Elio Adib, a resident in the Harvard Radiation Oncology Residency Program, shared a post on X about a recent article published in the Journal of Thoracic Oncology:
“Our study in Journal of Thoracic Oncology CRR examining TMB/PD-L1 expression and outcomes in patients with NSCLC and new brain mets receiving brain-directed radiotherapy and immunotherapy. Grateful to collaborate with amazing colleagues.
We studied 178 patients with 536 newly-diagnosed brain metastases receiving combined treatment.
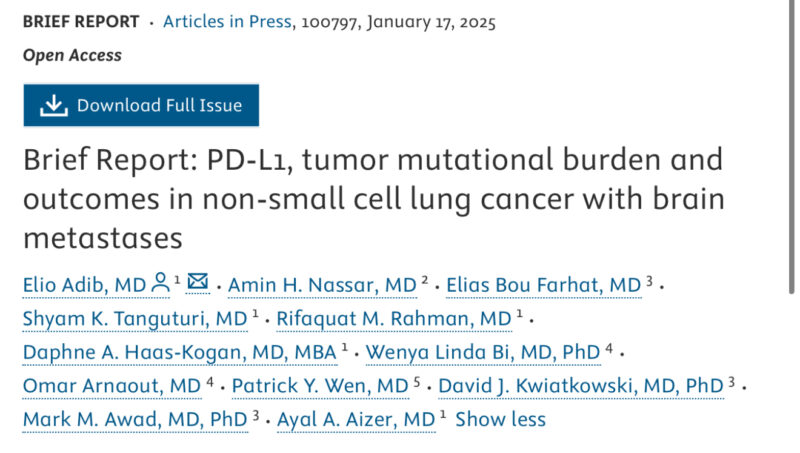
Not surprisingly, median OS was significantly longer in patients with higher PD-L1 expression. This was driven by reduced systemic (no neurologic) death.
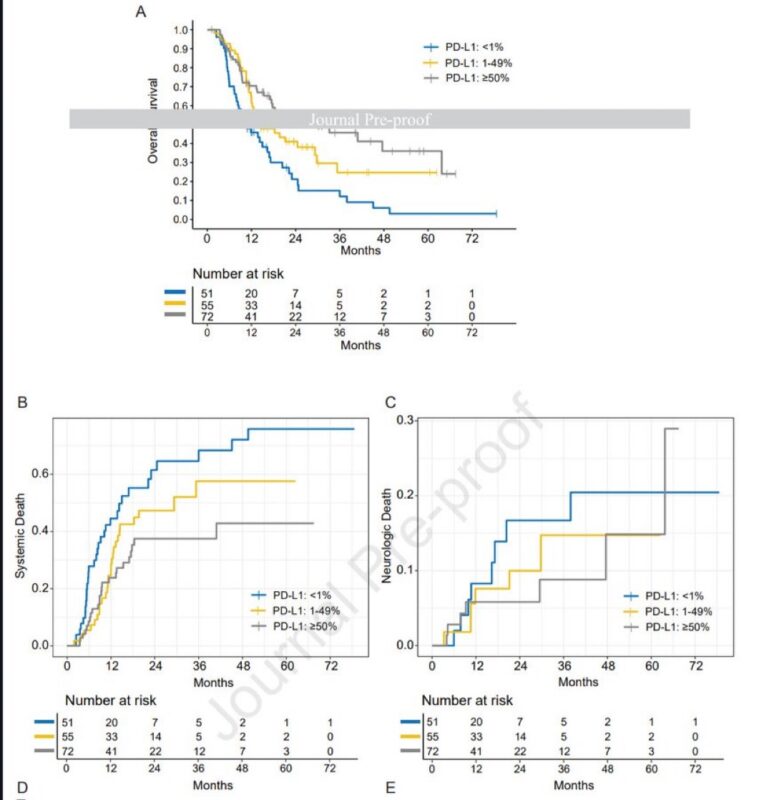
Time to intracranial and systemic progression was also improved in patients with higher PD-L1. TMB did not significantly correlate with outcomes.
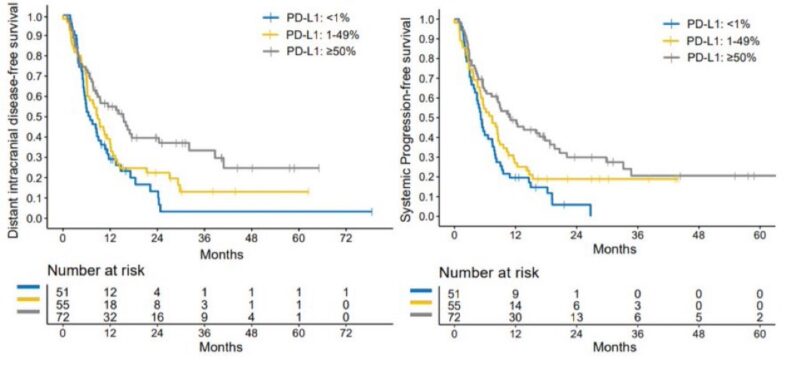
Local control after treatment was excellent (>95% at 2 years) across all categories.
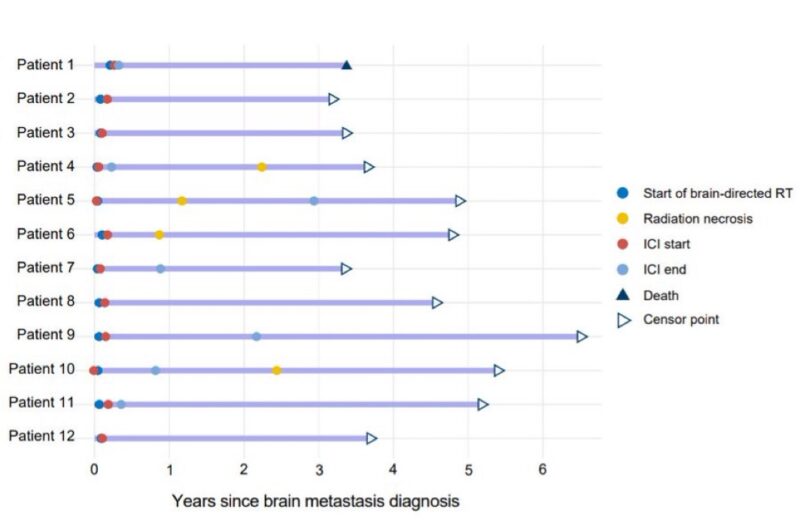
We followed 12 long-term survivors on this treatment regimen (radiotherapy and immunotherapy) who had no evidence of progression 3+ years after brain mets diagnosis; 4/12 developed symptomatic radiation necrosis.
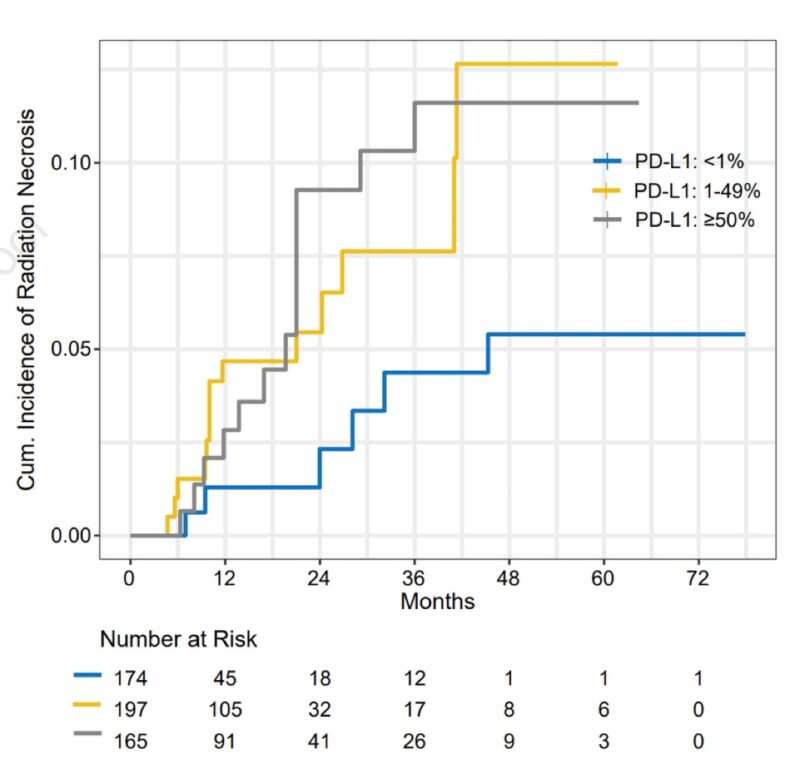
We also found that radiation necrosis rates were higher in patients with high PD-L1 expression. Since patients with high PD-L1 also had high OS (more chance for RN), we used a Fine-Gray model accounting for competing risk of death.
Conclusions:
– Combined treatment with immunotherapy and brain -directed radiotherapy is efficacious in patients with NSCLC and brain mets
– PD-L1 levels correlate with intra- and extra cranial outcomes (TMB role unclear)
– Rates of radiotherapy necrosis increased in long term survivors, especially in high PD-L1.
Huge thanks to all mentors and co-authors who contributed to this work!”