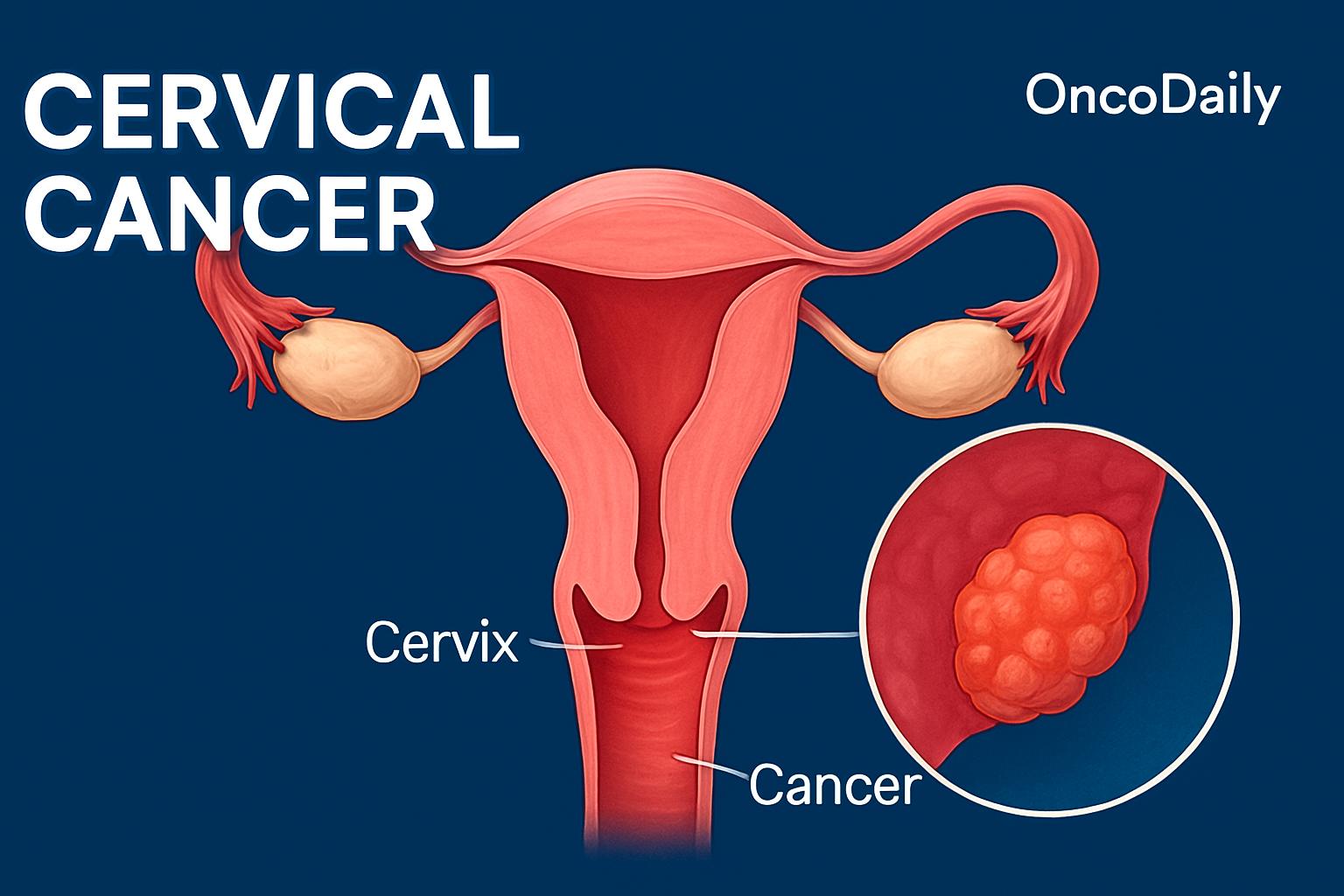
Cervical cancer is a type of cancer that occurs in the cells of the cervix, which is the lower part of the uterus connecting to the vagina. Cervical cancer is a significant global health concern, particularly in less developed regions where it ranks as the second most commonly diagnosed cancer and the third leading cause of cancer-related deaths among women. According to The Global Cancer Observatory (GLOBOCAN), cervical cancer was indeed reported to have approximately 660,000 new cases globally in 2022. This underscores the ongoing need for effective prevention, early detection, and treatment strategies worldwide.
The disease is primarily caused by persistent infection with high-risk types of human papillomavirus (HPV), a common sexually transmitted virus. Early detection through regular screenings, such as Pap tests and HPV tests, plays a crucial role in identifying precancerous lesions and preventing the progression to invasive cancer.
This article aims to provide a thorough exploration of cervical cancer, covering its symptoms, causes, diagnostic methods, stages, treatment options, and the latest advancements in research. By addressing these aspects, the article seeks to enhance understanding of the disease, promote awareness, and highlight progress in prevention and treatment strategies.
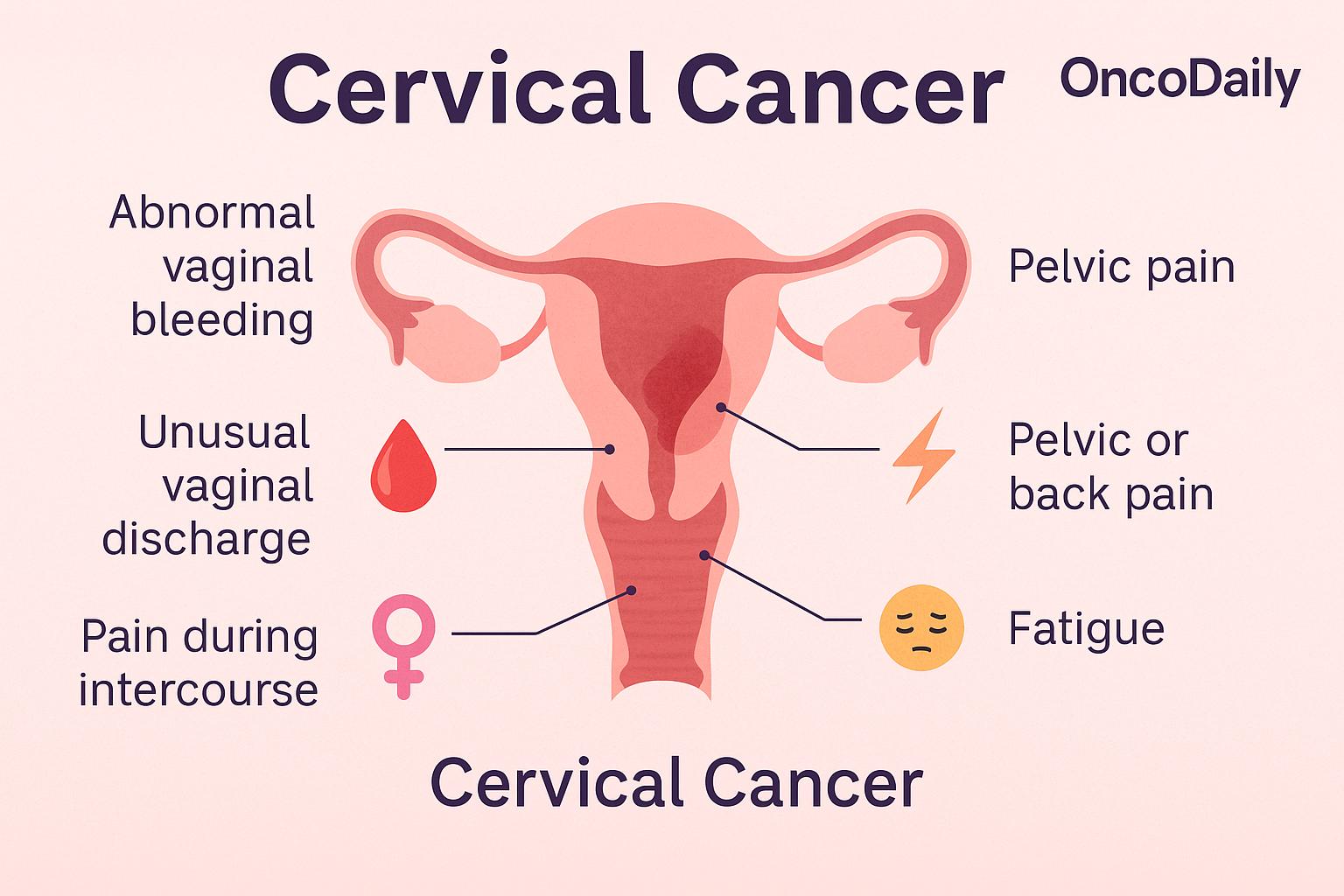
What Are the Symptoms of Cervical Cancer?
Cervical cancer often begins without any noticeable symptoms, which is why many women remain unaware of its presence until it has progressed. In the early stages, signs can be subtle or completely absent. When symptoms do appear, they commonly include abnormal vaginal bleeding—such as bleeding between periods, after intercourse, or following menopause—along with unusual vaginal discharge that may be watery, pink, or foul-smelling. Some women may also experience pelvic pain or discomfort during sex, though these symptoms can be mistaken for other conditions.
As the disease advances, the symptoms become more pronounced. Women with later-stage cervical cancer may report persistent pelvic or back pain, swelling in the legs due to lymphatic obstruction, or problems with urination and bowel movements caused by tumor pressure. Fatigue and unexplained weight loss are also frequent indicators of advanced disease.
Many women do not show symptoms until the cancer has grown significantly or spread, which makes routine screening essential. According to the American Cancer Society, the five-year survival rate for early-stage cervical cancer is as high as 91%, but drops to around 67% for more advanced cases. Pap tests and HPV testing—recommended starting at ages 21 and 25, respectively—are critical tools for catching the disease before symptoms arise. Early detection not only improves the chances of survival but can often lead to less intensive treatment and better quality of life.
What Are the Causes and Risk Factors for Cervical Cancer?
Cervical cancer is primarily caused by long-term infection with certain high-risk types of human papillomavirus (HPV), a very common virus that is spread through sexual contact. According to the World Health Organization (WHO) and the ICO/IARC HPV Information Centre, HPV is responsible for nearly all cases of cervical cancer. In particular, HPV types 16 and 18 are the most dangerous, accounting for about 70% of all cases worldwide.
Most HPV infections go away on their own without causing any problems. However, when the infection doesn’t clear and becomes persistent, it can cause changes in the cells of the cervix. If these abnormal cells are not detected and treated early, they can eventually develop into cancer. Certain factors increase the risk of developing cervical cancer, especially in the presence of an ongoing HPV infection. These risk factors include:
-
Having multiple sexual partners, which increases the likelihood of exposure to high-risk HPV types.
-
Smoking, which weakens the immune system and damages cervical cells, making it harder for the body to fight off HPV.
-
Long-term use of birth control pills (typically more than five years), which has been associated with a slightly increased risk.
-
A weakened immune system, such as from HIV infection or immunosuppressive medications, which reduces the body’s ability to clear HPV.
What Are the Types of Cervical Cancer?
Cervical cancer is primarily categorized into two main types: squamous cell carcinoma and adenocarcinoma, which together account for the vast majority of cases. Less commonly, cervical cancer can also present as small cell carcinoma and other rare histological subtypes. Each type differs in how it develops, how common it is, and how it may respond to treatment.
Squamous Cell Carcinoma of the Cervix
Squamous cell carcinoma (SCC) is the most common form of cervical cancer, making up approximately 80–90% of all cases. It begins in the squamous cells, which are the thin, flat cells that line the outer part of the cervix, called the ectocervix. These cells are especially vulnerable to persistent infection with high-risk types of human papillomavirus (HPV), particularly HPV-16, which is the leading cause of SCC.
One of the reasons SCC is more frequently detected than other types is because it typically develops in the transformation zone—the area where the squamous and glandular cells meet—which is also the region sampled during routine Pap smears. This makes it more likely to be caught early with regular screening.
An interesting fact about SCC is that it tends to respond better to radiation and chemotherapy than adenocarcinoma, especially in advanced stages. According to a study by Liu et al. in BMC Cancer (2022), the 5-year overall survival rate for SCC after treatment was significantly higher (72.2%) compared to adenocarcinoma (56.9%). This makes early identification and correct histological classification particularly important for optimizing outcomes.
Adenocarcinoma of the Cervix
Adenocarcinoma is a less common but significant type of cervical cancer, accounting for about 10–20% of all cases. It begins in the glandular cells located in the endocervix, the inner lining of the cervical canal that produces mucus. Unlike squamous cell carcinoma, which develops on the outer surface of the cervix, adenocarcinoma tends to form deeper within the cervical canal, making it more difficult to detect early through routine Pap smears.
Because of its location, adenocarcinoma is often missed in early screening, particularly if the abnormal cells are not well-sampled during a Pap test. This contributes to a trend where adenocarcinomas are often diagnosed at more advanced stages than squamous cell cancers. An interesting point is that adenocarcinomas are more likely to occur in younger women, and the incidence has been rising, partly due to limitations in screening methods that are better at detecting squamous abnormalities. Additionally, HPV-18 is more strongly associated with adenocarcinoma than HPV-16, and research suggests that adenocarcinomas may be less responsive to radiation therapy compared to squamous types, especially in later stages.
How Is Cervical Cancer Diagnosed?
Diagnosing cervical cancer involves several important steps that work together to detect abnormal changes and confirm the presence of cancer. These tools are used either during routine screening or when symptoms raise concern:
-
Pap Smear: This test checks for abnormal cells on the cervix that could develop into cancer over time. It’s often the first step in detecting early, precancerous changes.
-
HPV Testing: This test looks for high-risk types of human papillomavirus (especially HPV-16 and HPV-18) that are known to cause most cervical cancers. It’s often done alongside a Pap smear or when Pap results are unclear.
-
Colposcopy: If Pap or HPV results are abnormal, a colposcopy may be performed. This is a simple procedure where the doctor uses a special microscope (colposcope) to closely examine the cervix for suspicious areas.
-
Biopsies: If any abnormal areas are seen during colposcopy, a small sample of tissue (biopsy) is taken and sent to a lab to check for cancer or pre-cancer. This is the only way to confirm a diagnosis of cervical cancer.
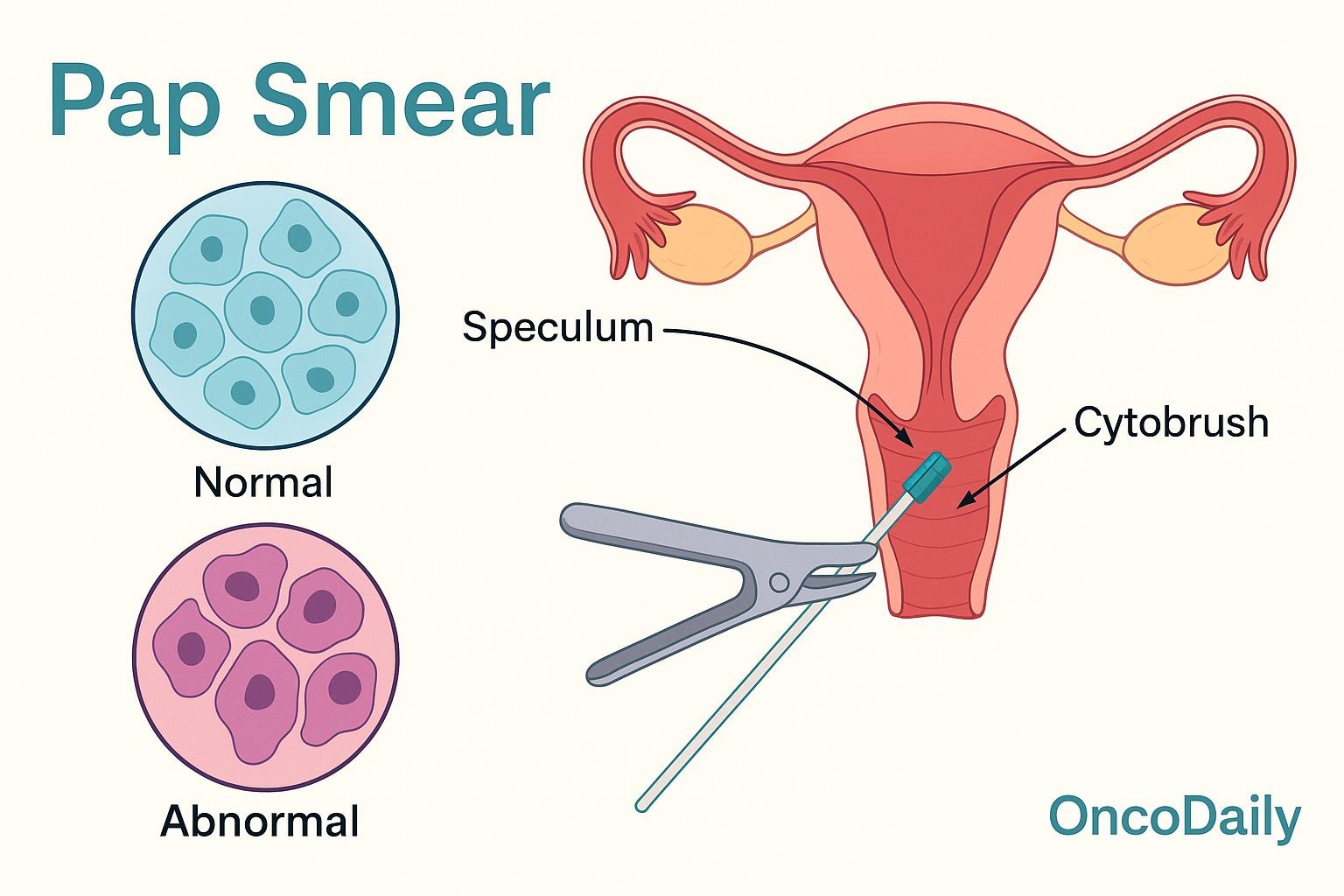
Pap Smear for Cervical Cancer Screening
Pap smears (also called Pap tests) play a critical role in the early detection and prevention of cervical cancer. The test involves collecting cells from the cervix and examining them under a microscope to identify any abnormalities that could lead to cancer if left untreated. By detecting precancerous changes (such as cervical intraepithelial neoplasia), Pap smears allow for early intervention before cancer develops.
Screening should begin at age 21. According to the American Cancer Society, women between the ages of 21 and 29should have a Pap test every 3 years. Starting at age 30, women should either continue with a Pap test every 3 years or choose co-testing (Pap smear + HPV test) every 5 years. After age 65, women with a history of regular normal results may stop screening.
Pap smears have significantly reduced cervical cancer mortality. According to data from the American Cancer Society and the National Cancer Institute, widespread Pap smear screening has led to a 70% decrease in cervical cancer deaths in countries where the test is routinely performed. This dramatic drop highlights how effective early detection is in preventing invasive cancer and saving lives.
HPV Testing for Cervical Cancer
HPV testing has become a crucial part of cervical cancer screening. Unlike the Pap smear, which looks for abnormal cells, HPV testing detects the presence of high-risk types of human papillomavirus—particularly types 16 and 18—that are known to cause the majority of cervical cancer cases. This test is especially important for women aged 30 to 65, where it can be used either on its own every five years, or alongside a Pap smear (a method known as co-testing) for more comprehensive screening.
According to recommendations from the U.S. Preventive Services Task Force, supported by ACOG, ASCCP, and the Society of Gynecologic Oncology, screening should begin at age 21 with a Pap smear. Starting at age 30, women have more options: they can choose to continue with Pap tests every three years, opt for HPV testing alone every five years, or combine both tests every five years. A positive HPV result doesn’t mean cancer is present—it simply indicates a higher risk and the need for closer follow-up.
If HPV or Pap test results are abnormal, further evaluation may be done through a colposcopy. During this procedure, the doctor uses a magnifying instrument called a colposcope to closely examine the cervix. A special solution is applied to highlight any suspicious areas, and if needed, a biopsy is taken. Biopsies are the definitive way to confirm a diagnosis. Small samples of tissue may be collected through a punch biopsy or endocervical curettage. In some cases, a cone biopsy may be done to remove a larger, cone-shaped section of cervical tissue for closer examination.
Colposcopy and Biopsy
A colposcopy is a diagnostic procedure that allows doctors to closely examine the cervix, vagina, and vulva for signs of abnormal cells. Using a colposcope—a special magnifying device with a bright light—the doctor can get a clear, enlarged view of the tissue to identify any areas that look suspicious. If any abnormalities are seen during the exam, a biopsy may be done to take a small sample of tissue for closer analysis in a lab. This helps confirm whether the changes are precancerous or cancerous. There are a few types of biopsies that may be performed during a colposcopy:
-
Punch biopsy: A small piece of tissue is removed from the surface of the cervix.
-
Endocervical curettage (ECC): Cells are gently scraped from inside the cervical canal.
-
Cone biopsy: A larger, cone-shaped section of tissue is removed, usually under anesthesia, to examine deeper layers of the cervix.
What Are the Treatment Options for Cervical Cancer?
Treatment for cervical cancer depends on the stage of the disease, overall health, and whether the patient wishes to preserve fertility. The main treatment options include:
-
Surgery, such as cone biopsy (removal of a cone-shaped section of tissue), trachelectomy (removal of the cervix while preserving the uterus), and hysterectomy (removal of the uterus, sometimes along with surrounding tissues).
-
Radiation therapy, which uses high-energy rays to destroy cancer cells, often combined with chemotherapy in more advanced stages.
-
Chemotherapy, which uses drugs to kill cancer cells or stop their growth, typically used for more advanced or recurrent cancers.
-
Targeted therapy, which focuses on specific molecules involved in cancer growth, and is often used when standard treatments are less effective.
These treatments may be used alone or in combination, depending on the stage and individual needs. Survival rates and recovery experiences vary by treatment type and cancer progression, which will be explored in detail with supporting data and real patient stories.
Surgery for Cervical Cancer
Surgical treatment is a key approach for cervical cancer, especially in its early stages, and the specific procedure depends on the stage of disease, tumor size, and whether fertility preservation is desired. One of the most conservative surgical methods is the cone biopsy, or conization, which involves removing a cone-shaped portion of tissue from the cervix. It is typically used for stage IA1 cervical cancer or high-grade precancerous lesions, especially in young women who want to maintain fertility. Most patients recover within 4 to 6 weeks, with mild cramping and bleeding being common post-operative symptoms. According to the American Cancer Society, cone biopsy has a high success rate when the margins are clear, meaning all abnormal tissue has been removed.
For women with early-stage cervical cancer (stage IA2 to IB1) who wish to preserve fertility, trachelectomy may be an option. This procedure removes the cervix but leaves the uterus intact, allowing for the possibility of future pregnancy. It is generally considered when the tumor is less than 2 cm in size. Recovery typically takes about 6 weeks, and studies such as the one by Wang et al., published in BMC Women’s Health in 2023 (PMCID: PMC10676234), report 5-year overall survival rates of 95.9% and disease-free survival rates of 94.5% following this surgery. However, women who undergo trachelectomy may face increased risks of miscarriage and preterm birth.
In more advanced stages, such as IB2 or higher, hysterectomy is the most commonly recommended surgical approach. This involves the removal of the uterus and cervix, and in the case of radical hysterectomy, also includes surrounding tissues and parts of the upper vagina. Recovery from hysterectomy varies depending on the surgical technique but usually takes 4 to 6 weeks. Hospital stays range from one to five days. For early-stage cervical cancer, the 5-year survival rate after hysterectomy often exceeds 90%, according to the American Cancer Society. However, a study published in the New England Journal of Medicine by Ramirez et al. (2018) indicated that minimally invasive hysterectomy might be associated with higher recurrence rates compared to open surgery, prompting reconsideration of surgical technique in certain patients.
Radiation Therapy and Chemotherapy
Chemotherapy and radiotherapy are central to the treatment of locally advanced cervical cancer (LACC), particularly in stages IB2 to IVA. Over the past two decades, the combination of these therapies—known as concurrent chemoradiotherapy (CRT)—has become the standard of care, supported by strong evidence from multiple randomized trials. Studies endorsed by the National Cancer Institute have shown that CRT significantly improves both disease-free survival (DFS) and overall survival (OS) compared to older treatments such as radiotherapy (RT) alone or RT combined with hydroxyurea. A systematic review and meta-analysis of 13 randomized trials reported that adding chemotherapy to radiotherapy increased 5-year overall survival by about 6% (hazard ratio [HR] = 0.81, P < .001).
CRT works by simultaneously targeting the tumor with localized radiation while using chemotherapy to treat cancer cells throughout the body, including micrometastases. This dual mechanism makes CRT especially effective in controlling disease both locally and systemically. One of the major recent advances has been the use of neoadjuvant chemotherapy (NACT)—chemotherapy administered before CRT. According to the European Society for Medical Oncology (ESMO), NACT offers several benefits: it can shrink the primary tumor to improve operability, eradicate micrometastatic disease, reduce the number of hypoxic (oxygen-deprived) cancer cells that are resistant to treatment, and increase tumor vascularization to enhance radiation sensitivity. When followed by radical surgery, NACT has shown survival advantages over radiotherapy alone.
The INTERLACE trial recently provided compelling new data supporting this approach. In this large, international study, patients with LACC received a short course of induction chemotherapy with carboplatin and paclitaxel before standard CRT. The results showed a 35% reduction in recurrence and a 40% reduction in cervical cancer deaths. After five years, 80% of patients receiving the new approach were still alive, compared to 72% who received standard CRT alone. Despite the clear benefits, combining radiation and chemotherapy does come with increased risk of side effects. A study involving 1,030 women with cervical cancer found that 56% experienced adverse effects from CRT. The most common issues included gastrointestinal symptoms (92.5%), neurological problems like numbness or tingling (78.5%), skin reactions (73.3%), and genitourinary complications such as urinary frequency or discomfort (71.0%).
These findings underscore both the life-saving potential of chemoradiotherapy in advanced cervical cancer and the importance of monitoring and managing treatment-related side effects. With ongoing research and refinement of protocols like NACT, outcomes continue to improve, offering greater hope for long-term survival.
After Treatment: What to Expect
After cervical cancer treatment, patients may experience side effects such as fatigue, early menopause, bladder or bowel changes, and sexual health concerns. Recovery time varies depending on the treatment type, but most women return to normal activities within weeks to months. Regular follow-up care is essential, especially in the first 2–3 years, when recurrence is most likely. Check-ups typically include pelvic exams and imaging or blood tests. According to studies, recurrence occurs in about 11–22% of early-stage cases and up to 64% in advanced stages.
Long-term health monitoring focuses on managing late side effects, detecting recurrence early, and supporting emotional and physical recovery. Maintaining a healthy lifestyle, staying active, and keeping follow-up appointments are key to post-treatment well-being.
How Is Cervical Cancer Prognosis Determined?
The prognosis for cervical cancer largely depends on the stage at diagnosis, tumor size, and whether cancer has spread to lymph nodes. Early-stage cancers (Stage I) have a 5-year survival rate of over 90%, while this drops to around 60% for Stage II, and 30–50% for Stage III. In Stage IV, the survival rate is typically less than 20%, according to data from the SEER database (National Cancer Institute).
Larger tumors and positive lymph node involvement are linked to poorer outcomes. For example, a study by Matsuo et al. (Journal of Clinical Oncology, 2015) found that patients with lymph node metastases had a significantly reduced 5-year survival compared to those without. Personalized treatment plans are developed by considering these factors—along with patient age, fertility desires, and overall health—to choose the most effective therapies while minimizing side effects.
How to Live with Cervical Cancer?
Living with cervical cancer can be challenging, both physically and emotionally. Managing side effects like fatigue, nausea, and early menopause involves resting when needed, eating a balanced diet, staying hydrated, and discussing symptom relief with your care team. Emotionally, it’s normal to feel anxious or overwhelmed—counseling, support groups, or talking to a therapist can help.
Building a support system is key: lean on family, friends, and cancer support organizations. Staying connected, asking for help, and sharing your feelings can make a big difference. Mindfulness, light exercise, and setting small daily goals also help maintain a sense of control and well-being during treatment.
Can Cervical Cancer Be Prevented?
Preventing cervical cancer starts with HPV vaccination, which protects against high-risk HPV types responsible for about 90% of cases. According to the CDC, the vaccine is most effective when given between ages 9–12, but can be given up to age 45.
Regular Pap smears and HPV tests help detect abnormal cells early—when treatment is most effective. Experts recommend starting screening at age 21 and continuing as advised by your doctor. Practicing safe sex—using condoms and limiting the number of sexual partners—also reduces HPV risk. In daily life, staying up-to-date on vaccines, attending routine checkups, and making informed choices about sexual health are key steps to prevention.
You Can Watch More on OncoDaily Youtube TV
Written by Mariam Chkheidze, MD
FAQ
What is cervical cancer and how does it develop?
Cervical cancer occurs when abnormal cells in the cervix grow uncontrollably, often due to persistent infection with high-risk human papillomavirus (HPV).
What are the early symptoms of cervical cancer?
Early symptoms may include abnormal vaginal bleeding (especially after sex or between periods), unusual discharge, or pelvic pain, though many cases are symptomless early on.
What causes cervical cancer?
The primary cause is long-term infection with high-risk types of HPV, particularly HPV-16 and HPV-18. Other risk factors include smoking, multiple sexual partners, and a weakened immune system.
How is cervical cancer diagnosed?
Diagnosis typically begins with a Pap smear or HPV test, followed by colposcopy and biopsy if abnormalities are found.
What are the types of cervical cancer?
The main types are squamous cell carcinoma (most common) and adenocarcinoma. Rare subtypes include small cell carcinoma.
How accurate are Pap smears and HPV tests?
Pap smears are very effective for detecting precancerous changes. HPV testing identifies high-risk virus types, increasing early detection accuracy when combined with Pap smears.
What is the treatment for early-stage cervical cancer?
Treatment may involve cone biopsy, trachelectomy, or hysterectomy, depending on stage and fertility goals. Early-stage cancers often have excellent outcomes.
What is chemoradiotherapy and when is it used?
Chemoradiotherapy combines chemotherapy with radiation and is the standard treatment for locally advanced cervical cancer (stages IB2–IVA).
Can cervical cancer be prevented?
Yes. HPV vaccination, regular screening with Pap/HPV tests, and safe sex practices significantly reduce the risk.
What is the survival rate for cervical cancer?
The 5-year survival rate is over 90% for Stage I, drops to 60% for Stage II, and falls below 20% in Stage IV. Early detection greatly improves survival.