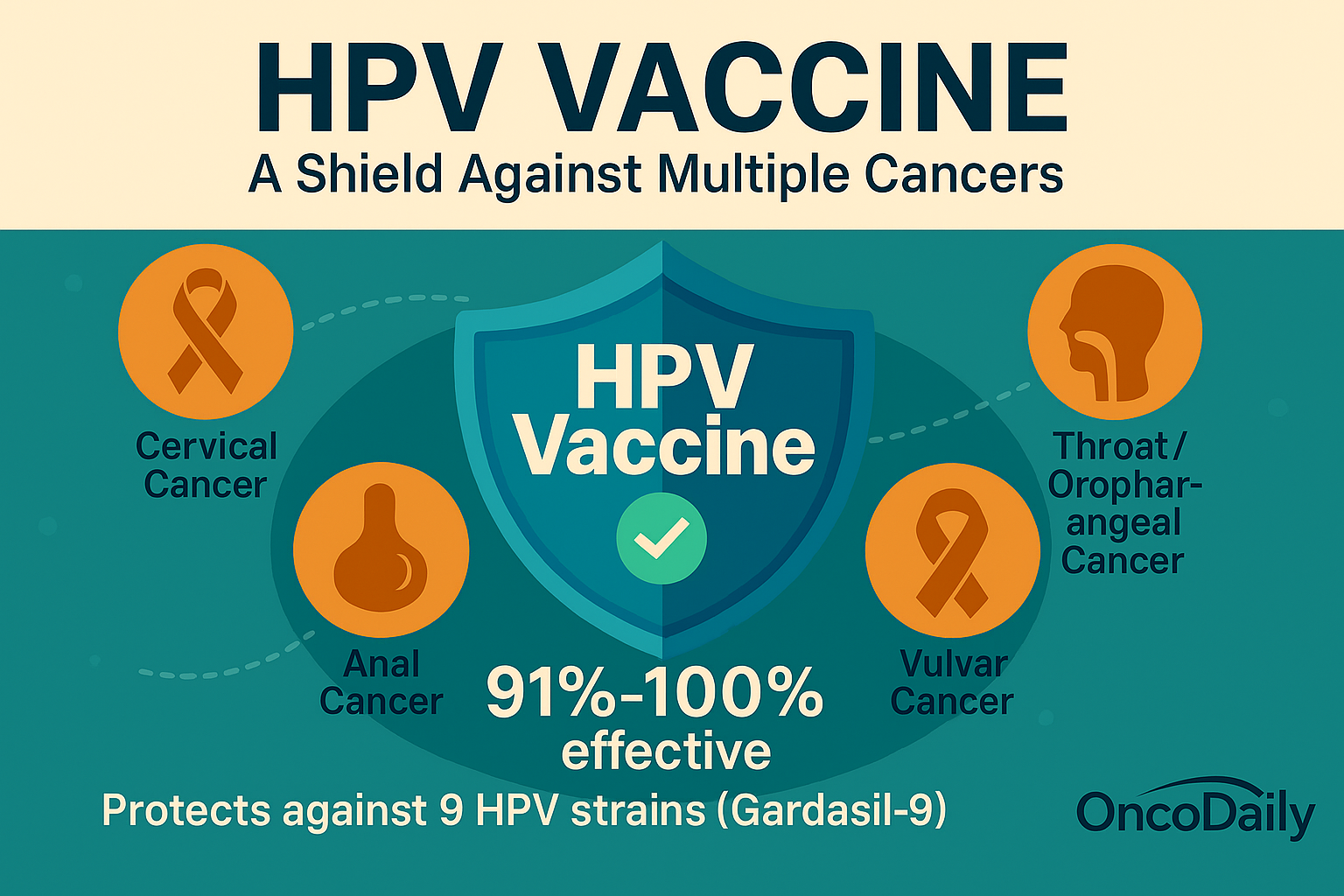
Vaccination is one of the most important public health achievements, preventing diseases that once caused millions of deaths. The HPV vaccine stands out for its ability to prevent several cancers caused by high-risk HPV strains, including cervical, anal, and oropharyngeal cancers. Since the introduction of Gardasil-9 in 2017, which protects against nine HPV strains, the vaccine has shown 91% to 100% effectiveness in preventing infections and precancerous lesions in young women under 26.
Photo: Depositphotos
Globally, about 47 million women had received the full HPV vaccine course by 2015. Despite this progress, vaccination rates remain below ideal in many countries. In the United States, only 58.6% of adolescents aged 13-15 were fully vaccinated by 2022, with slightly higher rates in females (60.7%) than males (56.6%). Large-scale studies involving over 3.4 million people confirm that HPV vaccination significantly reduces the risk of HPV-related cancers.
This article draws on trusted sources such as the Cleveland Clinic, CDC data, global vaccination reports, and recent research presented at the 2024 ASCO Annual Meeting. It highlights the vaccine’s critical role in cancer prevention and emphasizes the need to increase awareness and access to HPV vaccination worldwide.
HPV: A Silent Threat
HPV is a common virus transmitted through skin-to-skin contact, including sexual activity. While most infections resolve on their own, certain high-risk strains can cause cancer in both men and women. HPV is responsible for nearly all cases of cervical cancer, as well as significant proportions of cancers of the anus, penis, vulva, vagina, and oropharynx (throat and mouth). Globally, HPV causes hundreds of thousands of cancer cases and deaths each year.
How Life-Saving Is the HPV Vaccine?
What if a simple vaccine could protect you from several deadly cancers? The HPV vaccine does exactly that. Human papillomavirus (HPV) is a common virus that, if left unchecked, can cause cancers like cervical, anal, and throat cancer. According to data from the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC), the HPV vaccine can prevent up to 90% of these cancers. In countries like England, where the vaccine has been widely implemented, public health data show a 90% reduction in cervical cancer cases among young women. Experts from the UK’s National Health Service (NHS) are optimistic that with continued vaccination efforts, cervical cancer could become extremely rare or even eliminated in the near future.
The Science Behind the Protection
This isn’t just hopeful thinking, it’s backed by solid research. A landmark study published in The New England Journal of Medicine in 2020 analyzed health records of nearly 3.5 million people in Sweden over 10 years. The study found that those vaccinated against HPV had significantly lower rates of HPV-related cancers compared to unvaccinated individuals. This protective effect was observed in both women and men, with vaccinated men showing a reduced risk of head and neck cancers. These findings reinforce the message from the CDC and WHO that HPV vaccination is one of the most effective ways to prevent certain cancers.
Who Should Get Vaccinated?
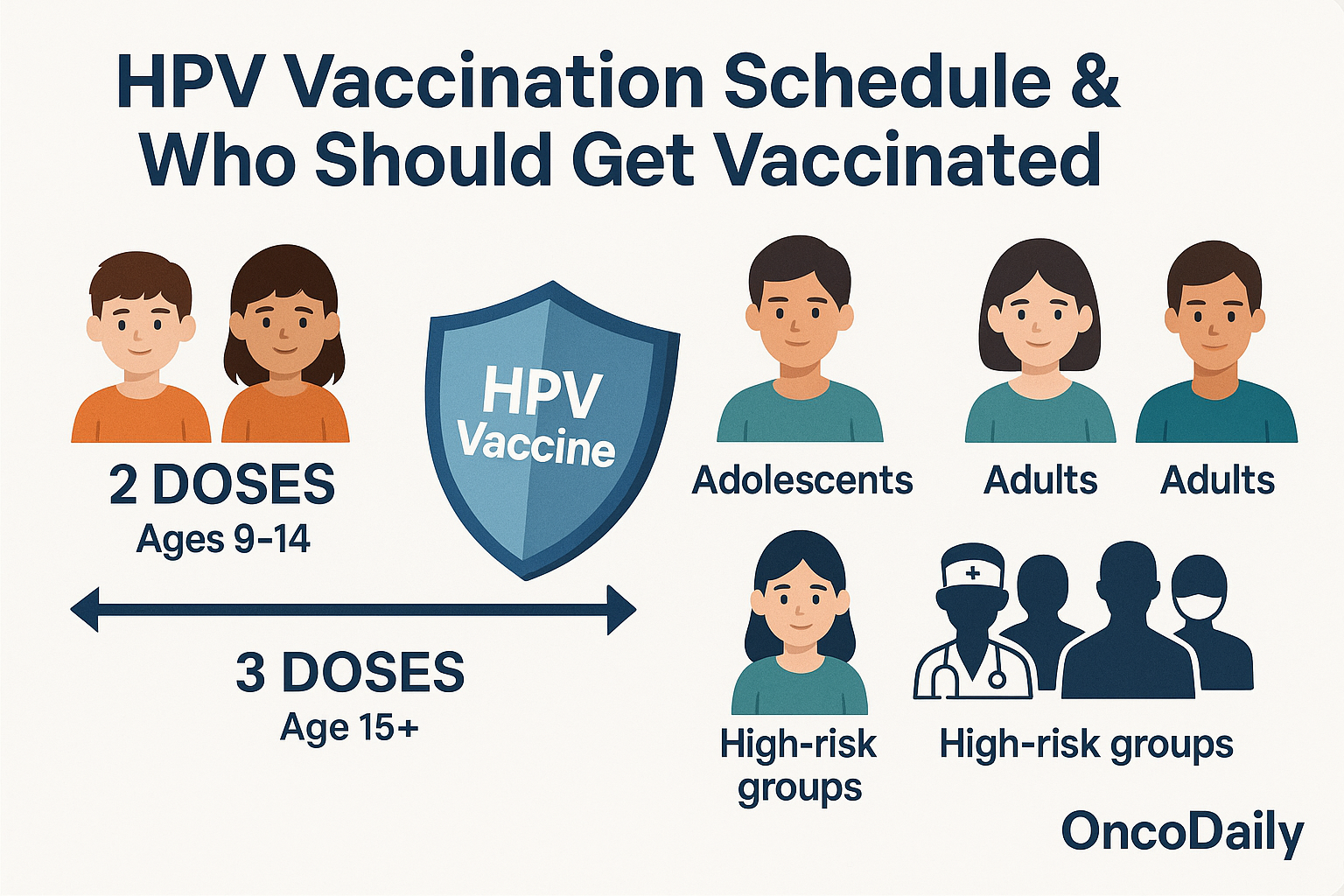
Health authorities, including the CDC and WHO, recommend the HPV vaccine for everyone aged 9 to 26, with catch-up vaccination available up to age 45. The vaccine works best when given before any exposure to HPV, which is why it’s routinely offered to preteens around ages 11 or 12. However, adults can still benefit from vaccination, as supported by ongoing clinical studies.
Vaccination is especially important for certain groups, including healthcare workers who may have increased exposure to HPV, individuals with multiple sexual partners or those entering new sexual relationships, men who have sex with men (MSM), and immunocompromised individuals such as those living with HIV. These groups are at higher risk of HPV infection and related diseases and should strongly consider vaccination even if they are older than the routine age range.
Regarding the vaccination schedule, the HPV vaccine is typically administered as a series of two or three doses depending on age:
- For individuals aged 9 to 14 years, two doses are recommended, spaced 6 to 12 months apart. The second dose is necessary to complete the vaccination series and ensure full protection.
- For individuals aged 15 years and older, including adults up to 45, three doses are recommended: the second dose is given 1 to 2 months after the first, and the third dose 6 months after the first. Completing all doses is critical for optimal immunity.
In summary, anyone starting the HPV vaccine series must receive the second dose at the recommended interval, and those in higher-risk occupations or groups should consider vaccination regardless of age to reduce their risk of HPV-related diseases.
Fewer Shots, More Protection
Recent research, including a 2022 study published in The Lancet, suggests that even a single dose of the HPV vaccine may provide protection equivalent to the traditional two-dose schedule. This finding could simplify vaccination programs and increase coverage, especially in low- and middle-income countries where access to healthcare is limited.
Can the HPV Vaccine Prevent Other HPV-Related Cancers?
While most people associate HPV with cervical cancer, data from the CDC show that HPV also causes other cancers affecting both men and women, including cancers of the throat, anus, vulva, and penis. This broad protection underscores the importance of vaccinating all eligible individuals, regardless of gender.
Overcoming Barriers to Protection
Despite overwhelming evidence and endorsements from global health organizations, HPV vaccination rates remain below target levels in many regions. According to the WHO’s 2024 global vaccine coverage report, misinformation, stigma, and limited access continue to leave millions vulnerable to preventable HPV-related cancers. Public health campaigns and improved healthcare infrastructure are essential to increase vaccine uptake worldwide.
“HPV vaccination is cancer prevention. Preventing cancer is better than treating it.”
— U.S. Centers for Disease Control and Prevention
In Conclusion
The HPV vaccine is not just a shot it’s a powerful shield against some of the deadliest cancers. Supported by extensive data from global health agencies and large-scale studies, vaccination offers a proven way to save lives. By getting vaccinated and encouraging others to do the same, we can move closer to a future where HPV-related cancers are rare or even eliminated.
Written by Marine Marashlian
FAQ
Can the HPV vaccine cause HPV infection or cancer?
No. The HPV vaccine contains no live virus, so it cannot cause HPV infection or any type of cancer.
Who should get the HPV vaccine and at what age?
The vaccine is recommended for everyone aged 9 to 26, with catch-up vaccination available up to age 45. It is most effective when given before exposure to HPV, which is why preteens are routinely vaccinated.
If I already have HPV, should I still get vaccinated?
Yes. The vaccine does not treat existing HPV infections but protects against other HPV types you have not yet been exposed to.
How many doses of the HPV vaccine are needed?
For ages 9 to 14, two doses spaced 6 to 12 months apart are recommended. For those 15 and older, three doses over six months are advised. Recent studies suggest one dose may offer strong protection, but completing the series is best. For ages 9 to 14, two doses spaced 6 to 12 months apart are recommended. For those 15 and older, three doses over six months are advised. Recent studies suggest one dose may offer strong protection, but completing the series is best.
Do I still need regular cervical cancer screening after vaccination?
Yes. The vaccine does not protect against all cancer-causing HPV types, so regular Pap tests or HPV screening remain essential.
Does the HPV vaccine cause infertility?
No. There is no evidence that the HPV vaccine causes infertility. In fact, by preventing cervical cancer, it may help preserve fertility.
Is the HPV vaccine safe?
Yes. The HPV vaccine is safe with mostly mild side effects like pain or redness at the injection site. Serious side effects are extremely rare and not causally linked to the vaccine.
Can pregnant women get the HPV vaccine?
Pregnant women are advised to avoid the HPV vaccine due to limited safety data during pregnancy.
What types of cancers does the HPV vaccine prevent?
The vaccine protects against cervical, vaginal, vulvar, penile, anal, and oropharyngeal (throat) cancers caused by HPV.
Can the HPV vaccine cause fainting?
Fainting can occur after any vaccination, especially in teens, but it is not caused by the vaccine itself. Recipients are advised to remain seated for 15 minutes after vaccination.