Access to vital preventive health services, including life-saving annual mammograms, could be severely restricted for millions of Americans depending on a pending Supreme Court decision. A legal challenge to the Affordable Care Act’s (ACA) mandate requiring insurers to cover these services without cost-sharing has reached the nation’s highest court, putting crucial early detection tools for diseases like breast cancer at risk. With over 150 million Americans currently relying on this no-cost coverage, and hundreds of thousands facing breast cancer diagnoses each year, the stakes are incredibly high.
What’s at Risk? Supreme Court Case Could End Free Mammograms
The legal battle centers on the case of Braidwood Management Inc. et al v. Xavier Becerra et al. This lawsuit challenges the ACA provision that mandates health insurers cover preventive services recommended by the U.S. Preventive Services Task Force (USPSTF) and other expert bodies without requiring patients to pay deductibles, copays, or coinsurance.
The case began in 2020 when Christian business owners and individuals argued that being required to cover certain preventive services, like pre-exposure prophylaxis (PrEP) for HIV, violated their religious freedoms. Additionally, the plaintiffs contend that the way members of the USPSTF and similar advisory bodies were appointed is unconstitutional under the Appointments Clause.
In March 2023, a Texas district court initially ruled that some preventive services might not require full insurance coverage, potentially limiting access. While this ruling was largely paused during the appeals process, the Fifth Circuit Appeals Court upheld the decision in June 2024, though its immediate effect was limited mainly to the specific parties involved in the lawsuit. The case has now advanced to the Supreme Court, with oral arguments anticipated in April 2025 and a final ruling likely by June 2025. A decision against the ACA mandate could have nationwide implications.
How Mammography Coverage Works Now?
The ACA’s preventive services mandate has been a cornerstone of increased access to critical screenings. Specifically, it requires full coverage for:
- Annual screening mammograms for women aged 40 and older.
- Risk-reducing medications for women at high risk for breast cancer.
- Genetic services for individuals with a relevant family history of cancer.
Organizations like Susan G. Komen, a leading breast cancer advocacy group, have strongly opposed the challenge to this mandate. Komen recently filed an amicus brief with the Supreme Court, arguing that the ACA’s no-cost preventive care provision has been essential in improving access to care, reducing treatment costs, and ultimately saving lives through earlier detection.
Early detection significantly improves outcomes for breast cancer. Finding cancer at an earlier, more treatable stage often means less aggressive treatment is needed, leading to higher survival rates and a better quality of life. Removing financial barriers through no-cost screening encourages more people to get tested. Komen estimates that over 150 million Americans currently benefit from these preventive services, which are now under threat.
Understanding Breast Cancer and the Power of Screening
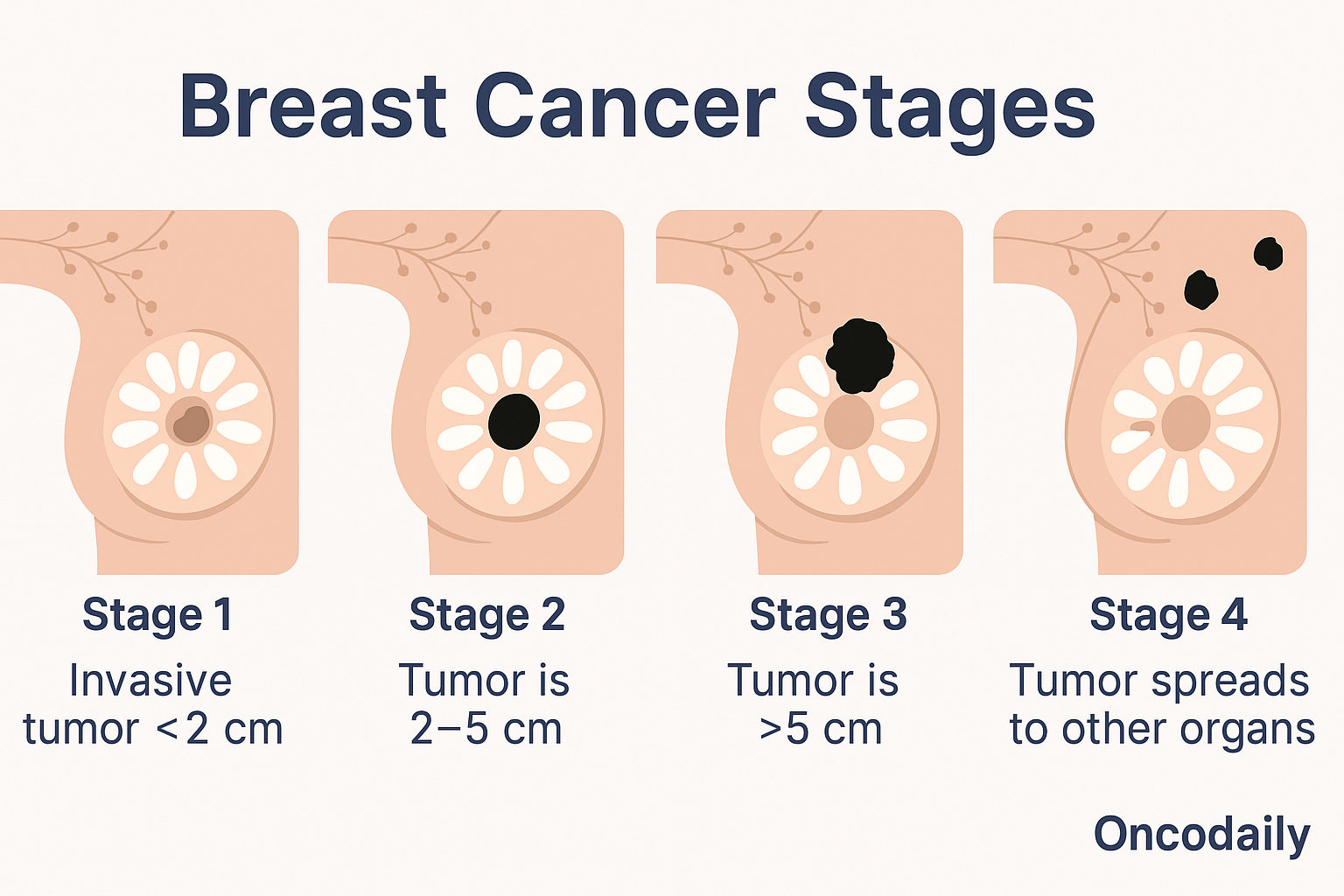
Breast cancer stands as the second leading cause of cancer death among women, surpassed only by lung cancer, with approximately a 1 in 43 lifetime risk of dying from the disease. It occurs when cells in the breast grow uncontrollably, forming tumors that can spread.
Read More About Breast Cancer Symptoms, diagnosis and treatment on OncoDail.
According to the American Cancer Society’s estimates for 2025, there will be around 316,950 new cases of invasive breast cancer diagnosed in women, plus about 59,080 cases of non-invasive ductal carcinoma in situ (DCIS). Sadly, an estimated 42,170 women are projected to die from the disease in 2025. While the median age of diagnosis is 62, breast cancer can and does affect younger women.
Encouragingly, breast cancer death rates have declined significantly since the late 1980s – a 44% reduction by 2022. This progress is largely attributed to two main factors: earlier detection through increased screening, and advancements in treatment.
Mammography is a key tool in this fight. A mammogram is a low-dose X-ray of the breast tissue used for both diagnostic purposes (when symptoms are present) and routine screening (to find cancer before symptoms appear). Mammograms can detect abnormalities – including cancers, non-cancerous tumors, and cysts – often years before they can be felt by hand. While not perfect, they are a highly effective screening method.
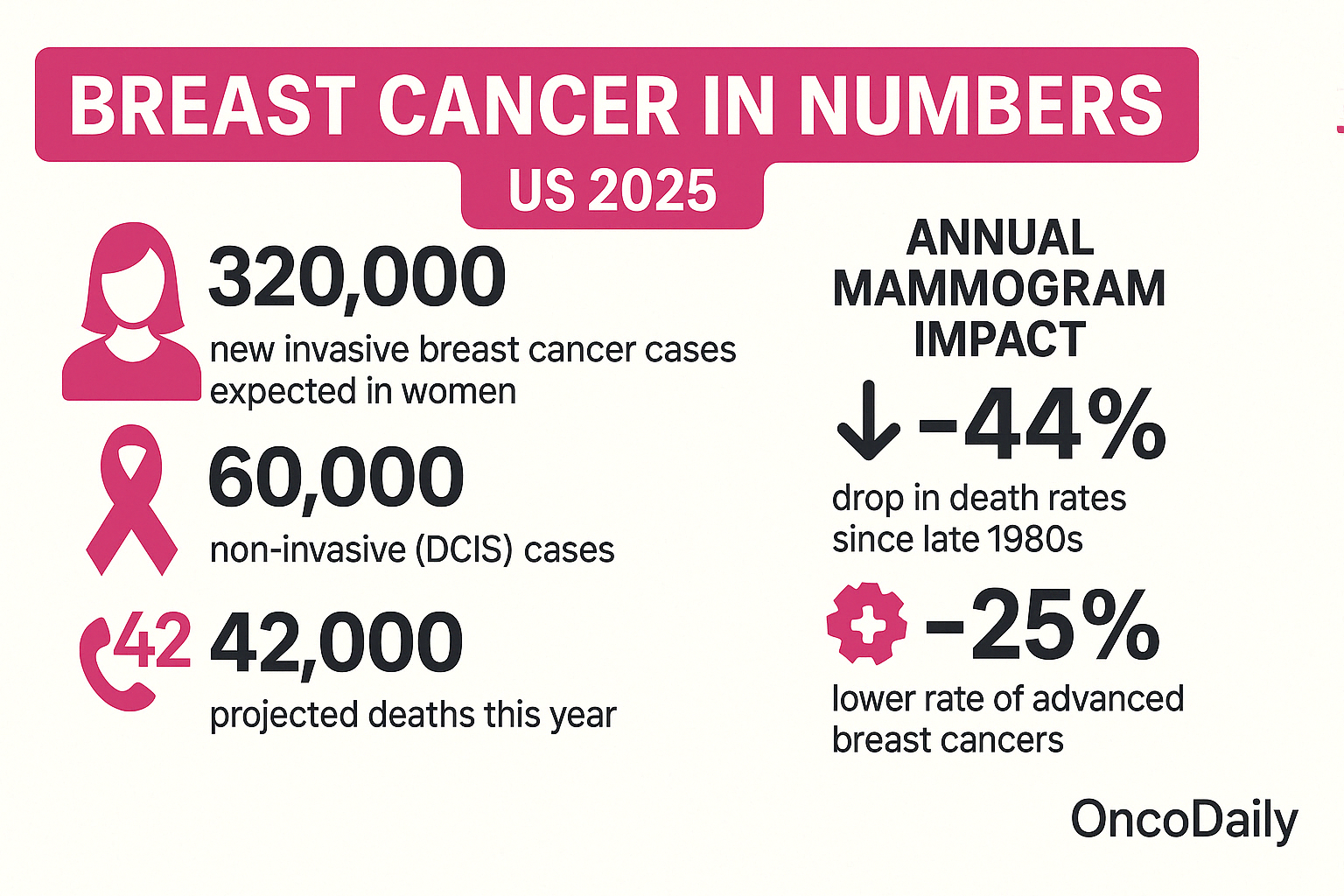
Scientific evidence supports the life-saving impact of mammography screening. A 2020 study published in the New England Journal of Medicine by Duffy et al. analyzing data from four randomized trials, found that women invited to participate in mammography screening had a significantly lower risk of dying from breast cancer. Specifically, they observed a 41% lower risk of death within 10 years (relative risk, 0.59) and a 25% lower rate of advanced breast cancers (relative risk, 0.75) compared to the control group.
The Real Cost of Mammograms
Losing the no-cost coverage mandate would reintroduce significant financial barriers to mammography and other preventive services. The cost of a screening mammogram without insurance coverage or with cost-sharing can vary widely based on location and facility, but typically ranges from $100 to $300 or even more.
- $100-$250 for standard screening mammograms
- $375-$500+ for diagnostic mammograms
- $500-$1,000+ for 3D mammograms (tomosynthesis)
For many individuals and families, particularly those with lower incomes or high-deductible health plans, these out-of-pocket costs can be prohibitive. Facing a bill for several hundred dollars for a routine screening may lead people to delay or skip their recommended mammograms altogether.
The impact of skipping or delaying mammograms due to cost is severe:
- Delayed Diagnoses: Cancers might not be found until they are larger, have spread to lymph nodes, or metastasized to other parts of the body.
- Worse Prognoses: More advanced cancers are harder to treat, require more aggressive therapies (extensive surgery, chemotherapy, radiation), and have significantly lower survival rates.
- Increased Healthcare Costs: Treating advanced breast cancer is far more complex and expensive than treating early-stage disease. This burden falls on individuals, families, and the healthcare system as a whole.
- Increased Mortality: Ultimately, delayed detection due to financial barriers will likely lead to an increase in preventable breast cancer deaths, reversing decades of progress in reducing mortality rates.
Beyond Mammography: Other Preventive Services at Risk
It’s important to note that the Braidwood case challenges the ACA mandate based on recommendations from the USPSTF and similar bodies broadly. This means that a Supreme Court ruling against the mandate could jeopardize no-cost coverage for a wide range of other essential preventive services. As the American College of Radiology has pointed out, this could potentially impact screenings for other deadly diseases, such as lung cancer CT scans for eligible individuals and colon imaging for colorectal cancer screening, among many others.
What Lies Ahead for Preventive Care Coverage
The case currently before the Supreme Court, Kennedy v. Braidwood Management, Inc., which originated as Braidwood Management Inc. et al v. Xavier Becerra et al, presents a significant juncture concerning the future of preventive healthcare services within the United States’ healthcare system. This litigation critically examines the constitutionality of a key provision of the Affordable Care Act (ACA) requiring most private health insurance plans to cover a broad spectrum of recommended preventive services without imposing cost-sharing requirements on patients.
Should the Court’s decision align with the arguments put forth by the plaintiffs, it holds the potential to substantially alter the existing framework that has facilitated access to essential health screenings, such as mammograms, immunizations, and other preventive interventions for a considerable segment of the American population.
This no-cost mandate, since its implementation under the ACA, has been associated with improved utilization of preventive services, impacting an estimated 150 million individuals by removing financial barriers that previously may have prevented them from seeking necessary care aimed at early detection and prevention of disease. The outcome of this case is therefore being closely watched for its potential implications on access to and affordability of preventive care nationwide.
“Maintaining access to affordable, no-cost preventive services like mammography is not just a matter of healthcare policy; it’s a matter of public health and saving lives”
As the Supreme Court carefully considers the arguments presented in Kennedy v. Braidwood Management, Inc., the eventual decision carries significant weight for the future delivery and accessibility of early detection and preventive health services across the United States. The ruling has the potential to influence whether and how millions of individuals access critical screenings and interventions, such as mammograms, designed to identify health issues at their earliest stages or prevent them from developing.
In light of this, remaining informed about the ongoing legal proceedings and understanding the potential outcomes is important for individuals navigating their healthcare options and for communities considering the broader public health implications. The case underscores the dynamic nature of healthcare policy and the ongoing national dialogue regarding the scope and provision of preventive care, highlighting its crucial role for individuals and communities throughout the country.