At SABCS 2025 (San Antonio Breast Cancer Symposium), Dr. Otto Metzger delivered an interesting talk, addressing one of the most persistent controversies in early ER-positive breast cancer: Does invasive lobular carcinoma (ILC) benefit from adjuvant chemotherapy?
Despite long-standing perceptions that lobular tumors are inherently chemoresistant, Dr. Metzger presented a nuanced evidence-based reassessment, arguing that the current clinical narrative oversimplifies the biology and risks undertreating select patients.
Lower pCR Does Not Mean Lower Chemotherapy Benefit
Clinical trials have consistently shown that ILC has much lower pCR rates compared with IDC when treated with neoadjuvant chemotherapy. In historical datasets:
- IDC pCR rate: 15%
- ILC pCR rate: 3%
- In ER/PR-positive tumors: 9% vs 4%
However, Dr. Metzger emphasized that pCR is not a meaningful surrogate for long-term benefit in ER-positive, low-proliferative cancers — including ILC.Many ER+ tumors gain survival benefit from chemotherapy despite failing to achieve pCR.
Large registries from California and the Netherlands reported no clear survival advantage for adding chemotherapy to endocrine therapy in ILC (HR ~1.0).But these datasets overwhelmingly represent patients with favorable biology and limited tumor burden — groups unlikely to benefit from chemotherapy regardless of histology.
Many ILC patients with significant anatomic burden (larger tumors, nodal involvement) were underrepresented in genomic-risk trials and population cohorts.Using these datasets as blanket evidence against chemotherapy risks undertreatment.
Prognostic vs Predictive Markers: A Critical Distinction
A major portion of the session focused on misinterpretation of genomic assays.
Prognostic markers describe the natural course of the disease independent of therapy (for example, tumor size and nodal status). They indicate overall risk of recurrence or progression, but they do not provide information about a tumor’s sensitivity to a specific treatment.
Predictive markers identify whether a patient is likely to benefit from a specific treatment. They guide therapy selection by indicating sensitivity or resistance to a particular intervention.
Most genomic assays used in ER-positive breast cancer — including Oncotype DX and MammaPrint — are prognostic tools. Their ability to predict chemotherapy benefit is inconsistent, especially in higher-risk patients.
Understanding Why Some ILC Patients Show Little “Room” for Chemotherapy Benefit
Dr. Metzger illustrated two clinical scenarios:
Scenario 1:
- Limited tumor burden + low genomic risk
- Excellent long-term DFS
- Very low early relapse risk
- Minimal space to improve outcomes with chemotherapy
Scenario 2:
- Higher tumor burden (large tumor and/or nodal positivity)
- Worse DFS trajectory
- Chemotherapy may meaningfully reduce recurrence risk even if genomic score is low
This distinction is critical, as ILC frequently yields low genomic scores, even in cases with significant anatomic risk.In lobular cancers, genomic assays frequently return very low scores, but these results should not create false reassurance when the underlying tumor burden is high.
Phase III Trials: TAILORx, MINDACT, RxPONDER
Modern genomic-risk trials transformed ER+/HER2-negative breast cancer care. But Dr. Metzger highlighted that their major conclusions apply mainly to node-negative or limited-node populations — cohorts with inherently good outcomes.
Key points across trials:
- Low genomic risk + limited disease burden = excellent prognosis
- Hard to detect additional benefit from chemotherapy in such low-risk settings
- Chemotherapy benefit did not increase with higher recurrence scores in RxPONDER
- Genomic assays are not validated predictive tools for high-risk ILC
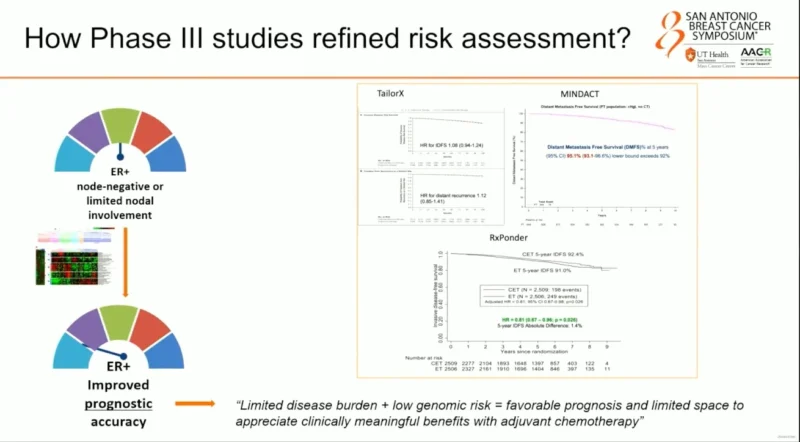
RxPONDER Trial
The primary hypothesis expected greater chemotherapy benefit with higher RS values. But observed data showed:
- Greatest benefit appeared at RS = 0
- Smallest benefit at RS = 25
This overturned the original predictive model and confirmed that Oncotype does not reliably identify chemotherapy-responsive biology.
MINDAct Trial
MINDAct remains the most informative dataset on ILC biology within genomic-risk frameworks.
- In classic ILC, 90% were low-risk by MammaPrint
- In non-classic variants, 77% low-risk, 23% high-risk
Most importantly:
When matched by genomic risk ILC and IDC have nearly identical distant metastasis–free survival and overall survival. Late relapse patterns in ILC are not unique when controlling for genomic risk.These findings demonstrate that lobular histology does not independently dictate prognosis when genomic and anatomic features are comparable.
Why Lobular Histology Should NOT Automatically Exclude Chemotherapy?
The Oxford Overview meta-analysis of anthracycline-based chemotherapy remains one of the strongest evidence sources:
- Relative benefit of chemotherapy in ER+ cancers is consistent across histology, grade, and nodal status
- Absolute benefit varies by baseline risk
- No evidence that ILC is inherently unresponsive to chemotherapy
Thus, chemotherapy can benefit ILC — the challenge is choosing the right patients.
Nuances of ILC Biology: Endocrine Sensitivity Matters
ILC tumors display a distinct biology characterized by loss of E-cadherin, unique growth patterns, and a FOXA1–ER chromatin program that contributes to relative tamoxifen resistance. Clinical data from BIG 1-98 and SOFT/TEXT further demonstrate that patients with ILC derive greater benefit from aromatase inhibitor–based endocrine therapy, with tamoxifen proving less effective compared with IDC.
These biological and clinical differences highlight the importance of optimizing endocrine therapy and maintaining a lower threshold for considering chemotherapy in patients with high tumor burden, reduced endocrine sensitivity, or other high-risk clinical and anatomic features. Emerging tools such as the SET2/3 endocrine sensitivity index may help refine treatment selection by identifying patients most likely to benefit from chemotherapy.
Dr. Metzger highlighted new research evaluating endocrine sensitivity through the SET ER/PR Index.
Early findings suggest:
- Low endocrine sensitivity = higher potential chemotherapy benefit
- High endocrine sensitivity = minimal added value from chemotherapy
- This aligns with the field’s next frontier: identifying true predictive biomarkers, not just prognostic scores.
Take-Home Messages
Patients with ILC and favorable clinical and biologic features achieve excellent long-term outcomes with endocrine therapy alone. However a small subset with high-risk biology or anatomy may benefit from chemotherapy. Over-reliance on low genomic scores risks undertreatment.Lobular histology alone should not be used to omit chemotherapy and clinical judgment integrating tumor size, nodal status, endocrine sensitivity, and patient-specific factors remains essential.
For more information click here.