Pancreatic ductal adenocarcinoma (PDAC) is characterized by poor long-term outcomes, even in patients with localized but locally advanced disease. Within this setting, the phase II NEOLAP trial (AIO-PAK-0113) evaluated induction chemotherapy followed by surgical exploration as a strategy to increase the likelihood of margin-negative (R0) resection, which remains a key determinant of survival. Despite the use of contemporary multiagent induction regimens, clinical outcomes remain heterogeneous, underscoring the need for reliable biomarkers to support prognostic stratification and treatment planning.
Against this background, the NEOLAP trial provided a unique prospective framework for biomarker evaluation in patients with non-metastatic PDAC treated with standardized induction chemotherapy. The present translational analysis investigated the clinical relevance of growth differentiation factor-15 (GDF-15) within this context. The results of this translational biomarker analysis were published as an Original Article in ESMO Gastrointestinal Oncology in 2026.
Title: Growth differentiation factor-15 (GDF-15) in localized pancreatic adenocarcinoma treated with multiagent chemotherapy: a biomarker analysis from the NEOLAP trial (AIO-PAK-0113)
Authors: B. Kimmel, S.T. Löhnert, F. Wedekink, M. Günther, S. Ormanns, I. Hartlapp, J. Siveke, G. Siegler, S. Boeck, H. Algül, U. Martens, F. Kullmann, T. Ettrich, S. Held, F. Anger, C.-T. Germer, V. Heinemann, J. Wischhusen, and V. Kunzmann
What is GDF-15?
Growth differentiation factor-15 (GDF-15), also referred to as macrophage inhibitory cytokine-1, is a member of the transforming growth factor-β superfamily that is minimally expressed under physiological conditions. Its production is induced in response to cellular stress, including inflammation, tissue injury, metabolic imbalance, and malignant transformation.
In cancer, elevated circulating GDF-15 levels have been repeatedly associated with adverse clinical outcomes, including in pancreatic ductal adenocarcinoma. Importantly, GDF-15 does not primarily reflect tumor burden. Instead, it appears to act as a stress-induced, immune-regulatory mediator that influences interactions between tumor cells, the tumor microenvironment, and systemic host responses.
In addition, GDF-15 plays a recognized role in cancer-associated cachexia. Together, these features support its relevance as both a biologically meaningful biomarker and a potential therapeutic target.
Methods
This biomarker study was conducted within the prospective, multicenter, randomized phase II NEOLAP trial (AIO-PAK-0113). Patients with therapy-naïve, locally advanced (borderline resectable or unresectable), non-metastatic PDAC received 4 months of induction chemotherapy with either nab-paclitaxel plus gemcitabine alone or nab-paclitaxel plus gemcitabine followed by sequential FOLFIRINOX. Patients without disease progression underwent surgical exploration with intent to resect.
Circulating GDF-15 (cGDF-15) was measured at baseline and after induction chemotherapy (week 16) using enzyme-linked immunosorbent assay. Tumor GDF-15 (tGDF-15) expression was assessed by immunohistochemistry on paired tumor specimens obtained before and after chemotherapy, with positivity defined as ≥10% GDF-15-positive tumor cells.
Results
Among 165 patients enrolled in NEOLAP, 131 patients with available baseline cGDF-15 measurements constituted the biomarker study population. Baseline characteristics and outcomes were representative of the overall NEOLAP cohort.
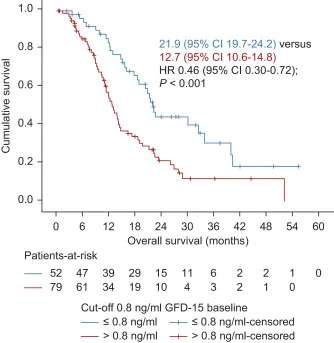
Baseline cGDF-15 levels were strongly associated with clinical outcomes. Patients with low baseline cGDF-15 (≤0.8 ng/ml) achieved significantly longer overall survival than those with higher levels, with median OS of 21.9 versus 12.7 months. This prognostic effect was also observed in patients who did not undergo R0 resection, although with reduced magnitude.
Baseline cGDF-15 was additionally predictive of surgical outcome. Patients with low baseline levels achieved substantially higher secondary R0 resection rates compared with patients with elevated cGDF-15 (36.5% versus 13.9%).
During induction chemotherapy, circulating GDF-15 levels increased significantly, rising from a median of 1.0 ng/ml at baseline to 2.37 ng/ml at week 16. The increase was observed in both treatment arms but was more pronounced in patients receiving platinum-based chemotherapy. Changes in cGDF-15 during treatment were not associated with objective response, resection status, or CA 19-9 dynamics.
Tumor GDF-15 expression was uncommon at baseline and primarily restricted to tumor cells. After induction chemotherapy, tGDF-15 positivity increased markedly, in parallel with rising circulating levels. Higher baseline cGDF-15 correlated with detectable tumor expression, and conversion from negative to positive tGDF-15 after chemotherapy was closely associated with increasing cGDF-15 levels.
Conclusion
These NEOLAP trial updates identify baseline circulating GDF-15 as a prognostic and predictive biomarker in localized, non-metastatic PDAC treated with multiagent induction chemotherapy. Low baseline cGDF-15 identifies patients with improved survival and a higher likelihood of achieving margin-negative resection.
The consistent induction of GDF-15 during chemotherapy—particularly with platinum-based regimens—together with its independence from tumor burden and parallel up-regulation at the tumor level, supports a biologically relevant role for GDF-15 in treatment response and disease evolution and provides a strong rationale for further investigation. These findings provide a strong rationale for further investigation of GDF-15-directed strategies in future PDAC clinical trials.
Read full article here.