junior senator, Sasse positioned himself as a principled conservative thinker, authoring bestsellers like The Vanishing American Adult (2017), critiquing cultural decay and advocating civic education, and Them: Why Most People Are Rationally Ignorant (2018), dissecting political tribalism.
Key legislative pushes included entitlement reform (Social Security/Medicare sustainability), Big Tech antitrust measures, and family policy enhancements. A never-Trumper, he condemned the January 6 riot, skipped Trump’s 2020 inauguration, and opposed election challenges drawing primary ire but earning bipartisan respect.
Ben Sasse’s Academic Leadership and Recent Family Trials
In January 2023, Sasse resigned from the Senate to become the 13th president of the University of Florida, the first non-alum in decades, focusing on “practical, high-impact education,” research commercialization, and affordability amid culture wars. His 18-month tenure boosted rankings and partnerships but ended abruptly in July 2024 to care for his wife, Melissa, battling severe epilepsy requiring full-time support.
This family-first decision prioritizing their three children (ages 12-18 at diagnosis) mirrors his writings and now faces ultimate test with his stage 4 pancreatic cancer revelation, transforming policy leader into mortality’s stark personal confrontation.
You Can Also Read Rudy Giuliani and Prostate Cancer: How He Went Against, How He Survived, and More by OncoDaily
Why Pancreatic Cancer Is Usually Found Too Late
Pancreatic cancer remains one of the most challenging malignancies to diagnose early, a reality consistently acknowledged by major oncology authorities including the National Comprehensive Cancer Network (NCCN), the American Society of Clinical Oncology (ASCO), and the U.S. National Cancer Institute (NCI). Across guidelines and population-level data, a central and sobering conclusion emerges: most pancreatic cancers are diagnosed at an advanced stage, when curative treatment is no longer feasible.
According to population-based data from the SEER Program, which underpins much of the evidence cited by NCCN and ASCO, only about 13% of pancreatic cancers are diagnosed at a localized stage, when the tumor is confined to the pancreas. Approximately 29% are identified with regional spread to nearby lymph nodes or structures, while nearly half around 45–50% are diagnosed with distant metastatic disease at presentation. This distribution has remained largely unchanged over the past two decades, despite advances in imaging and oncology care.
NCCN guidelines emphasize that this late-stage presentation is not due to delays in care alone, but rather to the biological and anatomical characteristics of pancreatic cancer itself. Early-stage disease is often clinically silent, producing vague or nonspecific symptoms—such as mild abdominal discomfort, fatigue, or weight loss—that are easily attributed to benign conditions. Jaundice, persistent pain, or bowel changes typically appear only once the disease has progressed beyond the pancreas.
ASCO clinical guidance further highlights that there is currently no effective population-wide screening strategy for pancreatic cancer. Unlike breast, colorectal, or cervical cancer, no screening modality has demonstrated sufficient sensitivity and specificity to detect early pancreatic tumors in asymptomatic individuals at average risk. As a result, most diagnoses occur only after symptoms prompt diagnostic imaging.
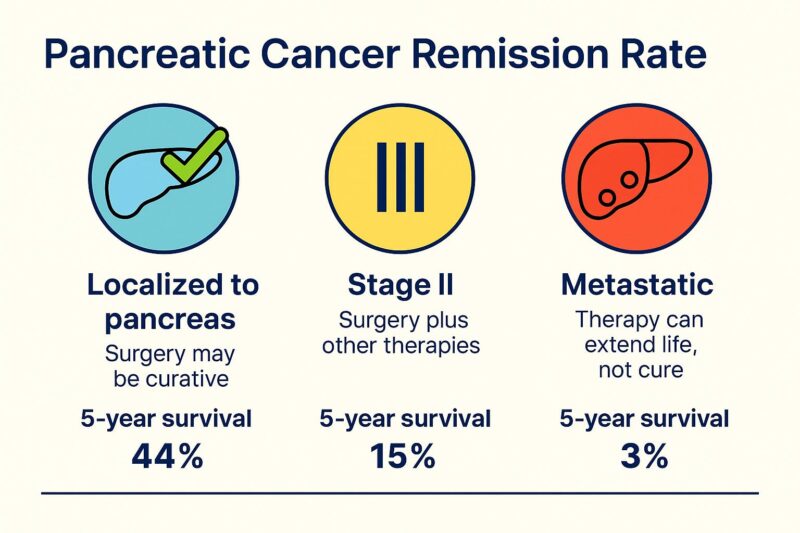
The consequences of this late detection are reflected directly in survival outcomes. SEER-based survival analyses, frequently cited by ASCO and the American Cancer Society, show that patients diagnosed with localized pancreatic cancer have a 5-year relative survival of approximately 45–50%, whereas those with regional disease have survival closer to 15–20%. For patients diagnosed with metastatic pancreatic cancer, 5-year survival drops dramatically to around 3%. When all stages are combined, overall 5-year survival remains in the range of 12–13%, making pancreatic cancer one of the deadliest solid tumors in oncology.
Importantly, even among patients who appear to have early-stage disease, NCCN and NCI stress that pancreatic cancer is frequently biologically aggressive and micrometastatic at diagnosis. This explains why recurrence rates remain high even after technically successful surgical resection and why long-term survival gains have been incremental rather than transformative.
Both NCCN and ASCO therefore underscore the urgent need for progress in early detection, including biomarker development, high-risk surveillance strategies, and improved imaging approaches for selected populations such as those with hereditary cancer syndromes, strong family history, or new-onset diabetes after age 50. Until such tools are validated, pancreatic cancer will continue to be diagnosed predominantly at advanced stages, with profound implications for patient outcomes.
Pancreatic Cancer Treatment by Stage and the Role of Molecular Testing (NCCN-Aligned)
Treatment of pancreatic cancer is primarily determined by stage at diagnosis, with markedly different strategies for resectable, locally advanced, and metastatic disease. According to the NCCN Clinical Practice Guidelines in Oncology for Pancreatic Adenocarcinoma, optimal care requires a multidisciplinary approach integrating surgery, systemic therapy, and increasingly, molecular profiling.
Resectable and Borderline Resectable Disease
For patients with resectable or borderline resectable pancreatic cancer, surgical resection with curative intent is the cornerstone of treatment. Depending on tumor location, this includes pancreaticoduodenectomy (Whipple procedure) or distal pancreatectomy. Surgery alone is insufficient; adjuvant chemotherapy significantly improves survival.
Current NCCN and ASCO-supported evidence identifies modified FOLFIRINOX as the preferred adjuvant regimen for fit patients, with gemcitabine-based combinations reserved for those unable to tolerate intensive therapy. Radiation therapy may be considered selectively, particularly in borderline resectable disease or clinical trial settings.
Locally Advanced (Unresectable) Disease
In locally advanced pancreatic cancer without distant metastases, systemic chemotherapy is the primary treatment. Regimens such as FOLFIRINOX or gemcitabine plus nab-paclitaxel are used to control disease, prolong survival, and in some cases downstage tumors to allow later surgical resection. Treatment decisions are individualized based on performance status and response.
Metastatic Disease
For metastatic pancreatic cancer, treatment is palliative and centered on combination chemotherapy, most commonly FOLFIRINOX or gemcitabine/nab-paclitaxel. These regimens offer meaningful survival benefits compared with older single-agent approaches, while supportive care remains essential for symptom control and quality of life.
Molecular and Genetic Testing: A New Standard of Care
NCCN guidelines now recommend universal germline genetic testing for all patients diagnosed with pancreatic cancer, regardless of family history. Germline mutations in genes such as BRCA1, BRCA2, PALB2, and ATM influence treatment selection, inform family risk assessment, and may predict sensitivity to platinum-based chemotherapy or PARP inhibitors.
In patients with locally advanced, recurrent, or metastatic disease, tumor molecular profiling using next-generation sequencing is strongly recommended. Somatic testing can identify actionable alterations, assess mismatch repair or microsatellite instability status, and guide targeted therapy or clinical trial enrollment. Although actionable mutations are uncommon, their identification can significantly alter management in selected patients.
Together, NCCN and ASCO guidance emphasizes that outcomes in pancreatic cancer improve when early surgical intervention, effective systemic therapy, and molecularly informed treatment decisions are integrated. While imaging remains essential for staging and resectability assessment, genetic and genomic testing now play a central role in modern pancreatic cancer care, marking a shift toward precision oncology even in this historically treatment-resistant disease.
You Can Also Read About Pancreatic Cancer Remission Rate by OncoDaily

Written by Aharon Tsaturyan, MD, Editor at OncoDaily Intelligence Unit
FAQ
What type of cancer was Ben Sasse diagnosed with?
Former U.S. Senator Ben Sasse was diagnosed with stage IV pancreatic cancer, meaning the disease had already spread beyond the pancreas at the time of diagnosis.
When did Ben Sasse announce his pancreatic cancer diagnosis?
Ben Sasse publicly announced his diagnosis on December 23, 2025, sharing the news in a personal post that emphasized faith, family, and acceptance while acknowledging the seriousness of metastatic pancreatic cancer.
What does stage IV pancreatic cancer mean?
Stage IV pancreatic cancer indicates metastatic disease, where cancer cells have spread to distant organs such as the liver, lungs, or peritoneum. At this stage, treatment is not curative and focuses on prolonging survival and maintaining quality of life.
What is the survival rate for stage IV pancreatic cancer?
According to data cited by NCCN, ASCO, and SEER, the 5-year survival rate for stage IV pancreatic cancer is approximately 3–5%, making it one of the deadliest cancers due to late diagnosis and aggressive biology.
Why is pancreatic cancer usually diagnosed at a late stage?
Pancreatic cancer often causes no specific symptoms in its early stages and lacks an effective screening test for the general population. As a result, nearly half of all patients are diagnosed at stage IV, when treatment options are limited.


