At the MASCC 2025 Annual Meeting, Dr. Moran Amit of MD Anderson Cancer Center and UTHealth Graduate School of Biomedical Sciences delivered a forward-looking presentation on the evolving role of drug repurposing in cancer supportive care, with a focus on the neural-tumor microenvironment and how it shapes both biological outcomes and quality of life for patients.

Introduction to Drug Repurposing in Oncology
Drug repurposing—the practice of applying existing, clinically approved medications to new indications—has gained traction as a faster, cost-effective strategy compared to traditional drug development. While new drug development often exceeds $1–2 billion and takes over a decade, repurposed drugs benefit from established safety profiles and expedited regulatory pathways. This strategy is particularly relevant to cancer supportive care, where patient needs around symptom control, mental health, and functional outcomes remain largely unmet.
Despite progress in oncology therapeutics, only 24% of new cancer drugs are associated with improved quality of life. Addressing this gap requires novel approaches, including leveraging already-approved agents for supportive interventions.
The Case for Targeting the Neural-Tumor Microenvironment
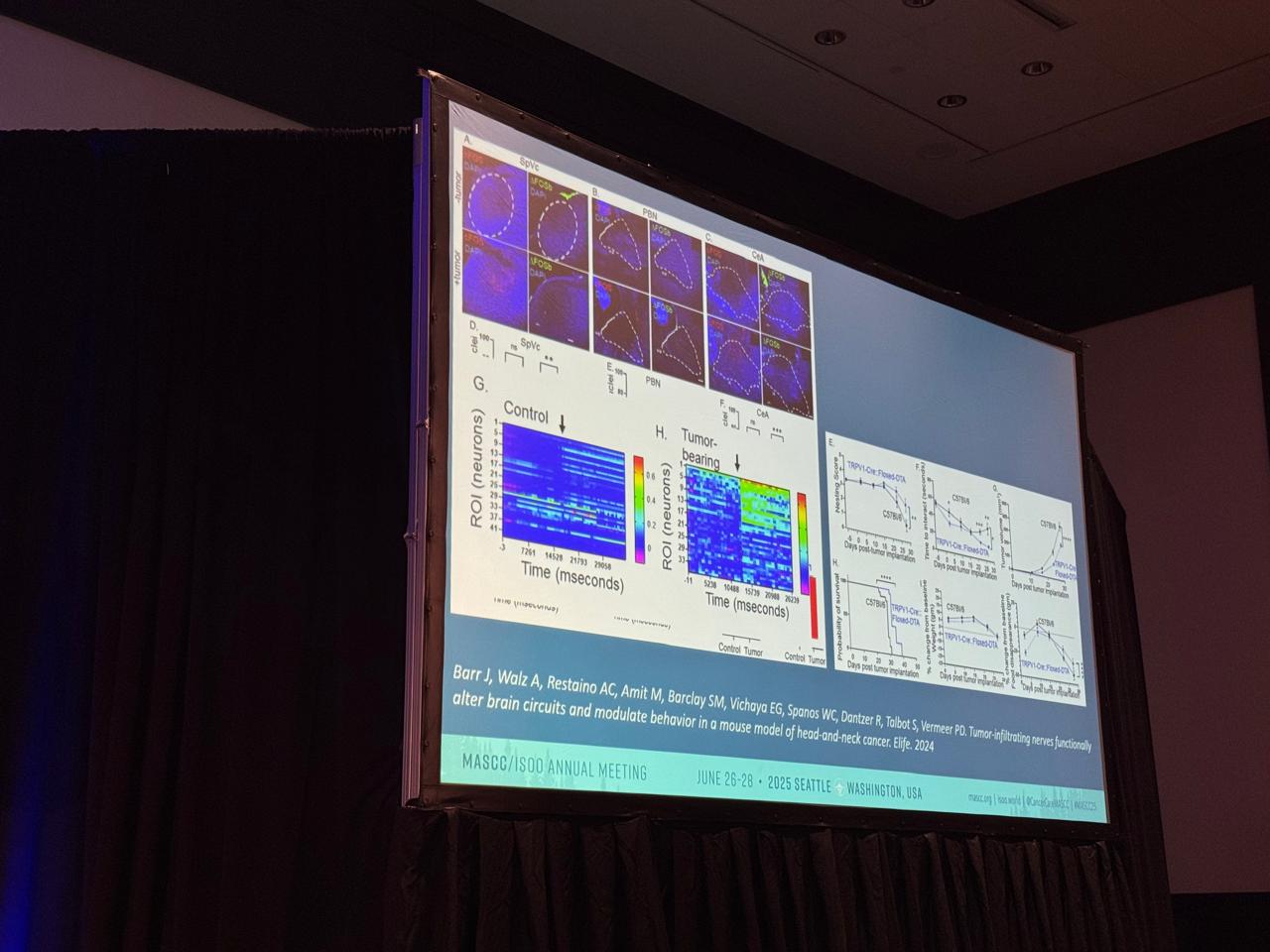
A major highlight of Dr. Amit’s talk was the growing evidence that tumor-infiltrating nerves form direct circuits with the brain, influencing both tumor biology and patient behavior. This insight opens a new frontier: using neuroscience-informed strategies to address cancer symptoms and treatment side effects.
The neural-tumor interface, including neuro-immune crosstalk and neurotransmitter signaling, may be particularly relevant to quality-of-life domains such as pain, anxiety, fatigue, and swallowing dysfunction. It also offers new drug targets ripe for repurposing.
Key Drug Classes and Mechanisms for Repurposing
Dr. Amit outlined several drug categories with high potential for repurposing:
Beta-blockers (e.g., propranolol): Traditionally used in cardiology, these inhibit adrenergic stress signaling, modulating immune response and perioperative tumor progression.
- CGRP receptor antagonists (e.g., rimegepant): Approved for migraines, these may modulate sensory nerves in the tumor microenvironment. In head and neck cancer, CGRP-positive nerves correlate with poor swallowing outcomes, suggesting a role for these drugs in preserving swallowing function.
- Cholinergic and GABAergic modulators: Used in neurological and psychiatric settings, these influence immune signaling and neural circuit function.
- Antidiabetic agents: By targeting metabolic pathways, some of these agents may modulate cancer metabolism or indirectly affect neural-tumor interactions.
Clinical Evidence and Opportunities
Multiple clinical trials are underway to evaluate repurposed drugs in oncology. Notably, beta-blockers have shown potential to improve progression-free survival, reduce perioperative stress, and enhance response to immunotherapy. Meanwhile, CGRP antagonists are being studied for their ability to modulate the tumor sensory nerve landscape and improve patient-reported outcomes.
Evidence from human studies is growing. Improvements in quality of life, particularly around function and symptom relief, are increasingly documented, especially in head and neck cancer populations where neural modulation may directly impact swallowing and speech.
Challenges in Implementation
Despite the promise, Dr. Amit outlined key barriers:
- Regulatory complexity: The 505(b)(2) pathway for repurposed drugs is slower and more restrictive than expected.
- Lack of industry incentive: Patent expiration reduces commercial interest.
- Funding constraints: Academic trials in supportive care are underfunded.
- Heterogeneity: Variability in patient populations complicates stratification and biomarker discovery.
- Clinical trial design: Long-term safety, combination strategies, and predictive biomarkers remain areas of active development.
Future Directions and Research Priorities
To unlock the full potential of drug repurposing in supportive care, future efforts should prioritize:
- AI-driven drug identification
- Biomarker-driven patient selection
- Survivorship-focused endpoints
- Neural-circuit–based precision medicine
- Cost-effectiveness and health economics evaluations
Integration of these elements can help move promising agents into clinical practice faster and more effectively.
Conclusion
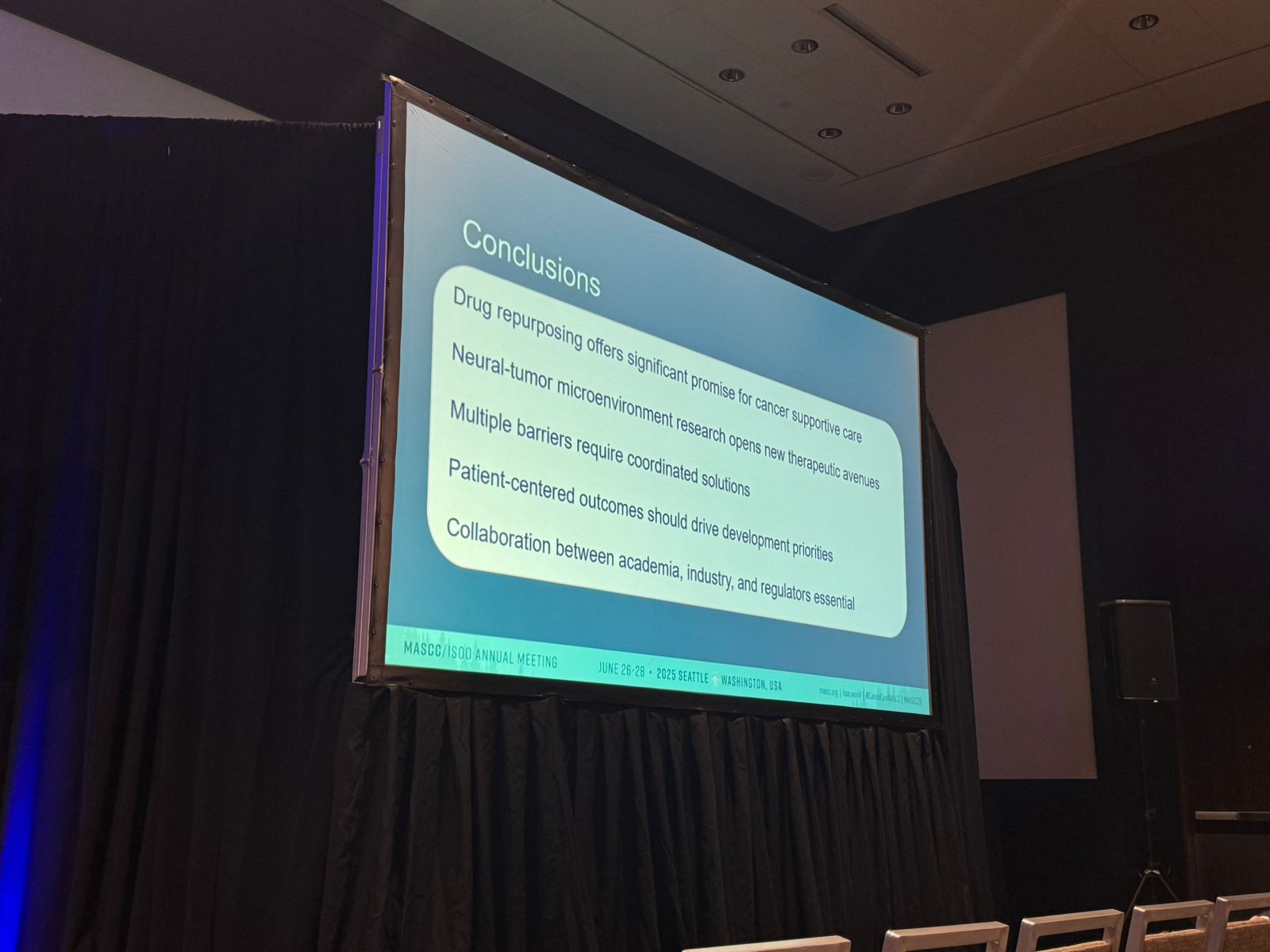
Dr. Amit’s presentation at MASCC 2025 underscored the untapped therapeutic potential of drug repurposing in cancer supportive care. By aligning advances in neuro-oncology, immunology, and pharmacology, and addressing structural barriers, the field can move toward a more patient-centered, quality-of-life–driven approach to cancer care.