Oncoviruses, classified as group 1 carcinogens by the IARC, directly or indirectly cause up to 20% of cancers worldwide. Major agents include Epstein-Barr virus (EBV), human papillomavirus (HPV), hepatitis B/C viruses (HBV/HCV), Kaposi’s sarcoma-associated herpesvirus (KSHV), and human T-cell lymphotropic virus (HTLV-1). Direct carcinogens like EBV and HPV produce proteins that disable tumor suppressors (e.g., p53), enabling uncontrolled cell growth. Indirect agents such as HBV and HCV drive malignancy through chronic inflammation and liver damage, while HIV-1 exacerbates risks by weakening immunity. Collectively, these viruses reshape the tumor microenvironment, promoting immune evasion, inflammation, and angiogenesis. This article examines their cancer-causing mechanisms and global health strategies to combat their impact.
Photo: Depositphotos
Who Are the Viral Culprits Behind Human Cancers?
Oncoviruses are a distinct group of viruses which are classified as group 1 human carcinoge
ns by the International Agency for Research on Cancer (IARC), responsible for a significant fraction of human cancers worldwide. The principal oncoviruses include Epstein-Barr virus (EBV), human papillomavirus (HPV), hepatitis B virus (HBV), hepatitis C virus (HCV), Kaposi’s sarcoma-associated herpesvirus (KSHV), human T-cell lymphotropic virus type 1 (HTLV-1), and human immunodeficiency virus type 1 (HIV-1). These viruses contribute to carcinogenesis through both direct and indirect mechanisms, often involving persistent infection and complex interactions with host cellular pathways.
EBV, HPV, HTLV-1, and KSHV are considered direct carcinogens that encode viral proteins capable of inactivating tumor suppressors and promoting cellular transformation. For instance Human papillomavirus (HPV) is a diverse group of more than 200 related viruses, of which approximately 12 are classified as high-risk types due to their strong association with cancer. Among these, HPV 16 and HPV 18 are the most oncogenic, responsible for about 70% of cervical cancer cases globally. Other high-risk types include HPV 31, 33, 35, 45, 52, and 58. These high-risk HPVs produce viral proteins that inactivate tumor suppressors such as p53 and retinoblastoma protein, leading to cellular transformation and cancer development.
In contrast, low-risk types like HPV 6 and 11 primarily cause benign lesions such as genital warts. EBV is intelected in nasopharyngeal carcinomas and various lymphomas by immortalizing B cells and modulating immune response. KSHV causes Kaposi’s sarcoma and certain lymphomas by altering cytokine secretion and promoting angiogenesis. HTLV-1 induces adult T-cell leukemia/lymphoma through degranulation of T-cell proliferation.
In contrast, HBV and HCV act as indirect carcinogens primarily through chronic inflammation and liver damage, which increase the risk of hepatocellular carcinoma. HBV integrates into the host genome, disrupting normal gene function, while HCV induces persistent hepatic inflammation and fibrosis. On the other hand, HIV-1 although it is not directly oncogenic can contribute to risk of cancer by causing immunosuppression that facilitates the reactivation and oncogenic activity of other viruses such as KSHV and EBV.

Collectively, oncoviruses alter the tumor microenvironment by promoting immune evasion, chronic inflammation, metabolic reprogramming, and angiogenesis, thereby facilitating tumor initiation, progression, and metastasis. Globally, these viruses account for approximately 12–20% of all cancers, with the highest burden observed in regions lacking widespread vaccinations and antiviral therapies. According to Mesri et al. (2014), oncoviruses play a significant role in cancer development by manipulating key cellular pathways and evading host immune responses, which underscores the urgent need for continued research to refine antiviral treatments and develop targeted therapies aimed at mitigating the global burden of virus-associated malignancies.
Can Finding Viral Traces in Cancer Help Predict Outcomes and Guide Treatment?
Virus-associated cancers, caused by oncoviruses like HPV, EBV, and hepatitis viruses, remain a major global health challenge. Early detection and precise monitoring are key to improving patient outcomes, and this is where biomarkers measurable indicators of disease play a transformative role.
Identifying Viral and Host Biomarkers
Scientists have made significant progress in pinpointing both viral and host biomarkers that help detect cancers early, predict disease progression, and monitor treatment response. For example, viral DNA fragments circulating in the blood, known as circulating tumor DNA (ctDNA), can reveal the presence of HPV-related cancers even before symptoms appear. Host biomarkers, such as proteins like CD44 and genetic changes in tumor suppressor genes (e.g., p53 and Rb), provide crucial information about tumor behavior and patient prognosis.
The Rise of Liquid Biopsies
Liquid biopsies, simple blood tests that detect tumor DNA or viral genetic material are revolutionizing cancer care. Unlike traditional tissue biopsies, liquid biopsies are minimally invasive, can be repeated easily, and offer real-time insights into how a tumor evolves or responds to treatment. This approach is especially valuable in virus-associated cancers, where viral genetic material can serve as a direct biomarker. According to Passaro et al. (2024), liquid biopsies are emerging as a powerful tool in personalized cancer treatment, enabling clinicians to monitor tumor dynamics and adapt therapies more effectively based on molecular changes detected in the blood.
Molecular Diagnostics in Clinical Practice
Advanced molecular diagnostic tools now allow oncologists to tailor treatments based on a tumor’s unique molecular profile. For instance, detecting specific viral oncoproteins or mutations helps guide targeted therapies and immunotherapies, improving effectiveness and reducing side effects. These tools also help identify patients at higher risk of metastasis, enabling closer monitoring and timely intervention.
Looking Ahead
As research advances, integrating viral and host biomarkers with cutting-edge molecular diagnostics promises earlier detection, better prognosis, and personalized treatment for patients with virus-associated cancers. Continued innovation and wider clinical adoption of these technologies will be essential to reduce the global burden of these cancers.
What’s Behind the Unequal Burden of Virus-Related Cancers Across the Globe?
Viruses are responsible for up to about 10–15% of cancers worldwide, with human papillomavirus (HPV) and hepatitis B and C viruses (HBV and HCV) being the most significant contributors to preventable cancers. These oncoviruses cause a substantial proportion of cancers, including cervical, liver, and several other malignancies. However, access to life-saving vaccines, screenings, and antiviral therapies is uneven globally, leading to higher cancer risks in regions with limited healthcare resources. This disparity means millions face increased vulnerability to virus-associated cancers simply due to where they live or their healthcare availability. According to Gallo, Montagnier, and Weiss (2017), addressing these inequalities through expanded vaccination programs and improved screening is critical to reducing the global burden of oncovirus-related cancers.
What Role Do Healthcare Inequities Play in the Global Burden of Virus-Driven Cancers?
Cervical cancer remains a major health challenge worldwide, especially in low- and middle-income countries where nearly 94% of the 350,000 annual deaths occur. Sub-Saharan Africa bears the highest burden, with 18 of the 20 countries with the greatest incidence located in the region. The disease is about six times more common there than in Europe, largely due to limited access to HPV vaccination, effective screening, and timely treatment. Women living with HIV are six times more likely to develop cervical cancer, further increasing the risk in high HIV-prevalence areas.
Despite being largely preventable, less than 6% of eligible women in Africa have ever been screened, and many cases are detected too late for effective treatment. The World Health Organization’s global strategy focuses on three key goals by 2030: vaccinating 90% of girls by age 15, screening 70% of women by ages 35 and 45 with high-performance tests, and ensuring 90% of women with cervical disease receive appropriate treatment. Achieving these targets is essential to reduce the stark inequalities and save millions of lives.
You Can Also Read Cervical Cancer: Symptoms, Causes, Stages, Diagnosis and Treatment by Oncodaily
What Can Be Done?
The good news? We have powerful tools to fight back:
Vaccinations against oncoviruses are transforming cancer prevention worldwide. The World Health Organization (WHO) recommends HPV vaccines for young people before they become sexually active and universal hepatitis B vaccination for newborns, as these vaccines can prevent most virus-related cancers.
In the United States, following the introduction of the HPV vaccine, infections caused by vaccine-type HPV among females aged 14–19 dropped by 64% between 2003–2006 and 2009–2012, according to NHANES data.
Cervical cancer rates in vaccinated groups have been reported to be up to 87% lower than in unvaccinated cohorts. Similarly, in Europe, countries like Belgium and Hungary have achieved HPV vaccination coverage rates of 80–90% among girls before age 15, leading to significant declines in HPV prevalence and precancerous lesions. However, vaccination rates vary widely across Europe, with some regions reporting coverage as low as 20% (European Cancer Organisation).
Universal hepatitis B vaccination programs have also dramatically reduced chronic hepatitis B infections by over 90% in vaccinated populations, leading to a sharp decline in liver cancer rates, especially in Asia. Taiwan’s HBV vaccination program, for example, reduced childhood liver cancer incidence by approximately 70% within two decades (WHO data).
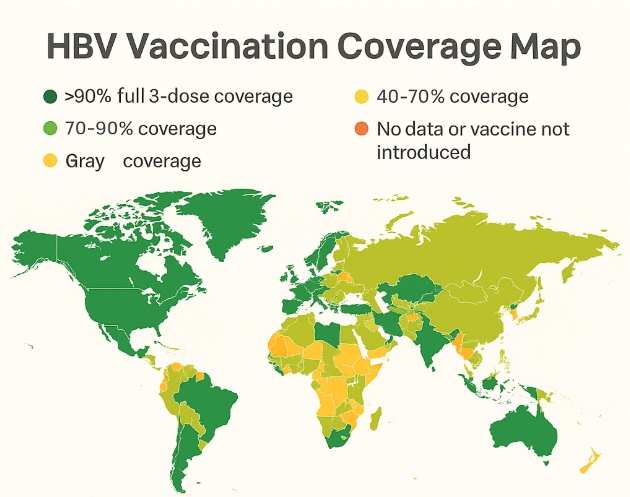
Regular cervical cancer screening and liver cancer monitoring remain essential for early detection and effective treatment. Expanding vaccine availability, reducing costs, and increasing public awareness are critical steps to closing the global gap in virus-related cancer prevention (Syrjanen et al., Nowotwory Journal of Oncology, 2019; European Cancer Organisation; WHO).
Your Role and Hope for the Future
If you or your loved ones haven’t been vaccinated or screened, talk to your healthcare provider. These simple steps can save lives. Globally, organizations like WHO, ASCO, and ESMO are pushing for equitable access to vaccines and screenings because everyone deserves a fair chance to beat cancer.
Together, by raising awareness and supporting prevention programs, we can turn the tide against oncovirus-related cancers and build a healthier future for all.
Written by Marine Marashlian
FAQ
What are oncoviruses?
Oncoviruses are viruses that can cause cancer in humans by directly or indirectly altering cellular processes that control growth and division.
Which viruses are classified as oncoviruses?
Major oncoviruses include human papillomavirus (HPV), Epstein-Barr virus (EBV), hepatitis B and C viruses (HBV, HCV), Kaposi’s sarcoma-associated herpesvirus (KSHV/HHV-8), human T-cell lymphotropic virus type 1 (HTLV-1), and Merkel cell polyomavirus (MCV).
How do oncoviruses cause cancer?
Oncoviruses can cause cancer by inserting their genetic material into host cells, disrupting tumor suppressor genes, promoting chronic inflammation, or weakening the immune system.
What types of cancer are linked to oncoviruses?
Oncoviruses are linked to cervical, liver, nasopharyngeal, anal, some lymphomas, Kaposi’s sarcoma, and certain head and neck cancers.
How common are virus-related cancers worldwide?
Oncoviruses account for about 12–20% of all cancers globally, with higher rates in regions lacking widespread vaccination and antiviral therapy.
Can oncovirus-related cancers be prevented?
Yes, many can be prevented through vaccination (HPV, HBV), safe practices, and regular screening for early detection.
Who is at higher risk for oncovirus-related cancers?
People with chronic viral infections, immunosuppression (such as HIV infection), or limited access to vaccines and healthcare are at higher risk.
Are there vaccines for oncoviruses?
Vaccines are available for HPV and HBV, which can greatly reduce the risk of related cancers.
How are oncovirus infections diagnosed?
Diagnosis may involve molecular tests (PCR), serology, or detection of viral DNA/RNA in blood or tissue samples.
What are the symptoms of oncovirus-related cancers?
Symptoms vary by cancer type but may include unexplained weight loss, persistent fatigue, lumps, chronic pain, or abnormal bleeding.
What is the outlook for people with oncovirus-related cancers?
Prognosis depends on the cancer type, stage at diagnosis, and access to effective treatment and prevention strategies. Early detection and vaccination improve outcomes
How are oncovirus-related cancers treated?
Treatment may include surgery, chemotherapy, radiation, antiviral therapy, immunotherapy, or targeted therapies, depending on cancer type and stage.