At ESTRO 2025, Dr. Matteo Lambertini, a leading expert in oncofertility, presented an in-depth overview of reproductive challenges in young women with BRCA-mutated breast cancer. His presentation focused on two major topics:
- Fertility preservation at the time of diagnosis
- The safety of pregnancy after breast cancer treatment in BRCA carriers.
Reproductive concerns are especially important in young women diagnosed with BRCA-mutated breast cancer. This patient population faces unique challenges related to fertility preservation and post-treatment pregnancy, given both the oncologic implications and the genetic predispositions involved.
Young BRCA carriers are often recommended to undergo risk-reducing surgery, such as bilateral salpingo-oophorectomy, between the ages of 35 and 45. This significantly narrows the window of reproductive opportunity. Additionally, preclinical and emerging clinical evidence suggests that BRCA mutations may negatively impact ovarian reserve by interfering with DNA repair mechanisms critical for oocyte survival, possibly leading to earlier ovarian aging.
Fertility counseling should be offered as early as possible—ideally at the time of diagnosis and certainly before initiating cancer treatment. The counseling process must include a thorough discussion of the patient’s age, mutation status, disease stage, the gonadotoxicity of planned therapies, and personal reproductive goals.
When considering fertility preservation strategies, oocyte or embryo cryopreservation is the current standard of care. This approach is effective and generally safe, even in BRCA-mutated patients. Although some studies suggest that these patients may yield fewer oocytes compared to non-carriers, outcomes are still acceptable. Short ovarian stimulation protocols, which typically last around two weeks, are considered safe even in hormone receptor-positive breast cancer, and they are widely used in clinical practice.
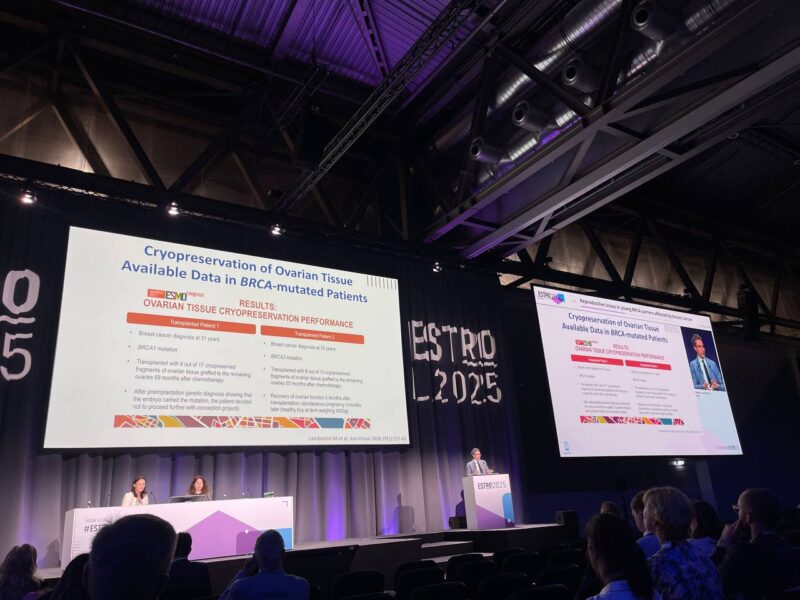
Ovarian tissue cryopreservation is not typically recommended for BRCA mutation carriers due to the elevated risk of ovarian cancer and concerns about reintroducing malignant cells. However, in very young patients or cases where immediate cancer treatment precludes oocyte stimulation, this option may be considered under strict experimental protocols. Some successful cases have been reported, though they remain rare.
The use of GnRH agonists during chemotherapy can be offered to patients as a complementary measure, especially when time or medical condition limits access to cryopreservation. While this method is less effective than cryopreservation, it may be the most feasible option in selected scenarios.
Following cancer treatment, many women—both patients and healthcare providers—remain concerned about the safety of pregnancy, particularly in BRCA mutation carriers. These concerns are largely centered on the potential hormonal stimulation of residual cancer cells and the ethical implications of passing on a genetic predisposition. However, robust clinical data, including the POSITIVE trial and multiple cohort studies, have demonstrated that pregnancy after breast cancer is safe and does not increase the risk of cancer recurrence, even in hormone receptor–positive cases. Importantly, pregnancy outcomes—including miscarriage rates, congenital abnormalities, and maternal complications—are similar to those of healthy women.
A large international study involving nearly 5,000 young women with pathogenic or likely pathogenic BRCA mutations found that approximately 22 percent of them were able to conceive after breast cancer treatment. This rate is higher than what has been reported in earlier trials, likely due to the patients’ young age, heightened reproductive awareness, and motivation given the narrowed fertility window.
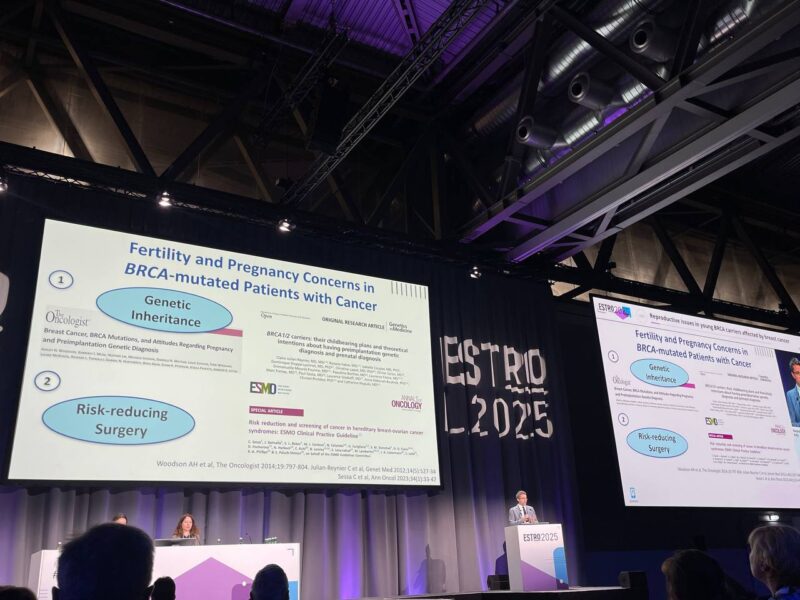
Genetic counseling is a critical component of reproductive care for BRCA mutation carriers. Women considering natural conception should be informed about the option of prenatal diagnosis, while those undergoing assisted reproduction should be offered preimplantation genetic testing to prevent transmission of the mutation. These conversations are often ethically complex and must be handled sensitively, with involvement from experienced genetic counselors.
Key takeaways
- Fertility preservation and pregnancy are both feasible and safe for BRCA-mutated breast cancer patients, provided that these topics are addressed early in the treatment process and managed through a multidisciplinary approach.
- Oocyte or embryo cryopreservation remains the preferred strategy, but alternatives such as ovarian tissue cryopreservation and the use of GnRH agonists may be appropriate in select cases.
- Long-term data now confirm that pregnancy after breast cancer is not only possible but can occur without increased oncologic risk, offering hope to young patients facing both cancer and fertility concerns.
Efforts should continue to build collaborative networks among oncologists, fertility specialists, and genetic counselors to ensure that young BRCA carriers receive personalized, timely, and compassionate reproductive care.
Read ESTRO 2025 Updates on OncoDaily.