A widely used antidepressant drug could help the immune system fight cancer, according to a new UCLA research study.
Key Takeaways
- SSRIs boosted the ability of T cells to kill cancer cells and suppressed tumor growth in both mouse and human tumor models.
- Researchers also tested a combination of an SSRI and an anti-PD-1 antibody, a common immune checkpoint blockade therapy. Together, the drugs drastically reduced tumor size and even led to complete remission in some mouse models of melanoma and colon cancer.
- Repurposing existing FDA-approved drugs like SSRIs could speed up the process of bringing new cancer treatments to patients, the researchers said.
Selective serotonin reuptake inhibitors, or SSRIs, significantly enhanced the ability of T cells to fight cancer and suppressed tumor growth across a range of cancer types in both mouse and human tumor models, the study, published in Cell, found.
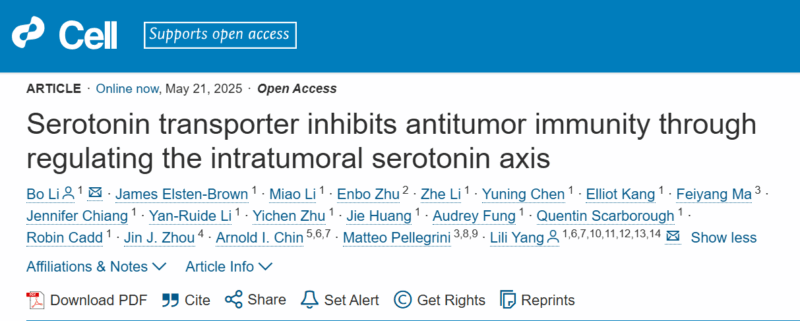
Title: Serotonin transporter inhibits antitumor immunity through regulating the intratumoral serotonin axis
Authors: Bo Li, James Elsten-Brown, Miao Li, Enbo Zhu, Zhe Li, Yuning Chen, Elliot Kang, Feiyang Ma, Jennifer Chiang, Yan-Ruide Li, Yichen Zhu, Jie Huang, Audrey Fung, Quentin Scarborough, Robin Cadd, Jin J. Zhou, Arnold I. Chin, Matteo Pellegrini, Lili Yang.
“It turns out SSRIs don’t just make our brains happier; they also make our T cells happier – even while they’re fighting tumors. These drugs have been widely and safely used to treat depression for decades, so repurposing them for cancer would be a lot easier than developing an entirely new therapy.” – said Dr. Lili Yang, senior author of the new study and a member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA.
Lili Yang
According to the CDC, one out of eight adults in the U.S. takes an antidepressant, and SSRIs are the most commonly prescribed. These drugs, sold under brand names like Prozac and Celexa, increase levels of serotonin – the brain’s “happiness hormone” – by blocking the activity of a protein called serotonin transporter, or SERT.
While serotonin is best known for the role it plays in the brain, it’s also a critical player in processes that occur throughout the body, including digestion, metabolism and immune activity.
Yang and her team first began investigating serotonin’s role in fighting cancer after noticing that immune cells isolated from tumors had higher levels of serotonin-regulating molecules. At first, they focused on MAO-A, an enzyme that breaks down serotonin and other neurotransmitters, including norepinephrine and dopamine.
In 2021, they reported that T cells produce MAO-A when they recognize tumors, which makes it harder for them to fight cancer. They found that treating mice with melanoma and colon cancer using MAO inhibitors, also called MAOIs – the first class of antidepressant drugs to be invented – helped T cells attack tumors more effectively.
However, because MAOIs have safety concerns, including serious side effects and interactions with certain foods and medications, the team turned its attention to a different serotonin-regulating molecule: SERT.
“Unlike MAO-A, which breaks down multiple neurotransmitters, SERT has one job – to transport serotonin. SERT made for an especially attractive target because the drugs that act on it – SSRIs – are widely used with minimal side effects.” – explained Dr. Bo Li, first author of the study and a senior research scientist in the Yang lab.
Bo Li
The researchers tested SSRIs in mouse and human tumor models representing melanoma, breast, prostate, colon and bladder cancer. They found that SSRI treatment reduced average tumor size by over 50% and made the cancer-fighting T cells, known as killer T cells, more effective at killing cancer cells.
Group photo of scientists in the Yang Lab at UCLA.
“SSRIs made the killer T cells happier in the otherwise oppressive tumor environment by increasing their access to serotonin signals, reinvigorating them to fight and kill cancer cells,” said Yang, who is also a professor of microbiology, immunology and molecular genetics and a member of the UCLA Health Jonsson Comprehensive Cancer Center.
How SSRIs could boost the effectiveness of cancer therapies
The team also investigated whether combining SSRIs with existing cancer therapies could improve treatment outcomes. They tested a combination of an SSRI and anti-PD-1 antibody – a common immune checkpoint blockade, or ICB, therapy – in mouse models of melanoma and colon cancer. ICB therapies work by blocking immune checkpoint molecules that normally suppress immune cell activity, allowing T cells to attack tumors more effectively.
The results were striking: the combination significantly reduced tumor size in all treated mice and even achieved complete remission in some cases.
“Immune checkpoint blockades are effective in fewer than 25% of patients. If a safe, widely available drug like an SSRI could make these therapies more effective, it would be hugely impactful.” – said James Elsten-Brown, a graduate student in the Yang lab and co-author of the study.

James Elsten-Brown
To confirm these findings, the team will investigate whether real-world cancer patients taking SSRIs have better outcomes, especially those receiving ICB therapies.
“Since around 20% of cancer patients take antidepressants – most commonly SSRIs – we see a unique opportunity to explore how these drugs might improve cancer outcomes. Our goal is to design a clinical trial to compare treatment outcomes between cancer patients who take these medications and those who do not.” – said Yang, who is also a member of the Goodman-Luskin Microbiome Center and the Parker Institute for Cancer Immunotherapy.
Yang added that using existing FDA-approved drugs could speed up the process of bringing new cancer treatments to patients, making this research especially promising.
“Studies estimate the bench-to-bedside pipeline for new cancer therapies costs an average of $1.5 billion. When you compare this to the estimated $300 million cost to repurpose FDA-approved drugs, it’s clear why this approach has so much potential.” – she said.
The newly identified therapeutic strategy is covered by a patent application filed by the UCLA Technology Development Group on behalf of the Regents of the University of California, with Yang and Li as co-inventors.
This research was supported by the National Institutes of Health, the California Institute for Regenerative Medicine, the Tower Cancer Research Foundation, a UCLA Broad Stem Cell Research Center Rose Hills Foundation Innovator Grant and a UCLA Jonsson Comprehensive Cancer Center and Broad Stem Cell Research Center Ablon Scholars Award.
Additional UCLA authors include: Miao Li, Enbo Zhu, Zhe Li, Yuning Chen, Elliot Kang, Feiyang Ma, Jennifer Chiang, Yan-Ruide Li, Yichen Zhu, Jie Huang, Audrey Fung, Quentin Scarborough, Robin Cadd, Jin J. Zhou, Arnold I. Chin and Matteo Pellegrini.
You can find more posts featuring UCLA in OncoDaily.