When someone is diagnosed with cancer, two words quickly become emotionally charged: remission and cure. They are often used interchangeably in everyday conversation, but in oncology, they mean very different things. Understanding the difference between remission vs cure is essential for patients, caregivers, and families trying to interpret prognosis, treatment success, and long-term expectations.
This article explains what remission and cure truly mean in cancer care, how doctors use these terms, why cure is rarely declared immediately, and what patients should realistically expect over time.
Why “Remission vs Cure” Matters in Cancer Care
Cancer treatment outcomes are rarely black and white. A scan may show no visible disease, yet doctors may still hesitate to use the word cure. This can be confusing and emotionally difficult for patients who feel well and have completed treatment.
The distinction between remission vs cure exists because cancer biology is complex. Some cancers behave aggressively and recur early, while others may remain dormant for years before returning. Oncology language reflects this uncertainty and is designed to protect patients from false reassurance while allowing room for optimism.
What Does Remission Mean?
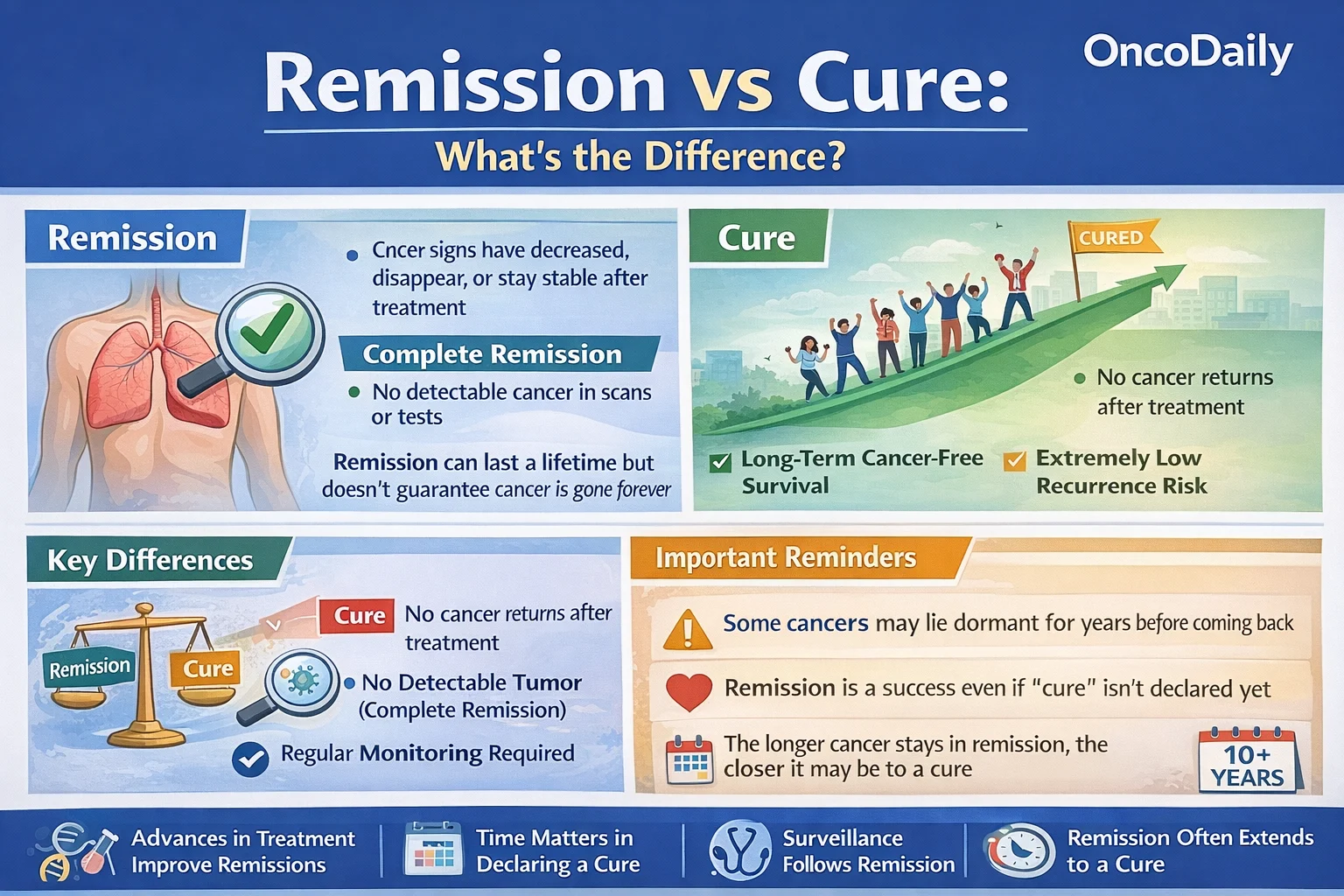
In oncology, remission means that the signs and symptoms of cancer have decreased or disappeared after treatment. Importantly, remission does not automatically mean that cancer is gone forever.
There are two main types of remission:
Complete Remission
Complete remission means that no cancer can be detected using available tests, imaging, or physical examination. Tumor markers may return to normal, and scans show no visible disease. However, microscopic cancer cells may still exist below the level of detection.
Partial Remission
Partial remission means that the cancer has shrunk significantly or become less active, but is still detectable. This is common in advanced or metastatic cancers, where the goal is often long-term disease control rather than eradication.
In the context of remission vs cure, remission describes a current state, not a final outcome.
What Does Cure Mean in Oncology?
A cure means that cancer has been eliminated and will never return. While this sounds straightforward, proving cure in cancer medicine is extremely challenging.
Unlike infections, cancer cells can remain dormant for years. Because of this, oncologists rarely declare a patient cured immediately after treatment, even if scans are clear.
Instead, cure is usually implied only after:
- Long-term cancer-free survival
- No recurrence over many years
- Risk of recurrence approaching that of the general population
In practice, cure is often declared retrospectively, not at a specific moment in time.
Why Doctors Prefer “Remission” Over “Cure”
The preference for remission over cure is not pessimism, it is scientific caution.
Cancer recurrence patterns vary widely by cancer type. For example:
- Testicular cancer often has very high cure rates
- Early-stage colon cancer may be considered cured after long follow-up
- Hormone-driven breast cancer can recur even after 10–15 years
- Some blood cancers behave as chronic diseases rather than curable ones
Because recurrence risk never drops to zero immediately, doctors use remission to describe what is known, rather than cure, which implies certainty. This careful language protects patients from emotional harm if recurrence occurs and reflects the biological reality of cancer.
How Long Does Remission Need to Last to Be Considered a Cure?
There is no universal timeline, but oncology practice has general patterns:
- 5 years disease-free is often used as a benchmark for many solid tumors
- 10 years or more may be needed for hormone-sensitive cancers
- Some childhood cancers may be considered cured earlier
- Certain cancers are never labeled cured, even with long remission
In remission vs cure, time is a critical factor. The longer remission lasts, the closer a patient comes to being functionally cured.

Read About Remission Rate in Cancer on OncoDaily
Cancer Types Where Cure Is Common
Some cancers have very high cure rates when detected early and treated appropriately:
- Early-stage testicular cancer
- Localized thyroid cancer
- Early-stage colon cancer after surgery
- Certain childhood leukemias
- Hodgkin lymphoma
In these cases, long-term survival is expected, and cure becomes a realistic goal rather than an exception.
Cancers Where Remission Is the Primary Goal
For other cancers, treatment focuses on achieving remission and maintaining it as long as possible:
• Metastatic breast cancer
• Advanced lung cancer
• Multiple myeloma
• Chronic leukemias
• Advanced pancreatic cancer
Here, remission may be deep and long-lasting, but cure is not typically expected. Advances in immunotherapy and targeted therapy have dramatically extended survival, blurring the line between chronic disease and cure.
This is a key nuance in remission vs cure discussions.
Molecular Remission and Deep Remission
Modern oncology has introduced new layers to remission.
In some blood cancers, doctors now measure minimal residual disease (MRD)—tiny traces of cancer detected only through advanced molecular tests. Patients may appear in complete remission by scans, yet still have detectable disease at the molecular level.
A deep remission or MRD-negative remission is associated with better long-term outcomes and may bring patients closer to cure, even if the word is not used explicitly.
Emotional Impact of Remission vs Cure
For patients, hearing “you’re in remission” can bring relief—but also anxiety. Many wonder:
- Does this mean the cancer will come back?
- Am I safe now?
- Why won’t my doctor say I’m cured?
Understanding the difference between remission vs cure helps patients regain a sense of control. Remission is a success, not a failure. It means treatment worked and the disease is currently under control. Fear of recurrence is common, even years into remission, and is a normal psychological response.
Surveillance After Remission
After remission, patients typically enter a follow-up or surveillance phase. This may include:
- Regular imaging
- Blood tests or tumor markers
- Physical examinations
- Long-term monitoring for late side effects
Surveillance schedules often become less frequent over time as recurrence risk decreases. This gradual spacing reflects growing confidence that remission may become durable or permanent.
Can Someone Be in Remission for Life?
Yes. Many people live the rest of their lives in remission without recurrence. In these cases, remission effectively becomes a cure, even if the word is never formally used.
This is especially true for early-stage cancers treated with curative intent. In practical terms, patients return to normal life, with cancer becoming part of their history rather than their future.
Remission vs Cure in the Era of Precision Oncology
Advances in genomics, immunotherapy, and personalized medicine are changing how we think about cancer outcomes.
Some cancers once considered incurable now achieve deep, durable remissions lasting many years. CAR T-cell therapies, immune checkpoint inhibitors, and targeted drugs are redefining survival expectations.
As a result, the boundary between remission vs cure is becoming less rigid. Long-term disease control may offer quality and length of life comparable to cure, even if cancer technically remains a possibility.
What Patients Should Take Away
Remission is not “second best.” It is a meaningful, positive outcome that reflects treatment success. Cure is a long-term conclusion that requires time, evidence, and biological certainty.
Understanding remission vs cure helps patients interpret medical language accurately, manage expectations, and focus on recovery rather than fear.
Cancer care today is not just about survival, it is about living well, for as long as possible, with or without the word “cure.”
Key Message
Remission vs cure is not a question of hope versus reality. It is a reflection of how carefully oncology balances optimism with honesty and how success in cancer is measured over time, not in a single moment.
You Can Watch More on OncoDaily Youtube TV
Written by Armen Gevorgyan, MD