Tumor markers are substances, usually proteins, that are produced either by cancer cells themselves or by the body in response to the presence of cancer. These markers can be found in the blood, urine, tissues, or other bodily fluids, and they often serve as important clues in the diagnosis, monitoring, and management of cancer.
In this article, we will explore what tumor markers are, how they are used in clinical practice, examples of common tumor markers, their limitations and challenges, and the emerging research aiming to improve their role in modern cancer care.
How Tumor Markers Are Used
Tumor markers play several important roles in cancer care, but each role has its own strengths and limitations. In screening and early detection, very few tumor markers are reliable enough to be used across the general population. For example, while PSA (prostate-specific antigen) is sometimes used to screen for prostate cancer, its usefulness is debated because it can also be elevated in non-cancerous conditions. Most tumor markers are not sensitive or specific enough to catch cancer early without other tests.
For diagnosis, tumor markers can help support the detection of cancer but are rarely used alone. They are usually combined with imaging studies, such as CT scans or mammograms, and confirmed by biopsy. In some cancers, like testicular cancer (using AFP or β-hCG), markers can strongly support a diagnosis. When it comes to prognosis, higher levels of certain tumor markers can indicate a more aggressive or advanced cancer. For example, very high CA 19-9 levels in pancreatic cancer or CA-125 in ovarian cancer may suggest a larger tumor burden or advanced disease.
Monitoring treatment response is one of the most valuable uses of tumor markers. If levels of a marker fall during therapy, it often indicates that the treatment is working and the tumor burden is decreasing. Regular monitoring helps doctors assess whether to continue, adjust, or change therapies. Finally, tumor markers are often used to detect recurrence. If marker levels begin to rise again after treatment has ended, it can be an early sign that cancer is returning—even before it shows up on scans.
Examples of Common Tumor Markers
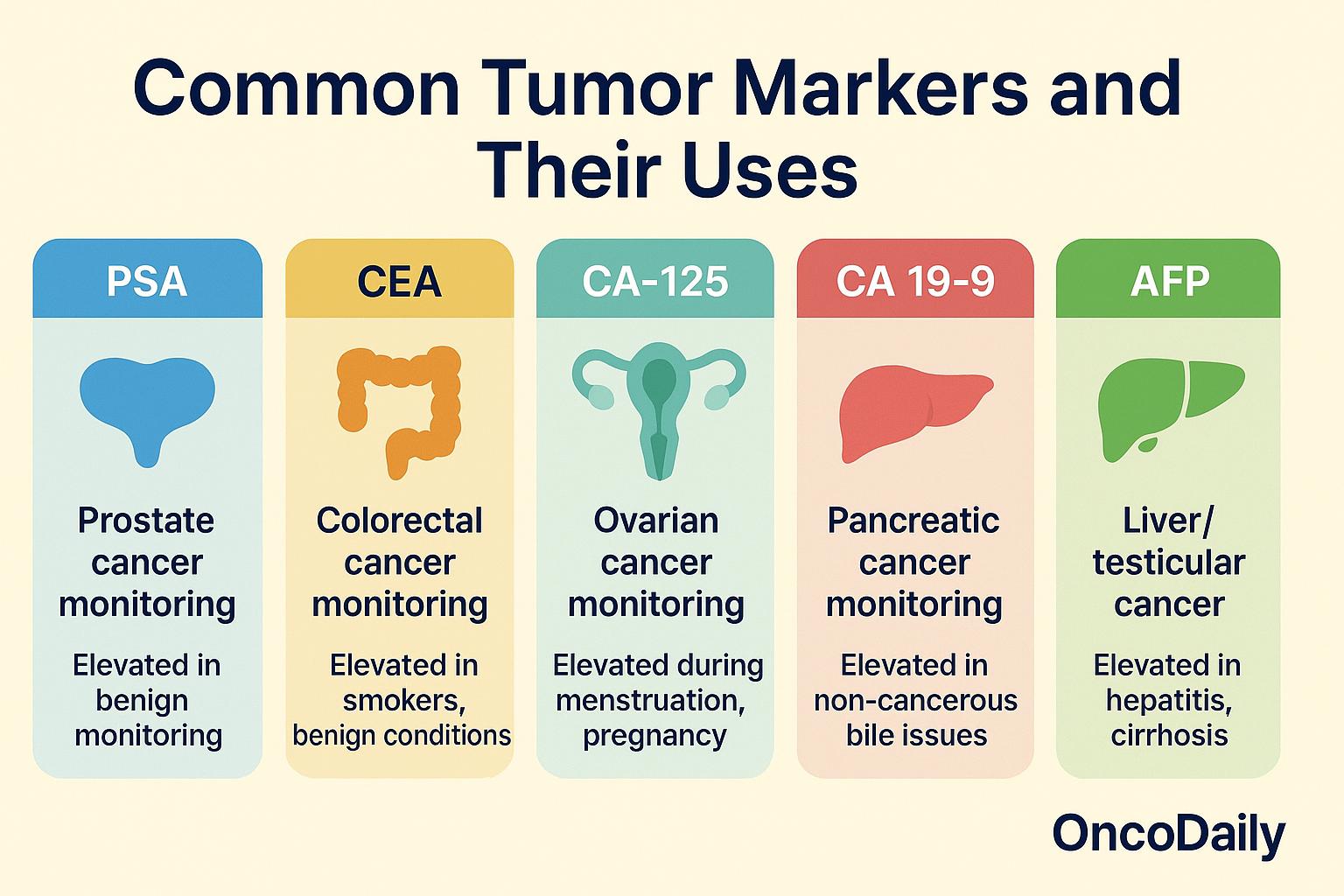
Several tumor markers are commonly used in cancer diagnosis, monitoring, and treatment planning, though each has its own limitations. One of the most widely known is PSA (Prostate-Specific Antigen), primarily used to screen for and monitor prostate cancer. Elevated PSA levels, however, are not specific to cancer and can also occur with benign conditions like prostatitis or benign prostatic hyperplasia (BPH), which can lead to false-positive results.
Another important marker is CEA (Carcinoembryonic Antigen), which is used mainly to monitor colorectal cancer. Elevated CEA levels can also be seen in lung and breast cancers. However, like PSA, CEA is not perfectly specific—smokers and individuals with certain benign conditions can also have elevated levels. For ovarian cancer, CA-125 is a commonly used marker, especially for tracking disease after treatment. While helpful for monitoring recurrence, CA-125 is less reliable for early detection because it can also rise during menstruation, pregnancy, and conditions like endometriosis.
CA 19-9 serves as a useful marker in pancreatic cancer, helping doctors assess how well treatment is working or if the disease is progressing. Still, it is not cancer-specific and can be elevated in non-cancerous conditions such as gallstones or bile duct inflammation. Another tumor marker, AFP (Alpha-fetoprotein), is often used in diagnosing and monitoring liver cancer (hepatocellular carcinoma) and certain testicular cancers. However, elevated AFP levels are also seen in chronic liver diseases like hepatitis and cirrhosis, which can complicate interpretation.
Each of these markers provides valuable information, but none are perfect on their own—emphasizing the need for comprehensive clinical assessment alongside marker testing.
Limitations and Challenges of Tumor Markers
While tumor markers are valuable tools in cancer care, they have important limitations that must be understood. One major issue is that tumor marker levels are not always specific to cancer. Many markers can rise due to benign (non-cancerous) conditions. For example, PSA levels can increase not only in prostate cancer but also in cases of prostatitis or benign prostatic hyperplasia, making it harder to distinguish between cancer and other health problems based on the marker alone.
Another challenge is the problem of false positives and false negatives. Not all cancers produce detectable tumor markers, and even when they do, the levels may not always correlate with the size or aggressiveness of the tumor. This means that a normal marker level does not necessarily rule out cancer, and an elevated level does not always confirm it. Because of these limitations, doctors cannot rely on tumor markers alone for diagnosis or treatment decisions. Tumor markers must always be interpreted alongside other clinical findings, imaging studies, and, when needed, biopsy results to ensure an accurate understanding of the patient’s condition.
Emerging Research and New Markers
Ongoing research continues to expand the field of tumor markers, aiming to discover new oncomarkers that are more accurate, sensitive, and useful in cancer care. Scientists are searching for markers that can better predict cancer presence, monitor disease progression, and detect recurrence earlier and more reliably than traditional markers.
One major area of focus is the development of multi-marker panels. Instead of relying on a single marker like PSA or CA-125, researchers are combining multiple tumor-related proteins or molecules into diagnostic panels to increase sensitivity and specificity. For example, combining CA-125 with HE4 (human epididymis protein 4) has improved the detection of ovarian cancer, particularly in women with early-stage disease. Another promising direction is the study of circulating tumor antigens and exosome-derived proteins. Tumor cells release tiny vesicles called exosomes into the bloodstream, and these carry tumor-specific proteins that may serve as early warning signs. Identifying and profiling exosomal proteins could offer a non-invasive way to detect cancer activity even before tumors become large enough to appear on imaging.
Researchers are also exploring new blood-based protein markers for hard-to-detect cancers like pancreatic and lung cancer. For instance, mesothelin and osteopontin are being studied as potential blood markers for mesothelioma and ovarian cancer, while markers like ProGRP (pro-gastrin-releasing peptide) are under evaluation for small cell lung cancer. While many of these emerging markers are still in experimental stages and not yet part of standard clinical practice, they represent important progress toward making cancer detection and monitoring more accurate, earlier, and less invasive.
You Can Watch More on OncoDaily Youtube TV
Written by Toma Oganezova, MD
FAQ
What are tumor markers?
Tumor markers are substances, often proteins, produced by cancer cells or by the body in response to cancer.
How are tumor markers used in cancer care?
They assist in diagnosis, monitoring treatment response, assessing prognosis, and detecting recurrence.
Can tumor markers be used for early cancer detection?
Rarely. Most tumor markers are not sensitive or specific enough for general screening without other tests.
What are examples of common tumor markers?
PSA (prostate cancer), CEA (colorectal cancer), CA-125 (ovarian cancer), CA 19-9 (pancreatic cancer), and AFP (liver cancer).
Are tumor markers reliable on their own?
No. They must be combined with imaging, clinical exams, and biopsies for accurate diagnosis.
What are the limitations of tumor markers?
They can be elevated in non-cancerous conditions and may sometimes give false positives or negatives.
What happens if a tumor marker level is high?
It could suggest cancer, but further testing is needed to confirm diagnosis or rule out benign causes.
How do doctors monitor cancer with tumor markers?
Doctors track marker levels over time to see if cancer is responding to treatment or returning.
What are emerging trends in tumor marker research?
Scientists are developing multi-marker panels, studying exosomal proteins, and exploring new blood markers.
Will future tumor markers improve early detection?
Yes, ongoing research aims to find markers that are more sensitive, specific, and able to detect cancer earlier.


