Palliative care aims to relieve suffering and improve quality of life for patients facing serious illness. Yet in many parts of the world, including Armenia, the system built to deliver this care is underdeveloped. The result is a dual burden: patients in need struggle to access compassionate care, and doctors tasked with providing it are often left unsupported, undertrained, and emotionally overwhelmed.
In conversations about palliative care, the focus is often on expanding access for patients, improving quality of life, and building better systems of delivery. But one angle that frequently goes overlooked—particularly in low- and middle-income countries—is the experience of the providers themselves. What happens when the doctors tasked with delivering compassionate, end-of-life care aren’t given the training, tools, or institutional support they need?
This was the central question behind a study presented at MASCC 2025 by Martin Harutyunyan. The study surveyed 124 physicians across Armenia, most of whom work in primary care—a frontline setting where palliative care is urgently needed but rarely integrated.

The results were sobering.
The Disconnect Between Importance and Preparedness
While 96% of doctors surveyed reported having no formal training in palliative care, more than 85% recognized it as essential to their daily practice. Yet only 14% said they are able to integrate palliative care “always” in their work. The majority said they could only do so “sometimes” or “rarely.” This points to a stark reality: even when providers understand the importance of palliative care, they often lack the practical means to deliver it.
Major Barriers: Resources, Training, and Family Hesitation
When asked about the barriers they face in integrating palliative care, the responses were strikingly consistent:
- 82% cited lack of resources, such as medications, equipment, or dedicated spaces
- 51% pointed to a lack of training, both during medical school and in ongoing professional development
Many also highlighted hesitancy or resistance from patients’ families, which complicates discussions around end-of-life care.
These challenges aren’t theoretical—they manifest in everyday clinical work. Time constraints, diagnostic pressures, and the emotional toll of working with terminally ill patients create a stressful environment, particularly when there is no institutional framework to support palliative decision-making.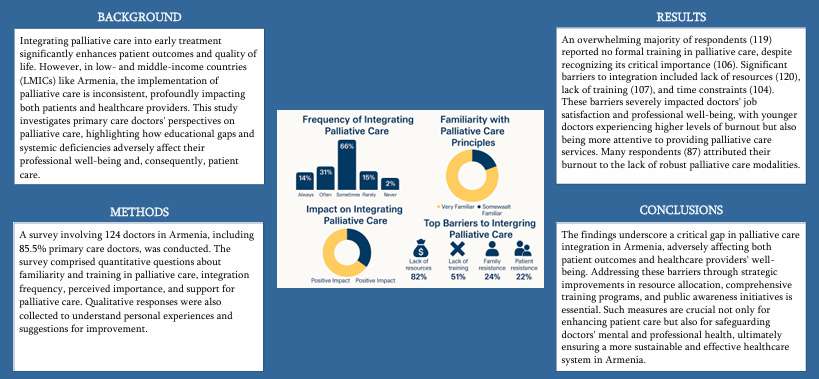
The Human Cost: Burnout and Emotional Strain
Perhaps the most compelling finding of the survey was its reflection of physician burnout. Nearly 90 doctors reported experiencing significant emotional strain linked directly to the lack of palliative care resources and structure. Physicians described the frustration of wanting to help, knowing what their patients need, but not being able to deliver that care effectively or sustainably.
Younger physicians in particular—those fresh out of training or early in their careers—reported feeling both more emotionally impacted and more motivated to provide palliative care. This dual burden of hope and helplessness puts them at risk of early burnout.
Why It Matters for Everyone
The implications of this study go beyond individual doctors. When providers lack the tools to deliver palliative care, patients and families suffer too. Pain goes unaddressed. Communication breaks down. Trust in the health system erodes.
But it doesn’t have to be this way.
What Needs to Change
The study calls for strategic interventions across three key areas:
- Early integration of palliative care training in medical education
- Resource allocation—ensuring that clinics and hospitals are equipped to deliver basic palliative services
- Public and family education to reduce stigma and hesitancy around palliative care
Improving palliative care is often framed as a patient-centered mission—and rightly so. But supporting the caregivers is an equally critical part of the equation.
When we train, support, and empower our doctors, their care becomes more compassionate, consistent, and sustainable. And when doctors feel equipped, patients feel it too. That’s the kind of ripple effect this field urgently needs—and deserves.