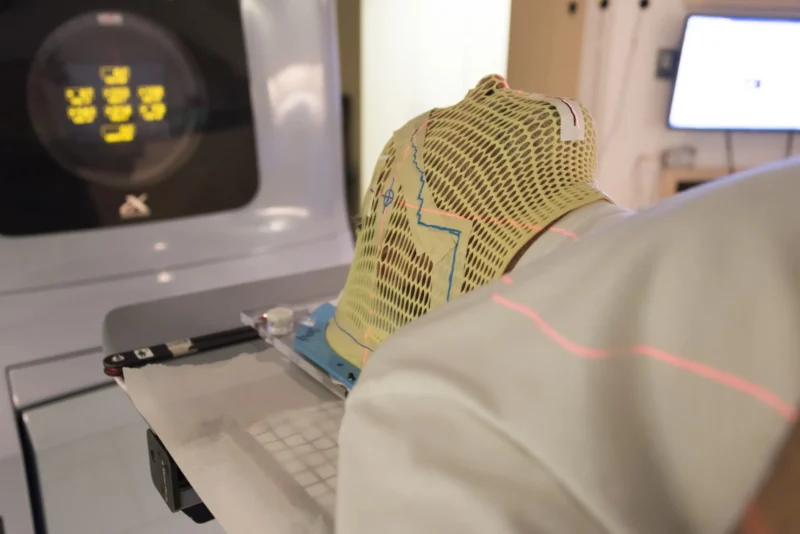
In cancer care, trust is built on verification. Plans are checked. Calculations are reviewed. Systems are validated. Yet one question rarely surfaces outside professional circles. Who checks the checkers?
Safety Is Not a Single Act
It is tempting to think of safety as a final confirmation — a last look before treatment begins. In reality, safety is cumulative. It is created through overlapping responsibilities, where no single person holds absolute authority and no single check is considered sufficient. This is not redundancy for reassurance. It is redundancy by design.
Why Expertise Is Never Left Alone
Highly trained professionals still rely on systems that challenge them. Not because they are unreliable — but because complexity demands humility. Independent reviews, peer verification, and automated safeguards exist to protect against the most human of risks: assumption. In cancer care, confidence is never a substitute for confirmation.
The Culture Behind Double-Checking
Checking the checker is not about mistrust. It is about shared responsibility. A culture where questioning is encouraged prevents silence from becoming the weak point. It creates space for pause — and pause is often what prevents harm. This culture is learned, reinforced, and protected daily.
When Nothing Goes Wrong
The most successful safety systems leave no trace. Patients don’t see the cross-checks. They don’t hear the internal discussions. They don’t know how many times a decision was reviewed before reaching the treatment room. What they experience instead is consistency — and consistency feels like calm.
Why This Matters to Patients
Patients rarely ask how many layers protect them. They ask whether treatment is safe. The answer lies not in reassurance, but in structure. Knowing that no one works alone — that every decision passes through more than one set of eyes — is what allows care to feel stable, even in uncertainty.
A Quiet Form of Accountability
Being checked is not a loss of autonomy. It is a commitment to accuracy. Professionals who accept oversight understand that safety improves when responsibility is shared and visibility is mutual. This is how high-stakes care sustains trust without relying on perfection.
A Final Thought
In cancer care, the question is not whether checks exist. It is whether the system expects them. When checkers are also checked, safety becomes a process rather than a promise. And that process — quiet, repetitive, and largely unseen — is what patients ultimately depend on.
Scientific context
The principles described in this article are grounded in established patient safety science and radiotherapy quality assurance literature. Modern cancer care safety is not achieved through a single final check, but through layered systems of verification, independent peer review, and shared accountability.
High-reliability models describe how adverse events occur only when multiple safeguards fail simultaneously. In radiotherapy, this approach is particularly critical due to the complexity of treatment planning, delivery technologies, and interdisciplinary workflows.
International guidelines and peer-reviewed studies consistently demonstrate that independent peer review before treatment initiation plays a central role in identifying latent errors and preventing near-miss events. Safety culture research further emphasizes that environments encouraging questioning, cross-checking, and open communication are associated with improved detection of errors and greater system resilience.
From the patient’s perspective, the success of these systems remains largely invisible. When safety mechanisms function as intended, patients experience stability, consistency, and trust — outcomes that reflect intentional system design rather than chance.
In this context, oversight is not a limitation of professional autonomy, but a defining feature of responsible, high-stakes care.
Written By Eftychia Tataridou, MD