The term “malignant” is used to describe cells that behave aggressively—they grow uncontrollably, invade nearby tissues, and have the ability to spread (metastasize) to distant parts of the body through the blood or lymphatic system. Malignant tumors are what we commonly refer to as cancers. This is different from benign tumors, which may grow but do not invade surrounding tissues or spread to other areas. While benign tumors can sometimes cause problems if they grow large enough, they are generally less dangerous than malignant tumors.
In this article, we will explore how malignant tumors develop, their key characteristics, the different types of malignancies, how they are diagnosed, treatment options available, and what factors influence the prognosis. Understanding malignancy is critical for recognizing the seriousness of a cancer diagnosis and the importance of early detection and modern treatments.
How Malignant Tumors Develop
Malignant tumors develop when normal cells lose control over their growth and behavior. Under healthy conditions, cells grow, divide, and die in a tightly regulated way, ensuring that tissues remain balanced and functional. However, when critical control systems in a cell are damaged, the cell can begin to divide uncontrollably and become cancerous.
The process usually starts with DNA mutations—changes in the genetic material of the cell. These mutations can affect genes that regulate cell growth (oncogenes), cell death (tumor suppressor genes), or the repair of damaged DNA. If enough mutations accumulate, the normal balance between cell growth and cell death is lost. Another key factor is the failure of normal programmed cell death, a process known as apoptosis. Healthy cells that are damaged beyond repair are supposed to self-destruct through apoptosis. In cancerous cells, this “self-destruct” mechanism is often disabled, allowing damaged and abnormal cells to survive and continue dividing.
As a result of unchecked division and survival, a mass of abnormal cells forms, invades surrounding tissues, and eventually has the potential to spread (metastasize) to distant organs. Several factors contribute to the development of malignant tumors. Some mutations are inherited genetically, meaning a person is born with a higher risk of cancer. However, many mutations arise from environmental exposures, such as tobacco smoke, radiation, harmful chemicals, and ultraviolet light from the sun. Lifestyle factors—like poor diet, obesity, physical inactivity, and alcohol use—also increase cancer risk. Additionally, certain infections, including human papillomavirus (HPV), hepatitis B and C viruses, and Helicobacter pylori bacteria, are known to contribute to the development of specific cancers.
While not every exposure leads to malignancy, and not every mutation causes cancer, it often takes a combination of multiple genetic alterations and environmental influences over time to transform a normal cell into a malignant one.
Characteristics of Malignant Tumors
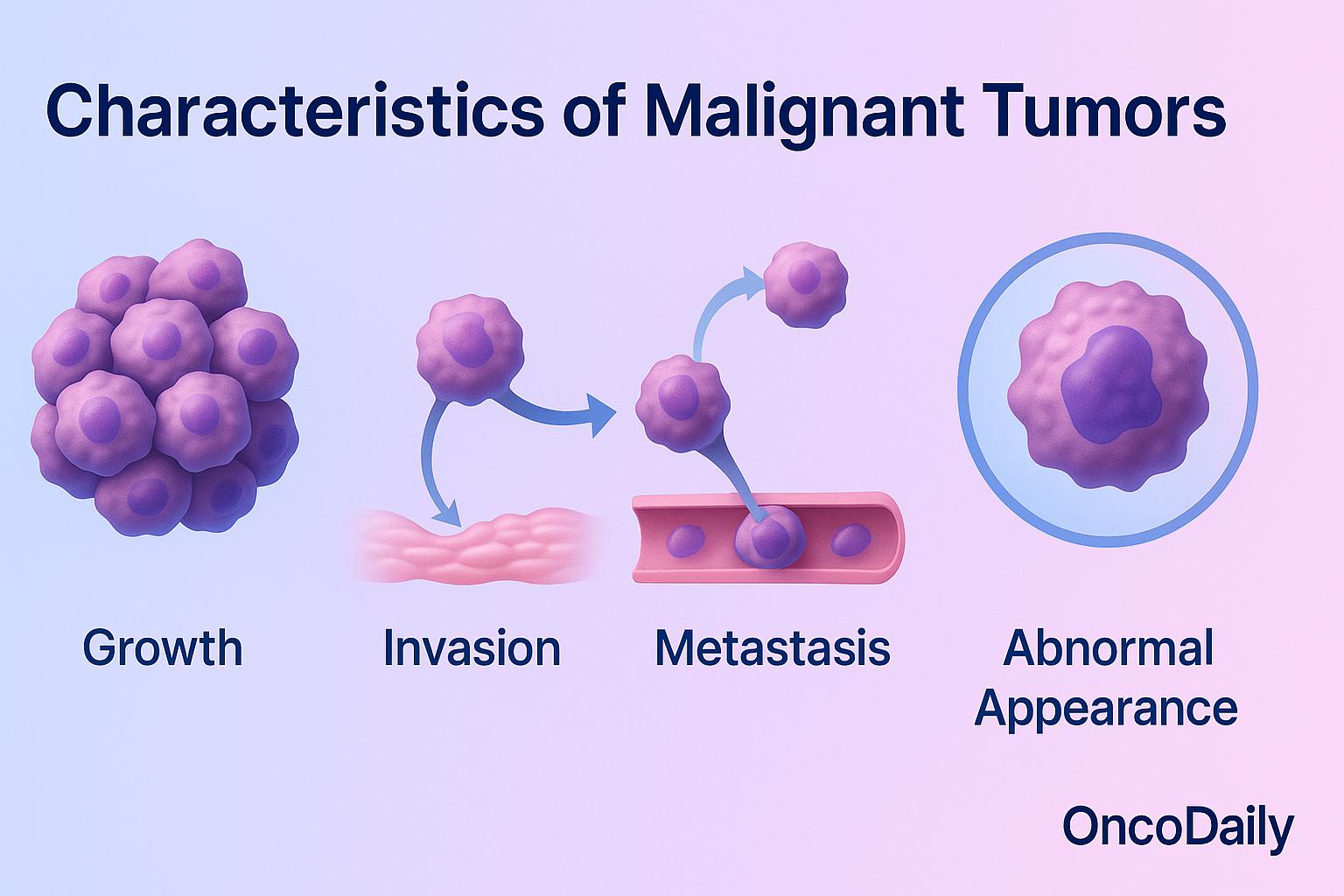
Malignant tumors are defined by several hallmark characteristics that distinguish them from normal or benign tissue. One of the key features is uncontrolled growth. Unlike healthy cells, which only divide when necessary and under strict regulatory controls, cancer cells ignore the normal signals that tell cells when to grow and when to stop. They continue dividing even when new cells are not needed, leading to the accumulation of abnormal tissue.
Another hallmark is invasion. Malignant cells are able to break through the boundaries of their tissue of origin and penetrate into nearby healthy tissues. They produce enzymes that degrade the surrounding structures, allowing them to infiltrate and disrupt normal organs and systems. Perhaps the most dangerous characteristic is metastasis. Malignant cells can enter blood vessels or lymphatic channels, travel through the circulation, and establish new tumors in distant parts of the body such as the lungs, liver, brain, or bones. Metastatic spread is what makes cancer so difficult to treat and is a major cause of cancer-related death.
Under a microscope, malignant cells often show an abnormal appearance. They tend to be high-grade and poorly differentiated, meaning they look very different from the healthy cells they originated from. Their nuclei are often larger, irregularly shaped, and stain more darkly, reflecting their aggressive and disorganized behavior. These features—uncontrolled growth, invasion, metastasis, and abnormal cellular appearance—are what define malignancy and underscore why early detection and aggressive treatment are so critical.
Common Types of Malignant Tumors
There are several major categories of malignant tumors, each named according to the type of tissue or cells from which they originate. Carcinomas are the most common type of cancer. They arise from epithelial cells, which are the cells that line the surfaces of the body, including the skin, glands, and the lining of internal organs. Examples of carcinomas include breast cancer, lung cancer, and colon cancer. Carcinomas tend to grow and spread through lymphatic channels, and many solid tumors in adults fall into this group.
Sarcomas are less common and develop from the body’s connective tissues, such as bone, muscle, fat, and cartilage. Examples include osteosarcoma (bone cancer) and leiomyosarcoma (cancer of smooth muscle). Sarcomas usually spread through the bloodstream rather than the lymphatic system. Leukemias are cancers of the blood-forming tissues, primarily affecting the bone marrow and blood cells. Instead of forming solid tumors, leukemia cells circulate in the blood and can affect the production of normal blood cells, leading to anemia, infection, and bleeding problems. Acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML) are common examples.
Lymphomas are cancers that begin in the lymphatic system, which is part of the body’s immune defense network. Lymphomas typically start in lymph nodes but can spread to other organs. The two main types are Hodgkin lymphomaand non-Hodgkin lymphoma. Other notable examples of malignant tumors include melanoma, a highly aggressive skin cancer arising from pigment-producing cells (melanocytes), and glioblastoma, an aggressive and often deadly brain cancer that originates from glial cells in the central nervous system.
Each type of malignancy behaves differently, grows at its own pace, and responds differently to treatment—making accurate diagnosis critical for planning effective therapy.
How Malignancy Is Diagnosed
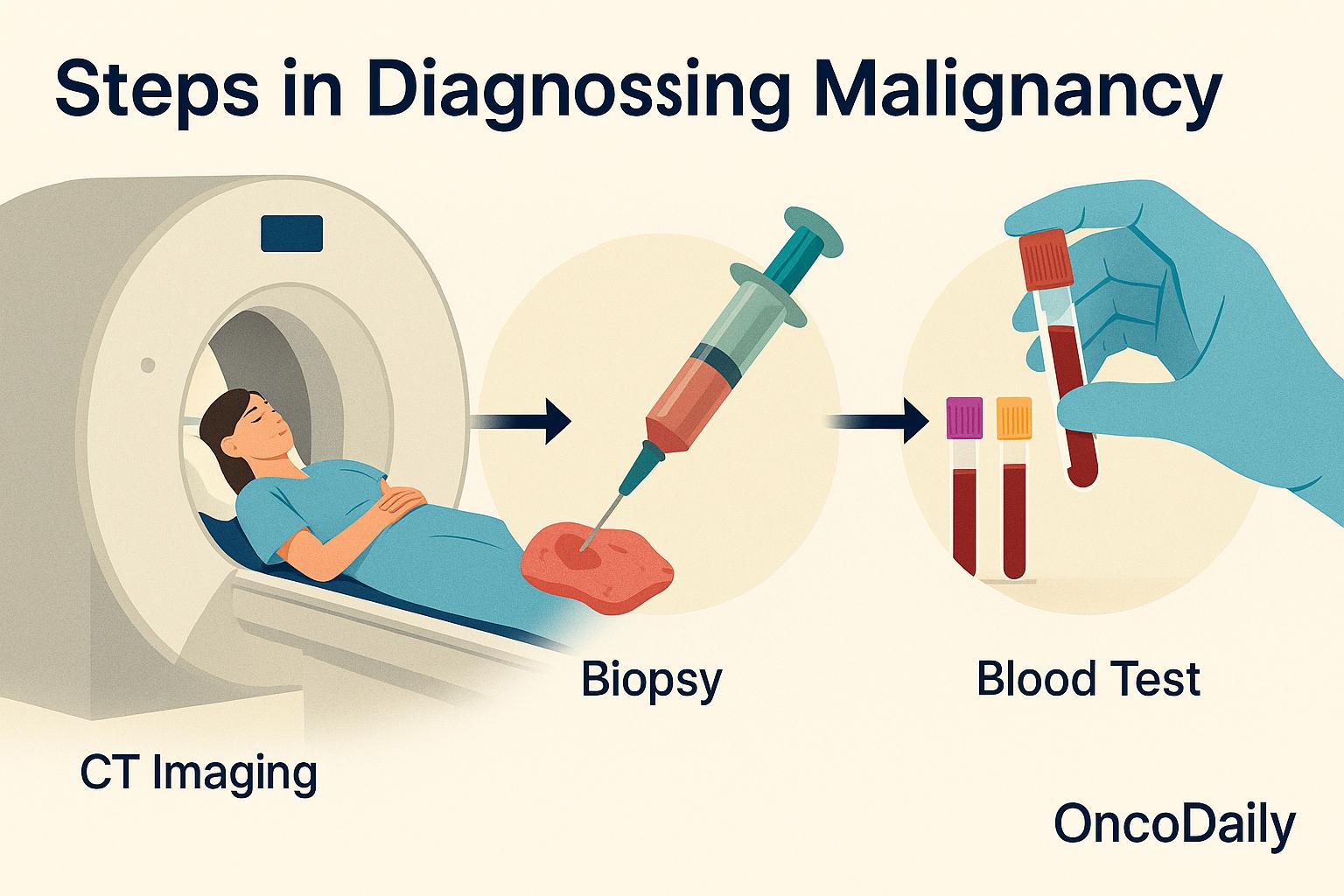
Diagnosing malignancy involves several important steps designed to confirm the presence of cancer, identify its type, and understand how far it has progressed. No single test is enough on its own—doctors use a combination of methods to get a complete picture.
A biopsy remains the gold standard for diagnosing malignancy. In a biopsy, a small sample of tissue is removed from the suspected tumor and examined under a microscope by a pathologist. This allows specialists to confirm whether cancer cells are present, determine the type of cancer, and evaluate specific features such as how abnormal (or aggressive) the cells appear.
Imaging studies are essential tools in both diagnosing and staging malignancies. Techniques like CT (computed tomography) scans, MRI (magnetic resonance imaging), and PET (positron emission tomography) scans allow doctors to visualize the location, size, and spread of tumors inside the body. Imaging helps identify whether the cancer is confined to one area or has spread to lymph nodes or distant organs (metastasis).
Blood tests can also provide valuable information. Certain blood markers, called tumor markers, can sometimes suggest the presence of cancer, although they are rarely definitive by themselves. For example, elevated PSA levels may suggest prostate cancer, while CA-125 levels might point to ovarian cancer. Blood tests can also detect anemia, liver function abnormalities, or high calcium levels, all of which can be indirect signs of cancer.
An essential piece of the diagnostic process is the pathology report generated after biopsy analysis. This report not only confirms malignancy but also evaluates critical features such as the tumor’s grade (how abnormal the cancer cells look under the microscope) and stage (how far the cancer has spread). Grade gives insight into how aggressive the cancer might be, while stage helps predict prognosis and guides treatment decisions.
Treatment Options for Malignant Tumors
The treatment of malignant tumors typically involves a combination of different approaches, tailored to the specific type of cancer, its stage, its location, and the overall health of the patient.
- Surgery is often the first line of treatment when the tumor can be safely removed. The goal is to physically extract the cancerous mass, sometimes along with surrounding tissues or lymph nodes, to reduce the risk of spread. Surgery can be curative if the cancer is detected early and has not metastasized.
- Radiation therapy uses high-energy rays to destroy cancer cells or shrink tumors. It can be used alone or alongside surgery and chemotherapy. Radiation is often employed after surgery to kill any remaining cancer cells or, in some cases, as a primary treatment when surgery is not possible.
- Chemotherapy involves the use of powerful drugs that kill rapidly dividing cells, including cancer cells. Chemotherapy can be used before surgery (neoadjuvant therapy) to shrink a tumor, after surgery (adjuvant therapy) to eliminate microscopic disease, or as the main treatment for cancers that have spread widely throughout the body.
- Immunotherapy is a newer approach that stimulates the body’s own immune system to recognize and attack cancer cells more effectively. Drugs like checkpoint inhibitors have revolutionized the treatment of certain malignancies, including melanoma, lung cancer, and some types of bladder cancer.
- Targeted therapy focuses on specific genetic changes or molecular markers found in cancer cells. Unlike chemotherapy, which affects both healthy and cancerous cells, targeted therapies aim to block the growth signals that cancer cells depend on, leading to fewer side effects and more precise action. Examples include HER2-targeted drugs in breast cancer and EGFR inhibitors in lung cancer.
The exact combination and sequence of these treatments depend heavily on multiple factors, including the type of cancer, how advanced (staged) it is, where it is located in the body, how aggressive it appears to be, and the patient’s overall health and ability to tolerate treatments. Personalized treatment planning is essential to achieving the best possible outcomes.
The Prognosis of Malignancy
The prognosis for a malignant tumor—the likely course and outcome of the disease—depends on several important factors. One of the most critical factors is the type of tumor. Some cancers, such as early-stage breast cancer or certain types of testicular cancer, are highly treatable and often curable with modern therapies. Others, like pancreatic cancer or glioblastoma, tend to be more aggressive and harder to control, even with advanced treatments.
The stage at diagnosis plays a major role as well. Cancers that are caught early, before they have spread beyond their original site, are generally associated with much better outcomes. In contrast, cancers diagnosed at a late stage, after metastasis to other organs, are usually more challenging to treat successfully.
Treatment response is another important consideration. Some tumors shrink dramatically in response to chemotherapy, radiation, or targeted therapies, while others may resist multiple lines of treatment. How well a tumor responds to initial therapy often predicts the chances of long-term control or cure. Additionally, molecular characteristics of the cancer—such as specific gene mutations, hormone receptor status, or protein expressions—can significantly affect prognosis.
For example, breast cancers that are HER2-positive can now be treated very effectively with targeted HER2 therapies, dramatically improving survival rates. Importantly, early detection often leads to better outcomes. When malignancies are found early, before extensive spread or severe symptoms develop, patients have a wider range of effective treatment options and a greater chance of achieving remission or cure.
You Can Watch More on OncoDaily Youtube TV
Written by Toma Oganezova, MD
FAQ
What is a malignant tumor?
A malignant tumor is made up of cancer cells that grow uncontrollably, invade nearby tissues, and can spread (metastasize) to distant parts of the body.
How do malignant tumors develop?
They develop when normal cells acquire mutations that disrupt growth control, allowing them to divide uncontrollably and avoid normal cell death.
What are key features of malignant tumors?
Uncontrolled growth, invasion into surrounding tissues, ability to metastasize, and abnormal cell appearance under a microscope.
What are the common types of malignant tumors?
Carcinomas, sarcomas, leukemias, lymphomas, melanomas, and glioblastomas are all types of malignant tumors.
How is malignancy diagnosed?
Diagnosis involves biopsy, imaging tests like CT or MRI, blood tests for tumor markers, and pathology analysis.
What treatments are available for malignant tumors?
Treatment options include surgery, chemotherapy, radiation therapy, immunotherapy, and targeted therapies.
Can malignant tumors be cured?
Some malignant tumors are highly treatable and curable if detected early, while others can be more aggressive and challenging.
What affects the prognosis of a malignant tumor?
Tumor type, stage at diagnosis, treatment response, molecular features, and overall patient health impact prognosis.
How do malignant tumors spread?
They spread by invading nearby tissues and traveling through blood vessels or lymphatic channels to distant organs.
Why is early detection of malignant tumors important?
Early detection often leads to more treatment options, better chances of cure, and improved survival rates.