Early stage Non-Small Cell Lung Cancer (NSCLC), radiotherapy is a highly effective, non-invasive treatment option, particularly for patients who are not candidates for surgery due to health reasons or personal preference.
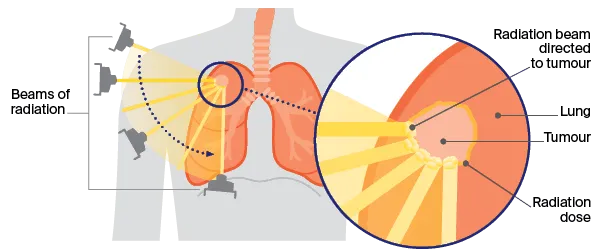
Stereotactic Body Radiation Therapy (SBRT), also known as Stereotactic Ablative Radiotherapy (SABR), is the most common and advanced form used. SBRT delivers very high, precise doses of radiation to the tumor in a few sessions (typically 1 to 5), minimizing damage to surrounding healthy tissue. This highly targeted approach has shown excellent local control rates and survival outcomes comparable to surgery in selected patients. While surgery remains the gold standard for operable patients, SBRT offers a strong alternative for many.
source: www.cancercouncil.com.au
Overview
SABR is particularly well-suited for patients who face a high surgical risk, such as individuals aged 75 or older, or those with compromised lung or cardiac function, who might not be able to tolerate a lobectomy. In situations where SABR is not feasible, less intensive but still highly conformal radiation techniques like IMRT with IGRT may be considered as alternatives. For patients who undergo surgery, postoperative radiotherapy (PORT) is generally not advised unless positive surgical margins (residual cancer cells) are present. Importantly, close follow-up and prompt treatment of any isolated local or regional recurrence after SABR have been shown to improve overall survival, as demonstrated in a large retrospective study.
When it comes to SABR dosing and application, the goal is to deliver a high-dose intensity. Regimens achieving a biologically effective dose (BED) of at least 100 Gy are strongly associated with significantly better local control and survival. In the United States, SABR typically involves five or fewer fractions (treatment sessions), though slightly more protracted regimens can also be effective. For tumors located centrally (within 2 cm of the proximal bronchial tree) or ultra-centrally (abutting the proximal bronchial tree or other critical mediastinal structures), risk-adapted regimens involving 4 to 10 fractions are preferred for both effectiveness and safety; it’s crucial to avoid high-dose, three-fraction regimens (e.g., 54 to 60 Gy in 3 fractions) due to their high toxicity.
Particular attention must be paid to tumors that abut the bronchial tree and esophagus to minimize severe side effects. Although SABR is most commonly used for tumors up to 5 cm in size, selected larger isolated tumors can also be treated safely, provided normal tissue constraints are carefully observed. Retrospective data suggest that for patients with larger tumors (5 cm or more), the addition of chemotherapy to SABR may offer a survival advantage and can be considered for appropriate candidates.
It is important to note that prescription doses alone do not fully describe the actual delivered doses; a complete understanding requires considering how the dose is prescribed, the degree of dose heterogeneity, the use of tissue density heterogeneity corrections, and the specific dose calculation algorithm. These factors are critical when interpreting or emulating regimens from previous studies.

Read OncoDaily’s Special Article About Radiotherapy for Lung Cancer
Research on Early Stage Non-Small Cell Lung Cancer
A 2009 study by Onishi et al., published in Practical Radiation Oncology, explored Stereotactic Body Radiotherapy (SBRT) as a treatment for medically operable patients with Stage I non-small-cell lung cancer (NSCLC) in Japan. The research involved 87 patients (median age 74) with Stage I NSCLC (65 T1N0M0, 22 T2N0M0) who chose SBRT over surgery between 1995 and 2004. SBRT was delivered in 3-10 fractions, with a median biological effective dose of 116 Gy. After a median follow-up of 55 months, the results were impressive: 5-year cumulative local control rates were 92% for T1 tumors and 73% for T2 tumors. Importantly, only 1.1% of patients experienced pulmonary complications above Grade 2.
The 5-year overall survival rates were 72% for Stage IA and 62% for Stage IB subgroups, and one patient with local recurrence even underwent successful salvage surgery. This study concluded that SBRT is a safe and promising radical treatment for operable Stage I NSCLC, with survival rates potentially comparable to those achieved through surgery.
A 2024 study by Ashworth et al., published in Radiotherapy and Oncology, tracked Stage I NSCLC treatment in Ontario, Canada, from 2010 to 2019. They found a significant shift: SABR use soared from 7.5% to 24.4%, while surgery decreased from 63.8% to 49.9%. Overall, 2-year cancer-specific survival improved from 81.9% to 85.0%, mainly driven by better outcomes in surgical patients. The study highlights increased SABR adoption alongside improved survival for Stage I NSCLC patients in Ontario, but also noted regional disparities in treatment access.
A comprehensive review by Wolf et al., published in Seminars in Thoracic and Cardiovascular Surgery, investigated Stereotactic Ablative Radiotherapy (SABR), also known as SBRT or SRS, as an increasingly utilized non-surgical treatment for high-risk patients with Stage I NSCLC. The expert panel conducted a systematic review of 16 prospective and 14 retrospective studies, encompassing 54,697 patients.
Their findings indicated that medical inoperability was the primary reason for SABR utilization in 93–95% of cases, with a median rate of histologically confirmed cancer in treated patients being 67% (ranging from 57–86%). Common dosing regimens observed were 48–54 Gy in 3–5 fractions in retrospective studies and 44–66 Gy in 3–5 fractions in prospective studies, with a median follow-up of 30 months (range 15–50) after SABR. The review summarized the complications, oncological outcomes, and quality of life associated with SABR in this high-risk patient group. It emphasized the ongoing need for further prospective randomized trials to compare SABR outcomes with those of sublobar resection to fully assess treatment options for this patient population.
A 2025 study by Park et al., published in Oncology Letters, retrospectively analyzed 271 patients with early-stage NSCLC treated with SBRT between 2012 and 2022, focusing on prognostic factors, symptomatic radiation pneumonitis (RP), and treatment failure. With a median follow-up of 30.8 months, the study reported impressive 1-, 2-, and 3-year overall survival rates of 96.1%, 91.8%, and 86.5%, respectively. Local control rates were similarly high at 98.8%, 96.5%, and 92.9% for the same periods.
Key findings included the Eastern Cooperative Oncology Group performance status () and a higher fractional SBRT dose () as significant predictors of overall survival. Larger tumor size () and a higher solid-to-total tumor ratio () were linked to an increased risk of local recurrence. Symptomatic RP, observed in 7.2% of lesions, was associated with solid tumor size ().
The study also noted that larger tumors with a higher solid component tended to have more in-field recurrences, while marginal recurrences were often attributed to air space spread and pleural involvement. Park et al. concluded that higher fractional doses in SBRT benefit patients with early-stage NSCLC, especially those with larger or more solid tumors, suggesting that dose escalation could optimize SBRT protocols and improve outcomes.
A 2024 study by Li et al., published in Frontiers in Oncology, evaluated the efficacy and toxicity of SBRT in 44 elderly patients ( years) with Stage I-II central NSCLC, addressing a gap in prior research focused on peripheral lung cancers. The typical SBRT dose was 60 Gy in 5 fractions. Key results included a median Progression-Free Survival of 31 months and a median Overall Survival of 69 months. The median time to cancer-specific death was 36 months, with cumulative incidences of 11.63% at 1 year, 42.99% at 5 years, and 65.94% at 10 years. Lower pre-SBRT BMI () and CAR () were significant predictors of higher overall survival.
Local and distant progression had median times of 10 and 11 months, respectively. In terms of safety, no Grade 4 or 5 acute toxicities were observed, with common Grade 1 acute toxicities including cough (38.64%) and radiation pneumonitis (29.55%). Two patients developed Grade 1 pulmonary fibrosis as a late toxicity. The study concluded that SBRT effectively controls local tumor progression with acceptable toxicity for elderly patients with centrally located Stage I-II NSCLC, and that lower pre-SBRT BMI and CAR are associated with a decreased risk of cancer-specific death.
Written By Aren Karapetyan, MD